Case Report
A rare case of cytomegalovirus papillitis in patient with immunodeficiency
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v25i3.1364 Med J Indones. 2016;25:190–4
Received: January 26, 2016
Accepted: August 28, 2016
Author affiliation:
Department of Ophthalmology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Kirana Hospital, Jakarta, Indonesia
Corresponding author:
Made Susiyanti
E-mail: madesusiyanti@yahoo.com
A 26-year-old male diagnosed with AIDS came with sudden blurred vision and central sco-toma in left eye since 2 weeks before admission. His visual acuity was counting finger at 5 meters with normal IOP and anterior segment. The posterior segment revealed edematous optic nerve covered by exudates and hemorrhages. Due to low CD4+ count and serological test result, we considered a HIV-related opportunistic ocular infection, specifically HSV infection. As visual acuity worsened during treatment with acyclovir, we performed PCR ex-amination from aqueous tap which revealed positive CMV DNA. Unfortunately, the visual acuity had worsened to no light perception before he received any specific anti- CMV agent. CMV papillitis is an unusual presentation of CMV retinitis. PCR examination from aqueous or vitreous tap should be performed while waiting for serological test result, especially in doubtful cases. Therefore, appropriate diagnosis and management can be established early to prevent irreversible visual loss.
Keywords
AIDS, cytomegalovirus, immunodeficiency, papillitis
Cytomegalovirus (CMV) papillitis is defined as greater than 270 degrees of disc edema/blurring of the disc margins as seen on direct examination and on color fundus photographs caused by CMV.1 CMV ocular infection will develop in 12% to 46% of patients with acquired immune deficiency syndrome (AIDS) in their lifetime. Of those patients with AIDS in whom CMV retinitis develops, CMV papillitis reportedly develops in up to 4% as well. Lestari2 reported the prevalence of CMV retinitis in Cipto Mangunkusumo Hospital (CMH) is 5.8%, there is no papil involvement reported in those cases. The majority of these patients have CD4 counts of less than 50 cells/mm3.1-3
Diagnosis of CMV papillitis in the setting of human immunodeficiency virus (HIV)/AIDS is essentially clinical, based on the features just described. In CMV papillitis, the optic nerve head is edematous with focal hemorrhages, and an afferent pupillary defect usually is present. Polymerase chain reaction (PCR)-based analysis of the aqueous or vitreous samples may provide critical diagnostic information of high sensitivity and specificity that allow the clinician to differentiate CMV from other herpetic causes of necrotizing retinitis and from toxoplasmic retinochoroiditis in immunocompromised patients with atypical lesions.1,3 In this case report, we demonstrated a rare case of ocular CMV infection that manifests as CMV papillitis in HIV/AIDS.
CASE REPORT
A male, 26 years old, came to Cipto Mangunkusumo Hospital, Jakarta on January 2014 complaining sudden blurred vision in left eye and central scotoma since two weeks before he was admitted. It was not red, it did not swell, and it was painless. Patient did not get any treatment for his eye before. There was no history of spectacles usage, hypertension, and diabetes mellitus. In the past medical history, this patient had been diagnosed with pulmonary tuberculosis, cryptococcal meningitis, and positive HIV test result. From social history, patient was a transmigrant from Sumatra Island. There was history of promiscuity with men and and intravenous drug user (IVDU).
Ophthalmological examination showed left eye’s visual acuity was 5/60, normal intraocular pressure (IOP), clear anterior segment, good right reflex with positive relative afferent pupillary defect (RAPD), and clear lens. In the posterior segment we found few cells in vitreous, and papil was hyperemic covered by exudates and peripapillary hemorrhages. There were flame-shaped hemorrhages, with turtous vein, and macular reflex hard to be evaluated. Right eye was in normal condition. We assessed this patient with specific opportunistic infection with several differential diagnosis including CMV, herpes simplex virus (HSV), cryptococcus, toxoplasmosis, and syphilis infection (Figure 1 and Figure 2).
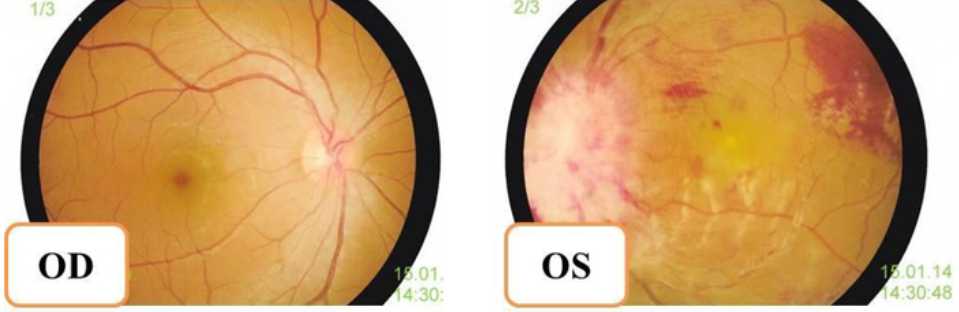
Figure 1. Normal funduscopy (right); hyperemic papil covered by exudates and peripapillary hemorrhages, flame-shaped hemorrhages (left). At this intital visit, the visual acuity of the left e ye is 5/60
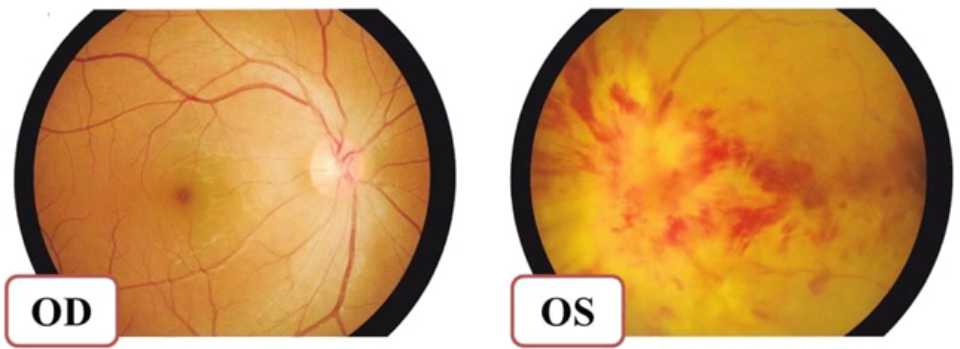
Figure 2. Normal funduscopy (right); the condition of the left eye is getting worse with hyperemic papil with extensive exudates and peripapillary hemorrhages, flame-shaped hemorrhages. At the third week follow-up, the visual acuity of the left eye is no light perception
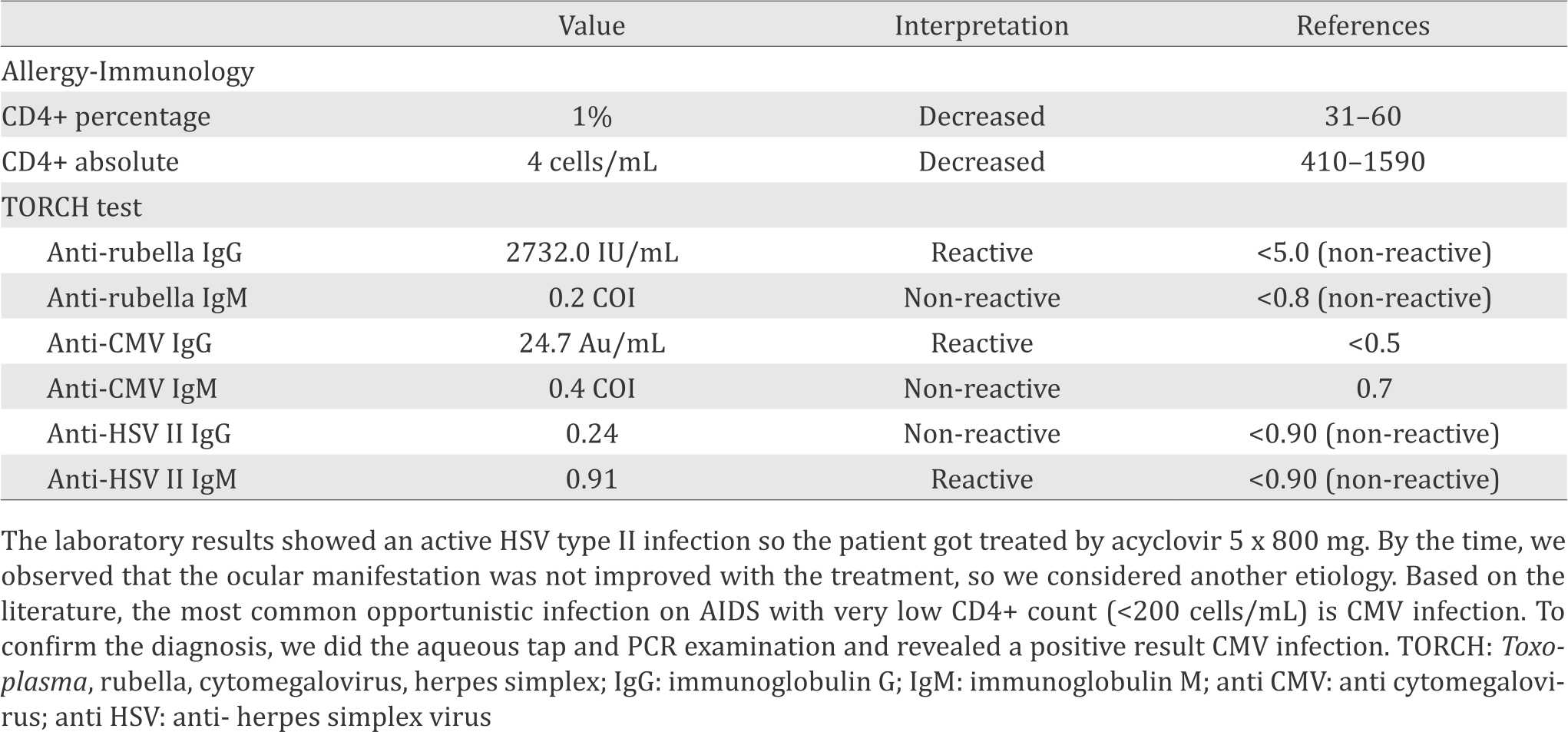
At the second and the third week after initial visit, the eye condition was getting worse, eventually leading to no light perception. Ancillary test revealed some abnormal result as shown in the Table 1. Based on clinical and laboratory results, we considered an active HSV infection, so we consulted the patient to Department of Internal Medicine and the patient got 800 mg acyclovir four times daily (Figure 3).
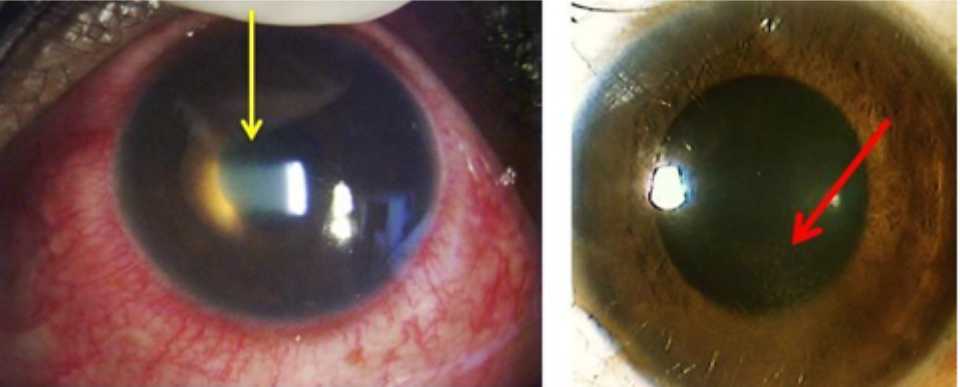
Figure 3. Immune recovery uveitis. Left eye shows conjunctival and ciliary injection, deep anterior chamber. Yellow arrow shows massive cells (+4) and flare (+2) in the anterior chamber. Red arrow shows keratitic precipitate
Due to worsening condition and confusing diagnosis, we performed PCR examination from aqueous tap to confirm the diagnosis. It was revealed that the patient had a positive CMV deoxyribonucleic acid (DNA). Therefore, we consulted to Department of Internal Medicine for a change to specific anti-CMV medication. The patient then received 900 mg valganciclovir twice a day for three weeks.
During the follow-up, five weeks after the first visit, the patient developed immune recovery uveitis with raising intraocular pressure up to 40 mmHg. He complained of pain of the left eye, accompanied with conjunctival and cilliary injection, the corneal edema and large keratitic precipitates were also noted. In anterior chamber, we found massive cells (+4) and flare (+2). The lenses were clear and the posterior segment was still the same. The patient received anti-glaucoma medication and topical steroid (Figure 4).
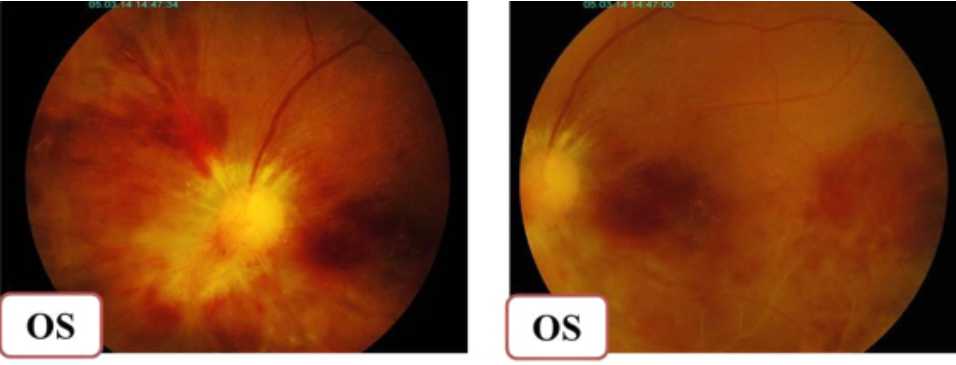
Figure 4. Left eye was showing subsided peripapillary hemorrhages and exudates after ad-ministration of oral valganciclovir 2 x 900 mg in third week
In seventh week after the initial visit, patient came with subsided peripapillary hemorrhages and exudates after administration of oral ganciclovir 900 mg twice daily in fourth week. This condition showed a good response to valganciclovir treatment. Based on the clinical manifestation, we diagnosed this patient with CMV papillitis (Table 1).
Table 1. Laboratory examination of clinical importance
Patient has been treated with highly-active anti- retroviral therapy (HAART) medication and also the anti-tuberculosis agent. HAART which consists of evafirenz, lamivudine, tenofovir disoproxil fumarate.
DISCUSSION
Opportunistic infections (OIs), which have been defined as infections that are more frequent or more severe because of immunosuppression in HIV-infected persons. It is important to recognize that the relationship between OIs and HIV infection is bidirectional.
Human immunodeficiency virus can cause systemic or organ diseases. Several systemic OIs include Mycobacterium tuberculosis infection, Cryptococcus infection, cytomegalovirus disease, toxoplasmosis infection. At the initial visit, our patient was already diagnosed with pulmonary tuberculosis and cryptococcal meningitis, still ongoing treatment. With the presenting systemic OIs, it is likely that this patient might have a specific organ disease.4,5
Iqbal6 stated an association between CD4+ cells count with ocular complication of HIV with the commonest infection is CMV. Cullen et al7 stated that neuro-ophthalmic manifestations of HIV tend to present at an advanced stage of the disease when CD4 cell counts are depleted below 200 cells/μl. In HIV-infected patients, opportunistic infections such as cytomegalovirus, toxoplasmosis, syphilis, and tuberculosis are by far the most common causes of optic nerve disorders.
In our cases, we found that patient was complaining sudden blurred vision of his left eye, diagnosed as AIDS since three months before came to this hospital (October 2013) with initial symptoms were loss of consciousness due to cryptococcal meningitis, starting HAART medication two months later (November 2013) and initial CD4+ count at first visit was 4 cells/mL (n: 410- 1,590 cells/mL). Initial presentation showed visual acuity 5/60, normal IOP, quiet eye with normal anterior segment, positive RAPD, and posterior segment manifestation that is edematous papil, peripapillary hemorrhages and exudates, and hemorrhages in retina. From this condition, our primary consideration was opportunistic infection with differential diagnosis caused by CMV, HSV, Cryptococcus, Toxoplasma, and syphilis. The laboratory examination and PCR testing show positive tendency to CMV infection. Based on this result we gave specific anti-CMV infection, valganciclovir 900 mg twice daily.
Cytomegalovirus papillitis has been described in immunocompromised patients and is usually a rapidly blinding disease.8 Many studies reported the incidence of CMV papilitis found less than 10% in CMV retinitis cases. CMV retinitis accounts for 75–85% of CMV disease and over 90% of blindness in AIDS patients. Freeman et al9 report papillitis is present in up to 4% of patients with CMV retinitis. Gross et al10 noted 4.1% patients with CMV retinitis also had CMV papillitis at initial presentation. Similarly, Rosecan et al11 noted optic nerve involvement in 8.3% eyes with CMV retinitis. Roarty et al12 also reported a patient with severe CMV papillitis and visual acuity of no light perception vision, and Palestine et al13 noted CMV papillitis in 7% eyes with CMV retinitis with no light perception vision upon initial presentation. Until now, there is no report of isolated CMV papillitis cases in without retinal manifestation in AIDS patient.
Successful management of active CMV retinitis reported by Figueiredo14 in an active CMV retinitis infection. In his report the patient had good visual outcome, from hand movement with good projection to 5/12 after induction doses of oral valganciclovir.
The Centers for Disease Control and Prevention (CDC), the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America15 give recommendation for treating CMV retinitis. For sight threatening lesions which is adjacent to the optic nerve or fovea, the recommended initial therapy comprised intravitreal injections of ganciclovir (2 mg/injection) or foscarnet (2.4 mg/injection) for 1–4 doses over a period of 7–10 days to provide higher intraocular levels of drug and faster control of the infection until steady state intraocular ganciclovir concentrations are achieved. This initial therapy might be accompanied by valganciclovir 900 mg twice daily for two until three weeks then followed by once daily doses. In our case, he given a systemic valganciclovir 900 mg twice daily in first three weeks, to control the presumably active CMV infection and to prevent the CMV involvement to the contralateral eye and also to improve patient’s systemic condition. Although the guideline of CMV papillitis’ management has not been established yet, this CDC recommendation is applicable in this case.
Based on the case explained above, we concluded the screening recommendations for patients with AIDS and low CD4+ T-cell counts should be performed routinely. PCR examination from aqueous or vitreous tap should be performed earlier while waiting for the serological testing result, especially in doubtful cases which severity progress rapidly. An appropriate diagnosis and management can be established and performed earlier to prevent the irreversible visual loss.
Conflicts of Interest
The authors affirm there is no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Patel SS, Rutzen AR, Marx JL, Thach AB, Chong LP, Rao NA. Cytomegalovirus papilltis in patients with acquired immune deficiency syndrome. Visual prognosis of patients treated with ganciclovir and/or foscarnet. Ophthalmology. 1996;103(9):1476–82.
- Lestari YD. Prevalensi manifestasi okular human immunodeficiency virus/acquired immunodeficiency syndrome di DKI Jakarta. [Thesis]. Jakarta: Univesitas Indonesia; 2009. p.3–5. Indonesian.
- Moorthy RS, Rao PK, Read RW, Gelder RN, Vitale AT, Bodaghi B, et al. Infectious ocular inflammatory diseases. In: Skuta GL, Cantor LB, Weiss JS, editors. Intraocular inflamation and uveitis. San Fransisco: American Academy of Ophthalmology; 2011-2012. p. 204–7.
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIVinfected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Available at http://aidsinfo.nih.gov/contentfiles/ lvguidelines/adult_oi.pdf. Accessed (February 13, 2014). p N1–8.
- Bentwich Z. Concurrent infections that rise the HIV viral load. J HIV Ther. 2003;8(3):72–5.
- Iqbal TB. HIV-related eye condition. In: Menon A, Kamarulzaman A, editors. Is it HIV? A hand-book for health care provider Thailand: The Australian Society for HIV Medicine (ASHM);KP Marketing.Darlinghurst: 2009. p. 46–51.
- Cullen C, Matlala B, Laher F, Pienaar A. Successful treatment of bilateral visual loss caused by idiopathic optic neuritis in an HIV-infected patient. The Southern African Journal of HIV Medicine 2011;12(4).
- De Silva SR, Chohan G, Jones D, Hu M. Cytomegalovirus papillitis in an immunocompetent patient. J Neuroophthalmol. 2008;28(2):126–7.
- Freeman W, Lerner CW, Mines JA, Lash RS, Nadel AJ, Starr MB. A prospective study of the ophthalmologic findings in the acquired immune deficiency syndrome. Am J Ophthalmol. 1984;97(2):133–42.
- Gross JG, Sadun AA, Wiley CA, Freeman WR. Severe visual loss related to isolated peripapillary retinal and optic nerve head cytomegalovirus infection. Am J Ophthalmol. 1989;108(6):691–8.
- Rosecan LR, Stahl-Bayliss CM, Kalman CM, Laskin OL. Antiviral therapy for cytomegalovirus retinitis in AIDS with dihydroxy propoxymethyl guanine. Am J Ophthalmol. 1986;101(4):405–18.
- Roarty J, Fisher EJ, Nussbaum JJ. Long-term visual morbidity of cytomegalovirus retinitis in patients with acquired immune deficiency syndrome. Ophthalmology. 1993;100(11):1685–8.
- Palestine AG, Stevens Jr G, Lane HC, Masur H, Fujikawa LS, Nussenblatt RB, et al. Treatment of cytomegalovirus retinitis with dihydroxy propoxymethyl guanine. Am J Ophthalmol. 1986;101(1):95–101.
- Figueiredo L, Rothwell R, Bilhoto M, Varandas R, Fonseca S. Immune recovery uveitis masked as an endogenous endophthalmitis in a patient with active CMV retinitis. Case Rep Ophthalmol Med. 2013;2013: Article ID 462968.p1–4
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Available at http://aidsinfo.nih.gov/contentfiles/ lvguidelines/adult_oi.pdf. Accessed (February 13, 2014). p N9–15.
Copyright @ 2016 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id
