
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
Tigecycline reduced tumor necrosis factor alpha level and inhospital mortality in spontaneous supratentorial intracerebral hemorrhage
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v25i2.1351 Med J Indones. 2016;25:69–75
Received: January 08, 2016
Accepted: May 23, 2016
Author affiliation:
1 Department of Neurosurgery, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
2 Department of Neurology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
3 Department of Pediatric, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
4 Clinical Epidemiology and Evidence-Based Medicine, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Corresponding author:
Mohamad Saekhu
E-mail: saekhu2010@hotmail.com
Background
The outcome of patients with spontaneous supratentorial intracerebral hemorrhage (SSICH) is unsatisfactory. Inflammatory response secondary to brain injury as well as those resulted from surgical procedure were considered responsible of this outcome. This study was intended to elucidate the anti-inflammatory activity of tigecycline by measuring TNF-α level and its neuroprotective effect as represented by inhospital mortality rate.
Methods
Patients with SSICH who were prepared for hematoma evacuation were randomized to receive either tigecycline (n=35) or fosfomycine (n=37) as prophylactic antibiotic. TNF-α level was measured in all subjects before surgery and postoperatively on day-1 and day-7. A repeated brain CT Scan was performed on postoperative day-7. The Glasgow outcome scale (GOS) and length of stay (LOS) were recorded at the time of hospital discharge. Data were analyzed using Mann-Whitney and Chi square test. Relative clinical effectiveness was measured by calculating the number needed to treat (NNT).
Results
There was a significant difference regarding the proportion of subject who had reduced TNF-α level on postoperative day-7 between the groups receiving tigecycline and fosfomycine (62% vs 29%, p=0.022). Decrease brain edema on CT control (86% vs 80%, p=0.580). Tigecycline administration showed a tendency of better clinical effectiveness in lowering inhospital mortality (17% vs 35%; p=0.083; OR=0.49; NNT=5) and worse clinical outcome / GOS ≤ 2 (20% vs 38% ; p=0.096; OR=0.41; NNT=6). LOS ≥ 15 hari ( 40% vs 27%; p=0.243; OR=1.81; NNT=8).
Conclusion
Tigecycline showed anti-inflammatory and neuroprotective activities. These activities were associated with improved clinical outcome in patients with SSICH after hematoma evacuation.
Keywords
inhospital mortality, SSIH, tigecycline, TNF-α
The mortality rate at day-7 post-spontaneous supratentorial intracerebral hemorrhage (SSICH) reaches 34.6%, and becomes 50.3% in the first month of treatment.1 Unfortunately, patients who can survive will suffer neurological disabilities with poor quality of life.2 Referring to a population-based study in the United States, the inhospital mortality for SSICH patients undergoing hematoma evacuation is 27.2%, and those without hematoma evacuation is 32%.3 Among the causes of unsatisfactory clinical outcome, is secondary brain injury as the consequence of untreated inflammatory response,4 as well as additional injury/inflammation due to surgical procedure5 that can lower the benefit of hematoma evacuation.6 Until now, SSICH management is still considered unsatisfactory.4,7
Considering that inflammation has pivotal role in the development of brain injury, controlling inflammatory response would be one of the promising treatment in SSICH management.8 However, administration of steroidal antiinflammatory drugs is proven ineffective, as well as increased infection as its complication.9 Animal studies have shown anti-inflammatory and neuroprotective activities of tetracycline derivatives.10,11 Among several inflammatory markers, tumor necrosis factor–alpha (TNF-α) has been known as a good marker of brain injury in SSICH patients.12,13 Low or reduced TNF-α level has been proven to be associated with better outcome of intracranial hemorrhage (ICH) in animal study14 as well as in human subjects.13,14 A new tetracycline derivative, tigecycline, reduces TNF-α level and shows neuroprotective activity in animal studies.15 However, anti-inflammatory and neuroprotective activities of tigecycline in SSICH patients has not been well studied. This study was aimed to evaluate whether tigecycline could reduce TNF-α level as well as reduce brain injury in human subject with SSICH who underwent hematoma evacuation.
METHODS
This was a randomized controlled trial (RCT) to elucidate the anti-inflammatory and neuroprotective activities of tigecycline in SSICH patients who underwent hematoma evacuation at 11 hospitals in Jakarta. Randomization was carried out by block system, with the size of four. Patients who were prepared for hematoma evacuation over a period of August 2012 to November 2014, were randomized to receive either 100 mg tigecycline or 2 g fosfomycine as prophylactic antibiotic. Antibiotic was administered intravenously 30 minutes before the surgery. The protocol of this study has been approved by Medical Ethics Committee, Faculty of Medicine, Universitas Indonesia/Cipto Mangunkusumo Hospital (No. 493/PT02.FK/ ETIK/2012).
SSICH diagnosis was made based on clinical condition and the results of CT scan imaging. Surgical intervention was indicated if the hematoma volume was ≥30 mL and the clinical finding showed a decreased level of consciousness. The volume was measured by following formula: ½ (A × B × C) with A as the greatest diameter of hematoma on CT scan, B as the vertical diameter (90°) to A, and C is the amount of slices on the CT scan by which the hematoma were seen (counted in centimeters).16 The surgical procedures were hematoma evacuation with craniotomy or craniectomy. Sample size was calculated by following formula:17

By taking P1=0.4 as the proportion of the effect of standard treatment, and P2=0.7 as proportion of the effect of tigecyclin, α=0.05 and β=0.1, a minimum of 22 subjects were needed in each group.
Subject characteristics and outcomes were recorded as numeric and/or categorical data. The subject characteristics were age, sex, Glasgow coma scale (GCS) score, hematoma volume and its mass effect, onset and duration of surgery, size of corticotomy, systemic factors which affected prognosis, as well as the plasma level of TNF-α before surgery. The outcomes of our study were TNF-α plasma level on postoperative day-1 and day-7, changes in brain edema level on CT scan, glasgow outcome scale (GOS) and length of stay (LOS) at the time of hospital discharge.
Brain edema level was measured by perihematoma hypodensity thickness on the CT scan before surgery and perihematoma hypodensity thickness/former hematoma area in milimetres. The changing level of edema was measured by comparing the degree of brain edema on CT scan pre-surgery with repeated CT scan at day seven post-surgery. The plasma level of TNF-α was measured using ELISA, the reagent for TNF-α is produced by DRG in the United States. Normal value of TNF-α according to the manual book is 4.5–12.5 pg/mL, by which the abnormal value of TNF-α was determined if it is more than 12.5 pg/mL. Data from all of the randomized subjects were included in the analysis. Numeric data were presented as mean value and data distribution, categorical data were presented as proportion (%). Comparison of numeric data between the two groups was done by using Mann–Whitney test, meanwhile categorical data were tested using Chi square test. The statistical level of significance was set at p˂0.05. Relative clinical effectiveness was calculated using relative risk (RR), odds ratio (OR), and number needed to treat (NNT).
RESULTS
The sample size of our study was 72 subjects, including 35 subjects in the treatment group (tigecycline) and 37 subjects in the control group (fosfomycine).
Subject characteristics
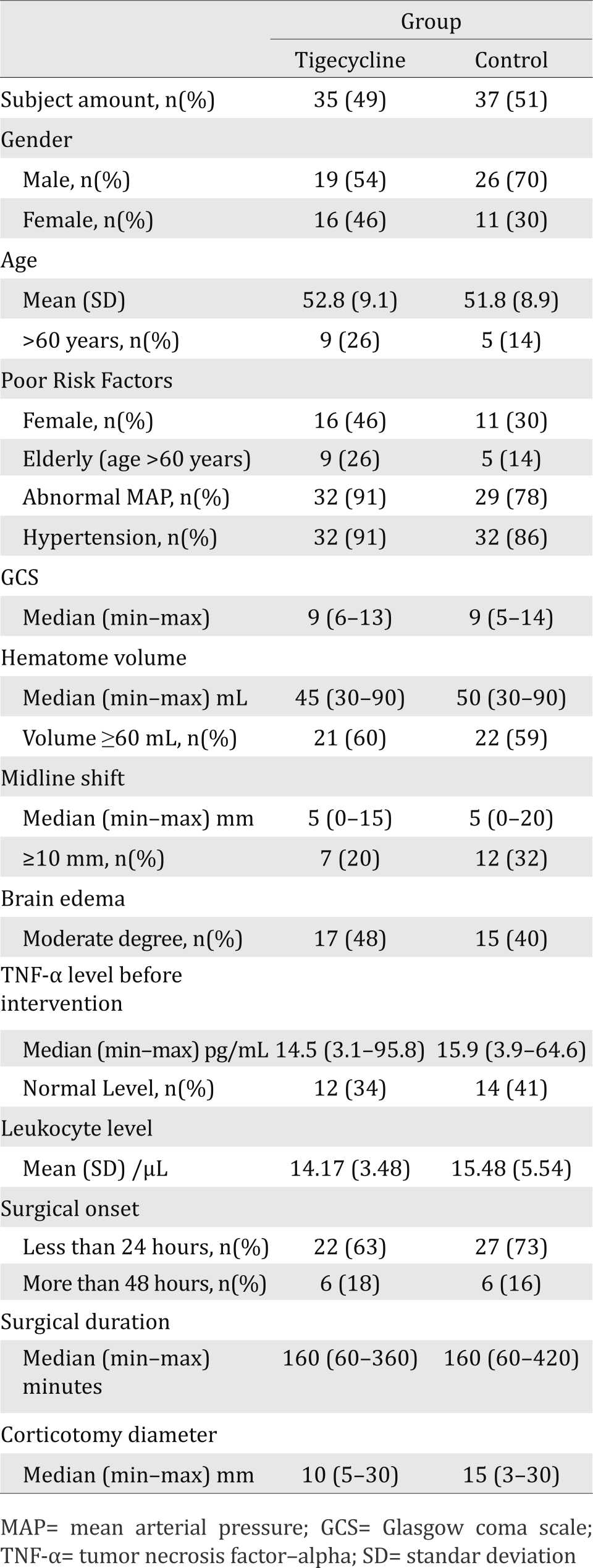
Age mean, GCS, and hematoma volume of subjects in both groups were equal. Risk factors for poor outcome such as elderly age (over 60 years), female, history of hypertension, and abnormal mean arterial pressure (MAP) were found greater in the tigecycline group. On the contrary, mid line shifting (MLS) of ≥10 mm, which is a sign of brain herniation, was greater in the fosfomycin group (Table 1).
Table 1. Subject characteristic
Changes of TNF-α plasma level
Changes of the TNF-α level were analyzed based on three aspects, i.e. mean value, proportion of subject with normal level, and with decreased level. Changes of brain edema were measured by comparing the degree of brain edema using CT scan figures before and after surgery. Changes of TNF-α plasma level are shown in Table 2.
Table 2. Changes of the TNF-α and brain edema
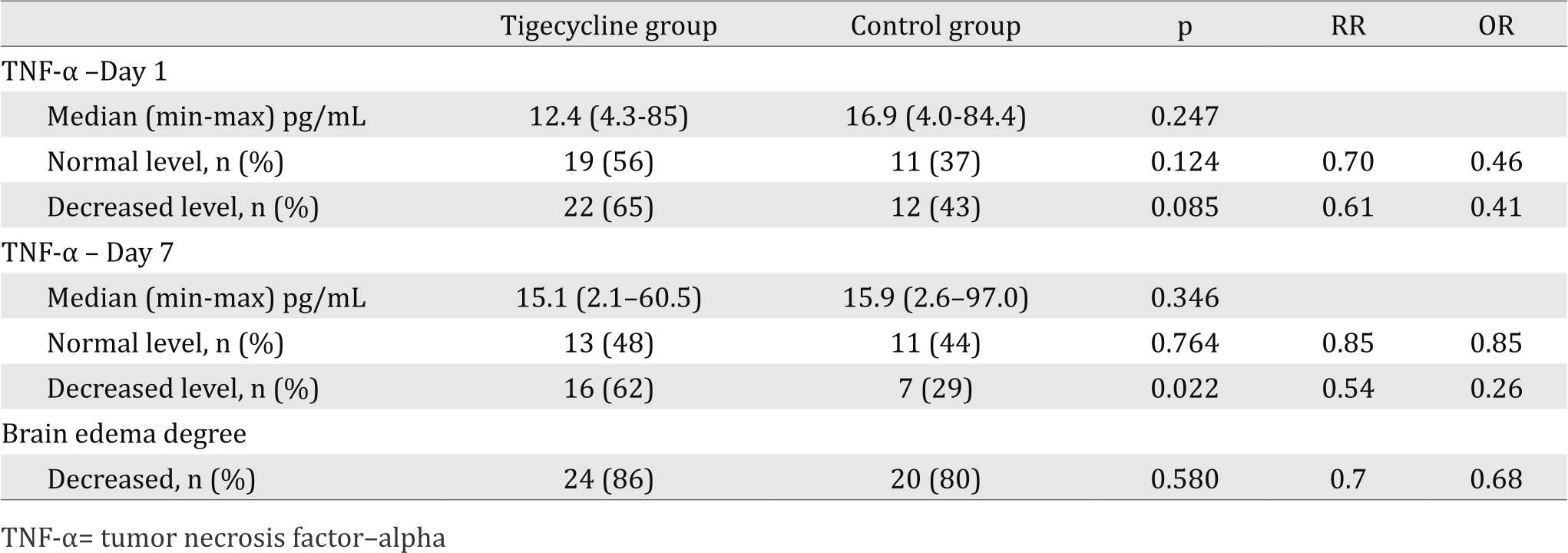
On post operative day one, TNF-α levels in the tigecycline group from all the three aspects were improved. Median was decreased from 14.5 (3.1–95.8) pg/mL to 12.4 (4.3–85.0) pg/mL, proportion of subjects with normal level of TNF-α was increased from 34% to 44%, and the proportion of subjects with decreased level was greater compared to the proportion of subjects having increased level (65% vs 35%). On the contrary, in the control group, median was increased from 15.93 (3.9–64.6) pg/mL, the proportion of subjects with normal level of TNF-α was decreased from 41% to 37%, and the proportion of subjects with decreased level was lower compared to the proportion of subjects having increased level (43% vs 57%). The changes of TNF-α level between the two group were statistically not significant. However, the data showed that the tigecycline reduced the TNF-α level, as well as the surgical procedure increased the TNF-α level.
On post operative day seven, the proportion of subjects with normal TNF-α level in the tigecycline group was increased from 34% (before tigecycline administration) to 48%. However, it was decreased compared to post operative day one from 56% to 48%. The proportion of subjects with normal TNF-α level in the control group was also increased from 41% (before fosfomycin administration) to 44% The differences of the proportion of normal level of TNF-α between the two group were statistically not significant (chi square resulted p=0.764 (95% CI=0.560-1.531). However, the differences of the proportion of subjects with reduced TNF-α level between the two group were statistically significant (62% vs 29%; p=0.022; 95% CI=0.313–0.941).
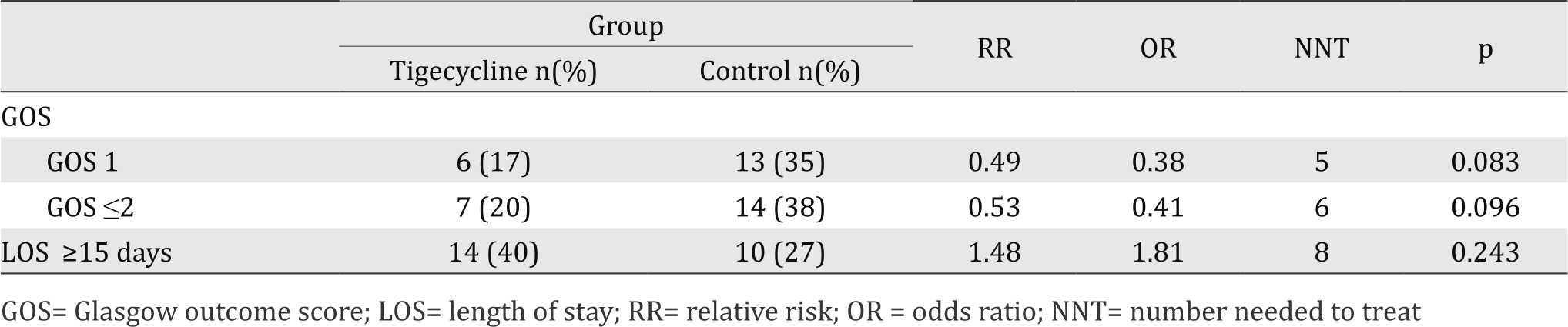
Short-term clinical outcome
Clinical outcomes were measured with GOS and LOS at the time of hospital discharge. GOS was quite applicable for measuring clinical outcome post spontaneous supratentorial intracerebral hemorrhage (SSIH), in spite of its rough characteristic. GOS consists of cognitive evaluation, disability, and social function.18 Therefore, GOS measurement at the time of hospital discharge is a prognostic marker for clinical outcome at six months.19 To present shortterm clinical outcome, the study also included LOS (Table 3).
Table 3. Glasgow outcome score and length of stay
DISCUSSION
Intracerebral hematoma causes mass effects in the form of increased intracranial pressure and brain herniation, as well as a source of neurotoxic substances that damage the brain cells. All causes may affect each other and lead to unsatisfactory clinical outcomes. A previous study showed that hematoma volume is a powerful predictor of the 30-day mortality rate.20 However, for most patients the usefulness of surgery is not well established. Hematoma evacuation can indeed reduce intracranial pressure and prevent brain herniation, as well as producing a significant amount of neurotoxic substances; however, the evacuation surgical procedure has been believed to cause additional brain injury.5,6
Surgical evacuation of hematoma for clinical deteriorating patients can be considered as a life-saving procedure.21 It seems that there is no particular type of treatment, either surgical or medical, that can provide satisfactory clinical outcomes. Recent advances from basic science and pre-clinical studies regarding treatment strategies for SSICH show the role of cell replacement therapy, endogenous neurogenesis, and neuroprotection.22 Neuroprotective agents were believed to provide brain cells protection from secondary brain injury that causes sustainable brain damage, as well as to improve neurological outcomes.23 On animal models, antiinflammatory drugs, as well as minocycline (the prototype of tigecycline), have been demonstrated to have neuroprotective activity and therapeutic effects.24,25 This study was intended to elucidate the anti-inflammatory activity of tigecycline by measuring TNF-α level, and its effects on clinical outcomes by measuring the inhospital mortality rate and/or GOS score.
The findings in the present study confirm that tigecycline reduced TNF-α plasma level. This study noted a significant difference on the proportion of subjects with reduced TNF-α plasma level on the seventh day after administration/surgery between those in the tigecycline and fosfomycine group. About 62% of subjects in the tigecycline group showed reduced TNF-α plasma level, while only 29% of subjects in the control (fosfomycine) group showed reduced TNF-α plasma level.
These results are similar with the results of previous studies conducted in animal,15 which indicate that tigecycline can reduce TNF-α plasma level. Since TNF-α is a proinflammatory cytokine,26 the reduced plasma level could be assumed as a reflection of less inflammation process. Inflammatory response plays an important role as a cause of brain injury, either due to SICH or surgical procedures.5,8 On the other hand, the nonsteroidal anti-inflammatory drugs (rosiglitazone) and tigecycline have been shown to reduce the inflammatory response.5,15
Reduced TNF-α level or activity,14,27 or moderate level of TNF-α13 is associated with better clinical outcomes in intracerebral hemorrhage. The results of present study are consistent with the statements above. Inhospital mortality rate was reduced by 18%, i.e. the tigecycline group has recorded inhospital mortality rate by 17%, compared with 35% in the control (fosfomycine) group. A population-based study in US showed that the inhospital mortality rate was 27.2%.28 Although statistically it was not significant, but it was clinically important. Subjects who received a single dose of 100 mg tigecycline would experience reduced risk of inhospital mortality by 2.6 times. In addition to the inhospital mortality rate, subjects in the tigecycline group also experienced better GOS score by 2.4 times.
This study protocol established a reexamination of CT scan on the seventh day after surgery. Considering that hematoma volume of more than 30 mL is associated with early death29 and most of the patients (89%) die before the seventh day, re-examination of the CT scan on the seventh day become one of the limitations in this study. Assesment on adequacy of hematotoma evacuation and/or the presence of rebleeding can not be done. Other limitations in this study include the small sample size (72 subjects), a slight difference in the facilities, especially in intersive care unit and wards that exist among the hospitals that had become the study site and a slight difference in surgical procedure performed by different neurosurgeons. Although there were limitations, several factors which were believed to affect the outcomes, i.e. age,30 gender,31 GCS on admission and volume of the hematomawere comparable in both groups.32,33
In conclusion, a single dose of 100 mg tigecycline treatment before surgical procedure for hematoma evacuation of SSICH can significantly reduce TNF-α plasma level. Tigecycline treatment also shows lower inhospital mortality rate, which is clinically important. Further studies are necessary to asses the effectiveness and efficiency of tigecycline treatment for ICH by considering various limitations found in this study.
Conflicts of Interest
The author affirms no conflict of interest in this study.
Acknowledgment
The author would like to thank all medical staffs of Department of Neurosurgery, Faculty of Medicine, Universitas Indonesia.
REFERENCES
- Sacco S, Marini C, Toni D, Oliveri L, Carolei A. Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke. 2009;40(2):394–9.
- Christensen MC, Mayer S, Ferran JM. Quality of life after intracerebral hemorrhage: result of the factor seven for acute hemorrhagic stroke (FAST) trial. Stroke. 2009;40(5):1677–82.
- Patil CG, Alexander AL, Gephart Gephart MG, Lad SP, Arrigo RT, Boakye M. A population-based study of inpatient outcomes after operative managemant of nontraumatic intracerebral hemorrhage in the United States. World Neurosurg. 2012;78(6):640–5.
- Belur PK, Chang JJ, He S, Emanuel BA, Mack WJ. Emerging experimental therapies for intracerebral hemorrhage: targeting mechanisms of secondary brain injury. Neurosurg Focus. 2013;34(5):E9.
- Hyong A, Jadhav V, Lee S, Tong W, Rowe J, Zhang JH, Tang J. Rosiglitazone, a PPAR gamma agonist, attenuates inflammation after surgical brain injury in rodents. Brain Res. 2008;1215:218–24.
- Minematsu K. Evacuation of intracerebral hematoma is likely to be beneficial. Stroke. 2003;34(6):1567–8.
- Anik I, Secer HI, Anik Y, Duz B, Gonul E. Meta-analyses of intracerebral hematoma treatment. Turk Neurosurg. 2010;21(1):6–14.
- Wang J, Dore S. Inflammation after intrcerebral hemorrhage. J Cereb Blood Flow Metab. 2007;27(5):894–908.
- Feigin VL, Anderson NE, Rinkel GJE, Algra A, Gijn JV, Bennett DA, et al. Corticosteroids in patients with hemorrhagic stroke. Stroke. 2006;37:1344–5.
- Yrjänheikki J, Tikka T, Keinänen R, Goldsteins G, Chan PH, Koistinaho J. A tetracycline derivative, minocycline, reduces inflammation and protects against focal cerebral ischemia with a wide therapeutic window. Proc Natl Acad USA. 1999;96(23):13496–500.
- Tikka T, Fiebich BL, Goldsteins G, Keinanen R, Koistinaho J. Minocycline, a tetracycline derivative, is neuroprotective againts excitotoxicity by inhibiting activation and proliferation of microglia. J Neurosci. 2001;21(8):2580–8.
- Brunswick AS, Hwang BY, Appelboom G, Hwang RY, Piazza MA, Connolly Jr ES. Serum biomarkers of spontaneous intracerebral hemorrhage induced secondary brain injury. J Neurol Sci. 2012;321(2012):1–10.
- Castillo J, Dávalos A, Alvarez-Sabin J, Pumar JM, Leira R, Silva Y, et al. Molecular signatures of brain injury after intracerebral hemorrhage. Neurology. 2002;58(4):624–9.
- Mayne M, Ni W, Yan HJ, Xue M, Johnston JB, Del Bigio MR, et al. Antisense oligodeoxynucleotide inhibition of tumor necrosis factor-alpha expression is neuroprotective after intracerebral hemorrhage. Stroke. 2001;32(1):240–8.
- Salvatore CM, Techasaensiri C, Tagliabue C, Katz K, Leos N, Gomes AM, et al. Tigecycline therapy significantly reduces the concentrations of inflamatory pulmonary cytokines and chemokines in a murine model of Mycoplasma pneumoniae pneumonia. Antimicrob Agents Chemother. 2009;53(4):1546–51.
- Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27(8):1304–5.
- Madiyono B, Moeslichan S, Sastroasmoro S, Budiman I, Purwanto SH. Perkiraan besar sampel. In: Sastroasmoro S, Ismael S, editors. Dasar-dasar Metodologi Penelitian Klinis. 5th ed. Jakarta: CV Sagung Seto;2014. p. 352–95. Indonesian.
- Sanchez CE, Ogilvy CS, Carter BS. Outcomes studies in cerebrovascular neurosurgery. Neurosurg Focus. 2007;22(3):E11.
- Oliveira RA, Araújo S, Falcão AL, Soares SM, Kosour C, Dragosavac D, et al. Glasgow outcome scale at hospital discharge as a prognostic index in patients with severe traumatic brain injury. Arq Neuropsiquatr. 2012;70(8):604–8.
- Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24(7):987–93.
- Hemphill III JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professional from the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2031–60.
- Andres RH, Guzman R, Ducray AD, Mordasini P, Gera A, Barth A, et al. Cell replacement therapy for intracerebral hemorrhage. Neurosurg Focus. 2008;24(3–4):E16.
- Hwang BY, Appelboom G, Ayer A, Kellner CP, Kotchetkov IS, Gigante PR, et al. Advances in neuroprotective strategies: potential therapies for intracerebral hemorrhage. Cerebrovasc Dis. 2011;31(3):211–22.
- Katsuki H. Exploring neuroprotective drug therapies for intracerebral hemorrhage. J Pharmacol Sci. 2010;114(4):366–78.
- Xue M, Mikliaeva EI, Casha S, Zygun D, Demchuk A, Yong VW. Improving outcomes of neuroprotection by minocycline: guides from cell culture and intracerebral hemorrhage in mice. Am J Pathol. 2010;176(3):1193–202.
- Shaikh PZ. Cytokines & their physiologic and pharmacologic functions in inflammation: a review. Int J of Pharm Life Sci. 2011;2(11):1247–63.
- Lei B, Dawson HN, Roulhac-Wilson B, Wang H, Laskowitz DT, James ML. Tumor necrosis factor a antagonism improves neurological recovery in murine intracerebral hemorrhage. J Neuroinflammation. 2013;10:103.
- Patil CG, Alexander AL, Hayden Gephart MG, Lad SP, Arrigo RT, Boakye M. A population-based study of inpatient outcomes after operative managemant of nontraumatic intracerebral hemorrhage in the United States. World Neurosurg. 2012;78(6):640–5.
- Nag C, Das K, Ghosh M, Khandakar MR. Prediction of clinical outcome in acute hemorrhagic stroke from a single CT scan on admission. N Am J Med Sci. 2012;4(10):463–7. Medical Journal of Indonesia
- Daverat P, Castel JP, Dartigues JF, Orgogozo JM. Death and functional outcome after spontaneous intracerebral hemorrhage. A prospective study of 166 cases using multivariate analysis. Stroke. 1991;22(1):1–6.
- Ganti L, Jain A, Yerragondu N, Jain M, Bellolio MF, Gilmore RM, et al. Female gender remains an independent risk factor for poor outcome after acute nontraumatic intracerebral hemorrhage. Neurol Res Intl. 2013;2013:219097.
- Togha M, Bakhtavar K. Factor associated with inhospital mortality following intracerebral hemorrhage: a three year study in Tehran, Iran. BMC Neurol. 2004;4:9.
- Yousuf RM, Fauzi ARM, Jamalludin AR, How SH, Amran M, Shahrin TCA, et al. Predictor of in-hospital mortality in primary intracerebral haemorrhage in East coast of Peninsular Malaysia. Neurology Asia. 2012;17(2):93–9.
Copyright @ 2016 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id