
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Review Article
Chlorhexidine-alcohol versus povidone-iodine as preoperative skin preparation to prevent surgical site infection: a meta-analysis
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v26i1.1388 Med J Indones. 2017;26:54–61
Received: February 22, 2016
Accepted: January 29, 2017
Author affiliation:
Department of Surgery, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Corresponding author:
Aditya Wardhana
E-mail: aditya_wrdn@yahoo.com
Background
Surgical site infection remains substantial problems to surgeons and patients as it increases the morbidity, mortality, length of stay, hospital cost, rate of re-admission, and rate of re-surgery. This study aims to compare the use of chlorhexidine-alcohol versus povidoneiodine for preoperative skin preparation to prevent surgical site infection.
Methods
The literature search was conducted through the PubMed database on November 2015. Included studies were RCTs with the year of publication up to 2015 which compared the use of chlorhexidine-alcohol versus povidone-iodine in its effectiveness reducing surgical site infection in adult patients. The quality of the study was assessed using Jadad Score. A meta-analysis was conducted in the included study to obtain a pooled estimate of the effect size. The evidence of heterogeneity and publication bias was also assessed.
Results
Six RCTs with a total of 2,080 patients were included in the meta-analysis. It showed that the use of chlorhexidinealcohol was associated significantly with fewer SSIs (pooled risk ratio=0.60 (95% CI=0.45-0.79)) and fewer positive skin culture results (pooled risk ratio, RR=0.38 (95% CI=0.28- 0.51)) compared with povidone iodine.
Conclusion
Preoperative skin antisepsis with chlorhexidine is more effective than povidone-iodine in preventing surgical site infection.
Keywords
chlorhexidine-alcohol, povidone-iodine, skin antisepsis, surgical site infection
Surgical site infection (SSI) is the third most frequently reported nosocomial infection, accounting for 14% to 16% of all nosocomial infections among hospitalized patients as reported by The Centers for Disease Control and Prevention (CDC). Despite the advances in infection control practices such as improved operating room ventilation, sterilization methods, barriers, surgical technique, and availability of antimicrobial prophylaxis, SSI remains substantial problems to surgeons and patients as it increases the morbidity, mortality, length of stay, hospital cost, rate of re-admission, and rate of re-surgery.1,2
The selection of antiseptic skin solution prior to the surgery is an important step to prevent surgical site infections. Povidone-iodine (PVI) has a broad-spectrum antimicrobial activity against gram-positive and gram-negative bacteria, viruses, fungi, and protozoa. Its low-price and its broad-spectrum antimicrobial activity of this preparation made this solution remain the most widely used antiseptics. However, several studies indicated fibroblast and keratinocyte cytotoxicity, as well as delayed in collagen maturation and in epithelization by the use of PVI and thus, impaired wound healing.3 The use of PVI in a large open wound also contraindicated because PVI could induce systemic toxicity; therefore, special caution was needed when this agent used for patients with preexisting thyroid and renal disease.4,5 Based on literature, PVI has been shown to be inactivated by blood and protein serum, and it has been associated with skin staining and irritation.1 Moreover, it needs an average three minutes drying time for optimal function.6
On the other hand, chlorhexidine has a board spectrum bactericidal effect by disrupting the cell membrane potential, causing imbalance of osmotic equilibrium, and leading to cell death.7 Some studies highlight its rapid onset in certain bacteria with maximum effect within 20 seconds against S. aureus, E. coli, and yeast. The antibacterial effect could last up to 48 hours on the skin.8 In topical application, chlorhexidine shows the ability to bind the proteins in human tissue (skin and mucous membranes) with limited systemic and bodily absorptions, and not affected by the presence of body fluids such as blood.9,10 However, it should be noted that chlorhexidine is not sporicidal, and mycobacteria are highly resistant.10 Moreover, as chlorhexidine has no colour, it is difficult to identify on the patient’s skin after application. Its high-price compared to PVI also caused the potential disadvantage of this preparation. Its alcohol content, futhermore, made the preparation of chlorhexidine-alcohol became highly flammable although there was a very rare case documenting such hazards in the operating theatre.11 To prevent such events, a precaution should be carried out such as three minutes waiting time for the solution to evaporate and wiping the skin with a cotton swab before draping the surgical site. Nevertheless, low rate of skin irritation and its effective interaction with non-sporulating bacterial made this preparation promising to use.6 The CDC already recommends the use of >0.5% concentration of chlorhexidinebased preparation for cleansing vascular catheter site of insertion. Chlorhexidine-alcohol is a newly introduced antiseptic preparation in health care facility in Indonesia. Thus, it provides alternative for healthcare practitioner to choose despite the commonly use antiseptic (povidone iodine).
A meta-analysis study was conducted to examine whether povidone-iodine or chlorhexidine is a preferred skin antiseptic before a surgery in order to reduce the rate of surgical site infection.
METHODS
The meta-analysis was conducted through the PubMed database on November 2015. The search was done using Endnote X7 with keywords: “chlorhexidine” or “chlorhexidine-alcohol” and “povidone-iodine” or “iodophor” and “surgery” and “skin disinfectant”. All the studies were screened by the title and the abstract, retrieved potentially relevant articles in full text, and assessed them for the inclusion criteria. Inclusion criteria for this study include: (1) randomized controlled trials (RCTs) with year of publication up to November 2015; (2) english literature; (3) the studies compared between preoperative chlorhexidine-isoprophylalcohol (CHX-IPA) (any concentrations) and PVI (any concentrations); (4) patient aged of 18-year old or above; (5) assessed the outcome of surgical site infections (SSIs); (6) any clean, clean contaminated, and contaminated surgical procedures. Studies evaluating chlorhexidine shower, bath, or oral rinse for pre-surgery antisepsis were excluded, and so did those evaluating chlorhexidine preparation without adding or containing the isoprophyl-alcohol. In addition, studies evaluating the preparations that have another mixture added to the povidone-iodine (such as iodine with mixture of any concentration of alcohol) were also excluded from the meta-analysis.
The quality of each study was evaluated using the Jadad score. It calculates the score of the following items for evaluating RCT: randomization, double blind, and dropouts. The total score ranges from 0 to maximum of 5.16
The primary outcome for the meta-analysis is the present of surgical site infection. Moreoever, the secondary outcome is the present of positive cultures after the application of skin antisepsis. Data were entered and analyzed in Microsoft Excel spreadsheet and RevMan version 5.3. A meta-analysis was conducted to obtain a pooled estimation of the effect size, which was reported as risk ratio (RR) using fixed effect model, with a 95% confidence interval (CI). Heterogeneity was assessed using the I2 test (≥50% was considered substantial heterogeneity) and c2 test (p≤0.10 was considered significant heterogeneity).17 The publication bias was assessed by visual inspection of the funnel plots.18 All statistical analysis of the result were performed by the RevMan version 5.3 (Nordic Cochrane Centre).19
RESULTS
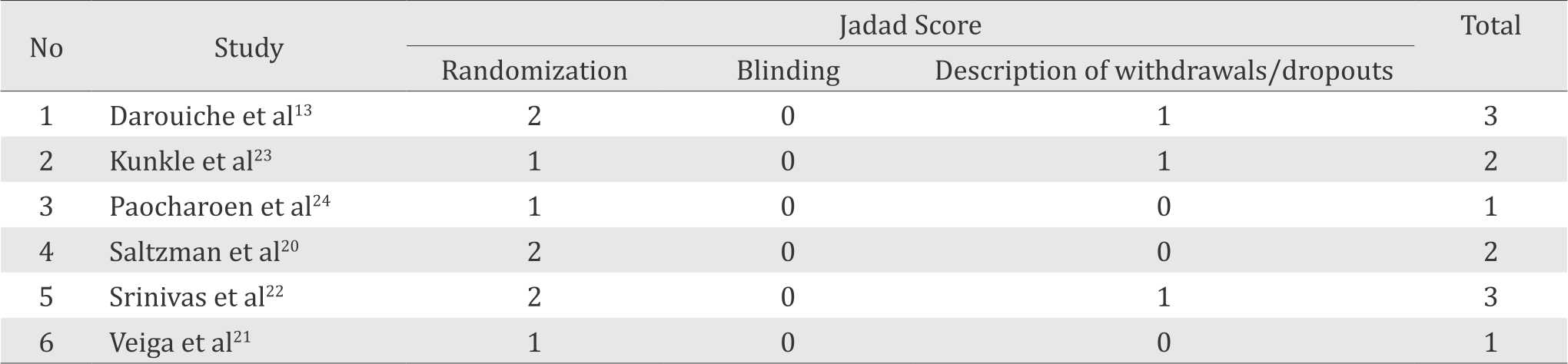
Of 881 studies identified for title and abstract screening, 19 articles underwent the full text reviews, and only six RCTs were included in our final analysis (Figure 1). The quality of the RCT was evaluated using the Jadad Score giving a varying score of one to three point. None of the studies showed the Jadad Score above of three point (Table 1).
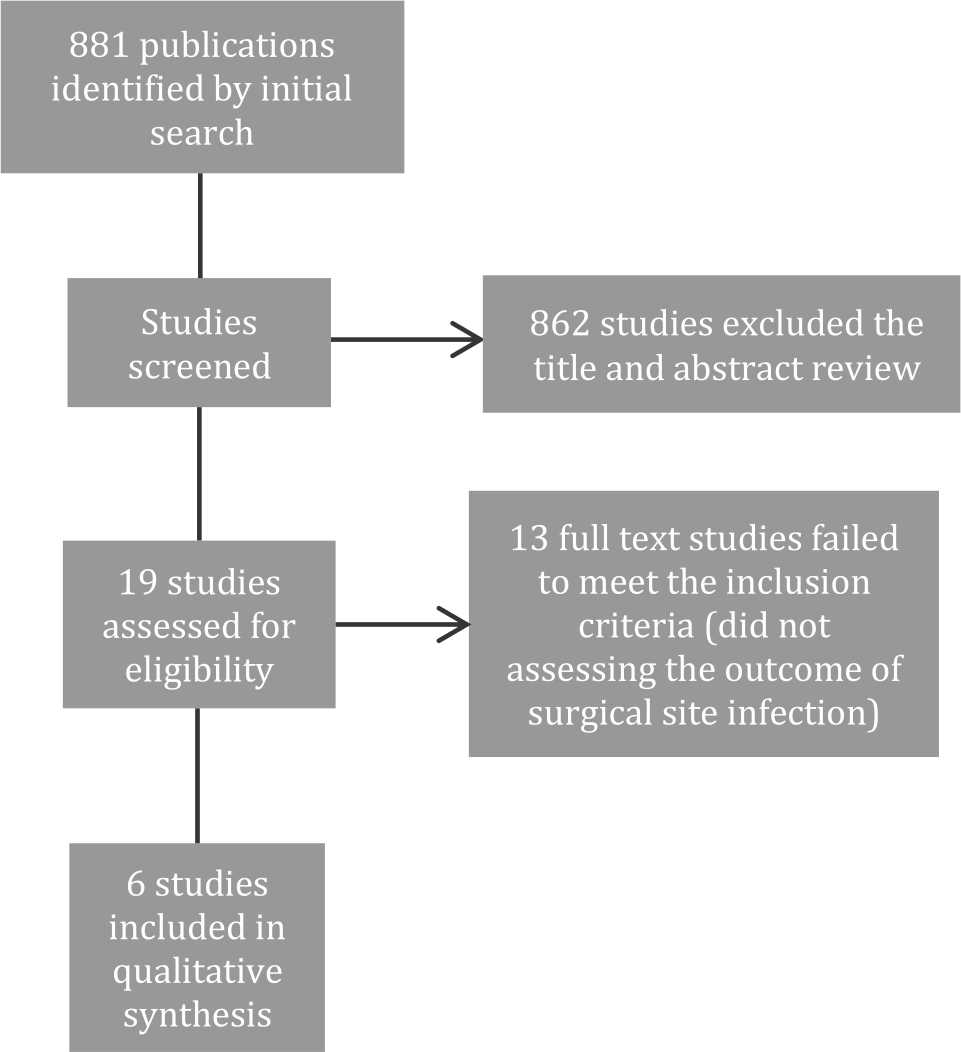
Figure 1. Flow diagram of article screening for meta-analysis
Table 1. Jadad score evaluation of the study
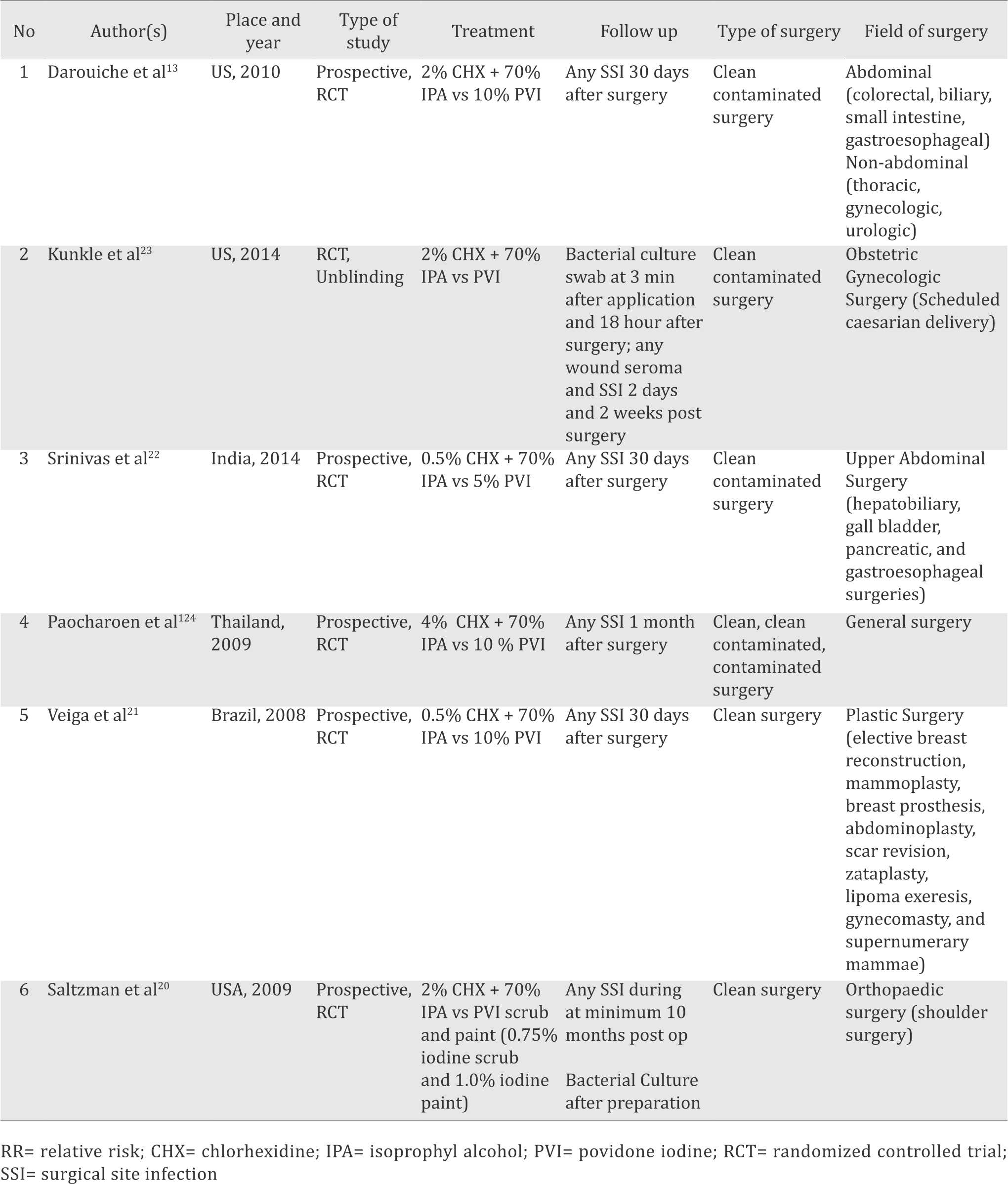
The six trials included in this study had a total of 2,080 patients.13,20–24 Two trials reported on patients who had a clean surgery,20,21 three trials included patients underwent clean contaminated surgery,13,22,23 and one trial on mixed surgery patients (clean, clean contaminated, and contaminated surgery) as shown in Table 2.24 The experiment group used chlorhexidine scrub and/or paint in varying concentrations (from 0.5% to 4%) with a mixture or addition of 70% isoprophyl-alcohol. The comparison group used povidone-iodine scrub and/or paint with varying concentrations (0.7% to 10%). One study reported a positive skin culture for multiple sampling sites (axilla and shoulder antero-posterior),20 so the result of each site (made the number of patients doubled) was combined. The surgical site infection rates for statistical analysis were obtained by adding all types of SSI presented in the study (all superficial incisional infection (SII), deep incisional infection (DII), and organ space infection (OSI). The SSI evaluated in this study was the one that had the longest observation period.
Table 2. Characteristics of eligible studies
Surgical site infection
Three trials reported significant decreases in SSIs with Chlorhexidine and Isoprophyl Alcohol compared to PVI.13,21–24 One trial showed nonsignificant decreases in the number of SSIs with chlorhexidine use,22 one trial found out nonsignificant increases in the number of SSIs with chlorhexidine use,23 and one trial reported no SSIs in either study groups.20
All six studies reported the post-operative SSI rates. The SSI occurred in 63 out of 1,009 (6.24%) patients who received CHX-IPA and 117 out of 1,071 (10.92%) patients received PVI as skin antisepsis before surgery. The meta-analysis showed that CHX-IPA significantly decreased the risk for SSI, compared to the use of PVI (pooled RR=0.60 (95% CI=0.45-0.79) (Figure 2). No significant study of heterogeneity was found (I2 =0%; x2 test, p=0.776). Furthermore, no evidence of publication bias was found from a visual inspection of funnel plots (Figure 3).
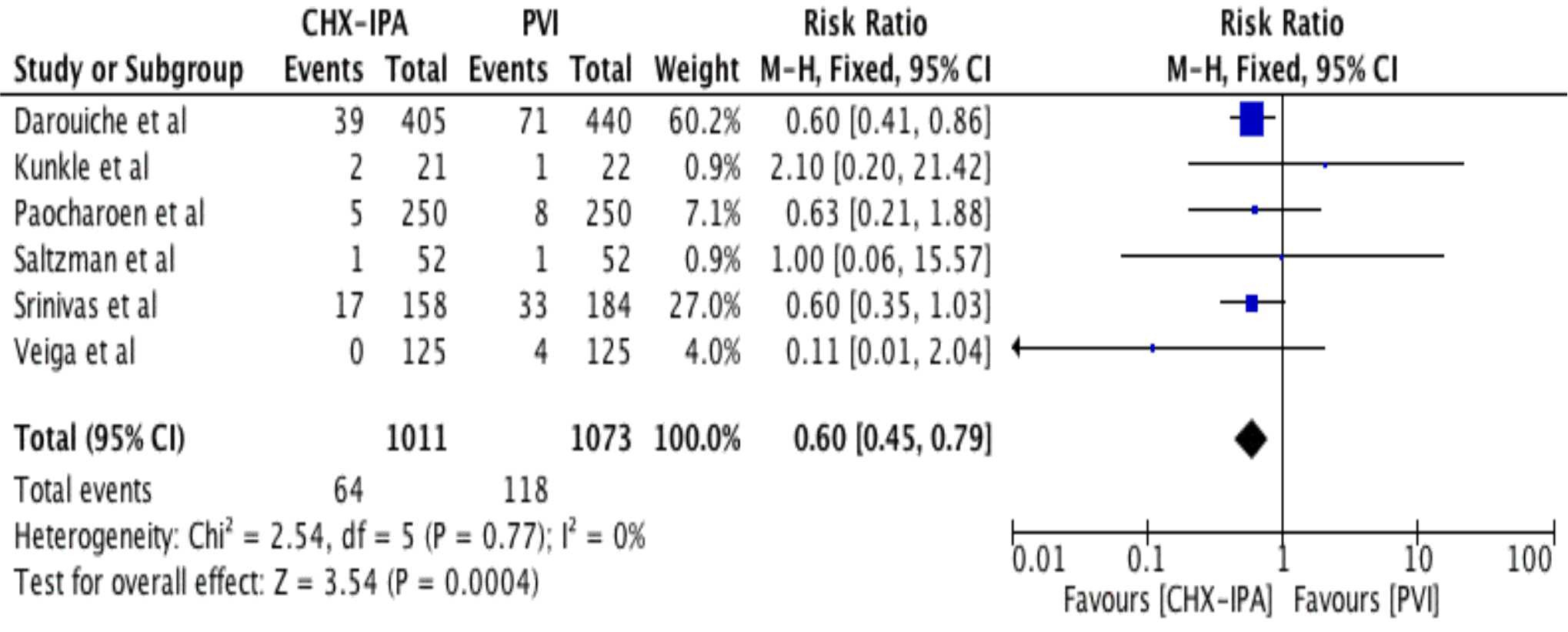
Figure 2. Forest plot comparing the incidence of surgical site infection following skin preparation with chlorhexidine-isopropylalcohol (CHX-IPA) versus povidone-iodine (PVI)
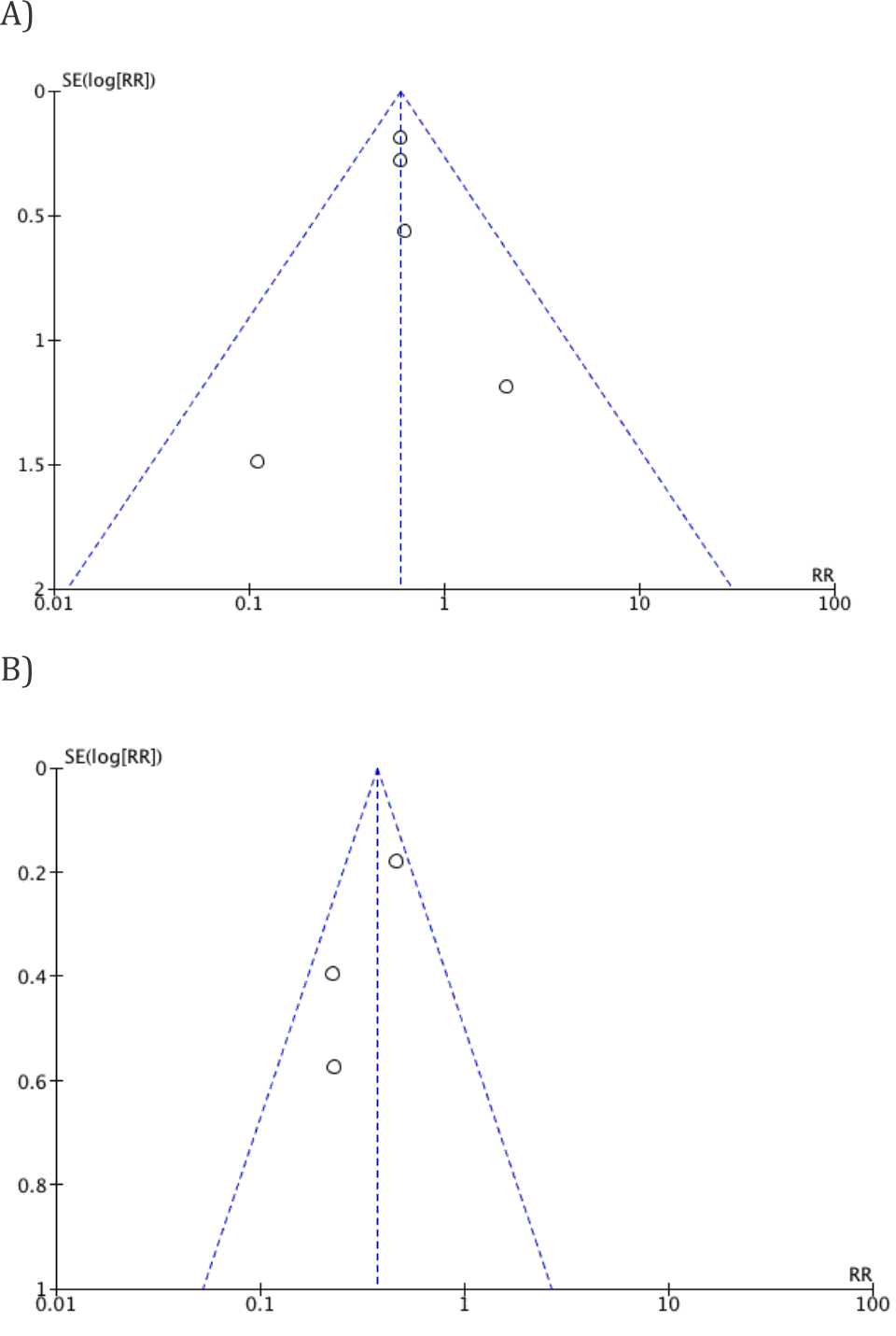
Figure 3. Funnel plots for surgical site infection (A) and for positive culture result (B) after application preoperative skin antisepsis of CHX-IPA versus PVI
Positive cultures after skin antisepsis
Two trials reported significant reduced positive culture results after the use of CHX-IPA as a preoperation skin antisepsis compared with the use of PVI.23,24 One trial reported insignificant reduction of positive cultures in the number of positive cultures when CHX-IPA was used compared with the use of PVI.20
The meta-analysis of the three studies showed that the use of CHX-IPA significantly decreased the risk for a positive culture result after application, compared with PVI (pooled RR=0.38 (95% CI=0.28-0.51). No significant heterogeneity was found (I2 =46%; x2 test, p=0.165) (Figure 4). Potential publication bias for positive culture result from a visual inspection of funnel plots was found as shown in Figure 3.
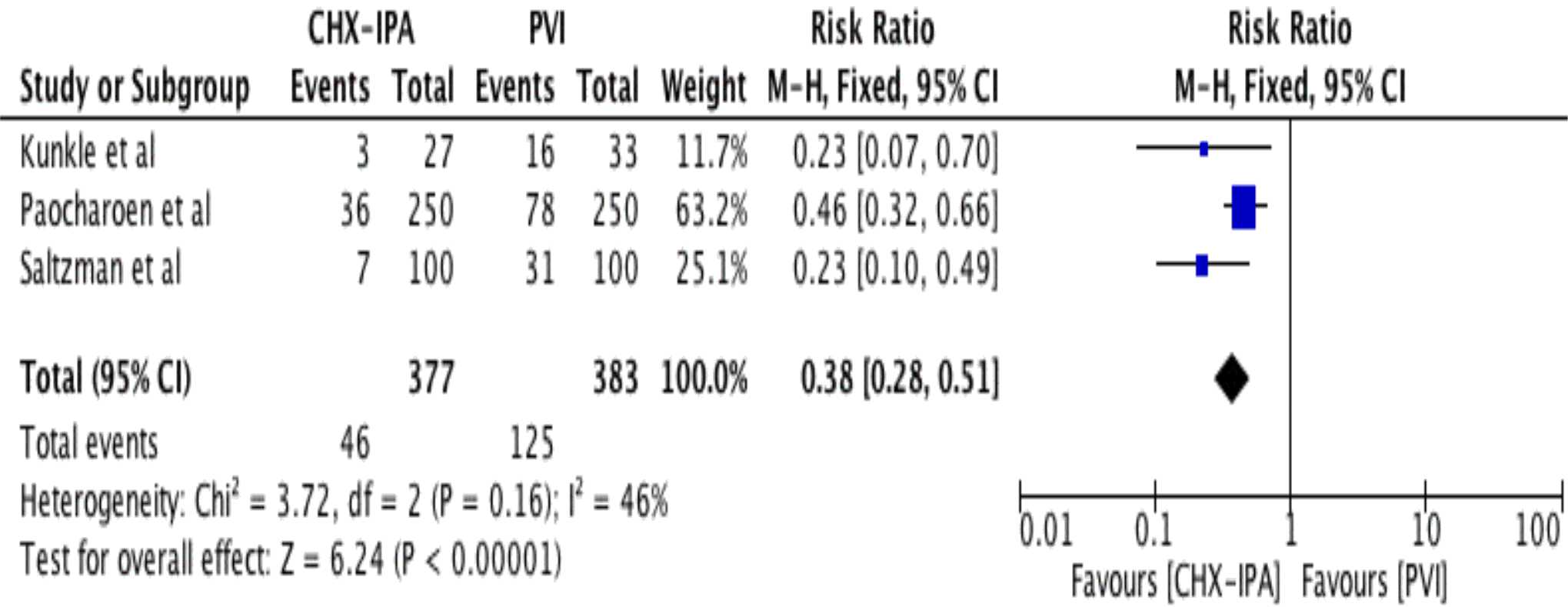
Figure 4. Forest plot comparing the positive cultures of bacterial growth following skin preparation with chlorhexidine-isopropyl- alcohol (CHX-IPA) versus povidone-iodine (PVI)
DISCUSSION
This meta-analysis showed superior result to the use of chlorhexidine in combination with isoprophyl-alcohol for antisepsis solution before surgery compared to the use of povidone-iodine in reducing the number of surgical site infection and the positive skin culture after application.
There was a 40% reduction in the risk of SSIs among patients received preoperative skin antisepsis of chlorhexidine compared to those who received povidone-iodine. This estimated number is similar in all of the studies, except three studies that had different estimation points from the pooled estimation.20–23 However, these studies only weighted less than 5% of the total studies, and had only a few events (total of 7 from 180 cumulative SSIs). Another review from Lee, et al25 also stated that chlorhexidine application as a skin antisepsis gave a reduction of 36% in the risk of SSIs compared to PVI. Meanwhile, a study from Noorani et al14 showed a slightly similar result from this study, which was a reduction of 42% in the risk of SSIs when using chlorhexidine as a presurgical antisepsis compared to PVI. However, Noorani et al14 also stated that there was no clear benefit in the favor of either agents in preventing intra-abdominal sepsis.
This study also supports the use of chlorhexidine for pre-surgical skin antisepsis. It shows that the use of chlorhexidine can reduce positive culture after skin antisepsis by 62%. This estimated number is similar in all of the included studies. Another meta-analysis also provides a slightly different rate of 56% reduction in positive skin culture results after skin preparation compared with PVI.25
Nevertheless, there were several limitations in this study. First, we found only six relevant studies. More relevant studies might be found if other sources such as other database (e.g.: excerpta medica database (EMBASE), Cochrane database of systematic review, cumulative index to nursing and allied health literature (CINAHL), etc.), conference proceedings, books, unpublished literature, and literature other than English language were included. Second, there were two studies that contributed more than 60% of the patients included in the meta-analysis.13,24 However, through the I2 and x2 test conducted, we found no evidence of significant heterogeneity in this meta-analysis, though the secondary outcome had borderline heterogeneity (I2=46%). Third, although the author had limited the number of studies that used chlorhexidine with mixture or addition of isoprophyl-alcohol, there were still different concentrations of chlorhexidine used in this study. Three trials used 2%,13,20,23 two trials used 0.5%,21,22 and another one trial used 4%.24 However, this study follows the CDC guideline which suggests that any concentration of chlorhexidine greater than 0.5% with alcohol can be used as a skin antiseptic before the insertion of intravascular catheter to decrease contamination. Another meta-analysis with specific concentration of chlorhexidine was needed to determine which concentration of chlorhexidine was preferred to reduce the surgical site infection. Fourth, in this study the type of surgery was varied from clean to clean-contaminated surgery with different types of specializations (Table 2). Further study in specific field of surgery and type of surgery is recommended.
This meta-analysis showed a superior result in chlorhexidine-isoprophylalcohol preparation as skin antisepsis. The high cost and the availability of this preparation became potential drawbacks to Indonesian surgeons. A study on cost-benefit model comparing the economic value of using chlorhexidine compared to PVI concludes that although chlorhexidine is more costly than iodine, the dramatic reduction of SSIs will likely result in greater overall cost savings with chlorhexidine use.25
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect Control Hosp Epidemiol. 1999;20(4):250–78.
- Yeung LL, Grewal S, Bullock A, Lai HH, Brandes SB. A comparison of chlorhexidine-alcohol versus povidoneiodine for eliminating skin flora before genitourinary prosthetic surgery: a randomized controlled trial. J Urol. 2013;189(1):136–40.
- McKenna PJ, Lehr GS, Leist P, Welling RE. Antiseptic effectiveness with fibroblast preservation. Ann Plast Surg. 1991;27(3):265-8.
- Welch JS. Efficacy and safety of povidone-iodine underscored. J Emerg Nurs. 1992;18(3):191–2.
- Shetty KR, Duthie EH Jr. Thyrotoxicosis induced by topical iodine application. Arch Intern Med. 1990;150(11):2400–1.
- 3m.com [Internet]. DuraPrep surgical solution (iodine povacrylex [0.7% available iodine] and isopropyl alcohol, 74% w/w) patient preoperative skin preparation. [cited November 2015]. Available from: http://solutions.3m.com/wps/ portal/3M/en_US/SH/SkinHealth/products/ catalog/? PC_7_RJH9U5230GE3E02LECFTDQG207_ nid=GSF83Z3YYXbeJLRV63SXXBgl.
- Hibbard JS. Analyses comparing the antimicrobial activity and safety of current antiseptics: a review. J Infus Nurs. 2005;28(3):194–207.
- who.int [Internet]. WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care [update: 2009; cited: 2015]. Available from: http://www.who.int/gpsc/5may/ tools/9789241597906/en/
- Saaiq M, S Zaib, S Ahmad. Electrocautery burns: experience with three cases and review of literature. Ann Burns Fire Disasters. 2012;25(4):203–6.
- McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev. 1999;12(1):147–79.
- Lim KS, Kam PC. Chlorhexidine--pharmacology and clinical applications. Anaesth Intensive Care. 2008;36(2):502–12.
- Sibbald RG, Leaoer DJ, Queen D. Iodine made easy. Wounds International. 2011; 2(2):s1–6.
- Darouiche RO, Wall MJ Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N Engl J Med. 2010;362(1):18–26.
- Noorani A, Rabey N, Walsh SR, Davies RJ. Systematic review and meta-analysis of preoperative antisepsis with chlorhexidine versus povidone-iodine in cleancontaminated surgery. Br J Surg. 2010;97(11):1614–20.
- O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162–93.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized control trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
- Egger M. Under the meta-scope: possibilities and limits of meta-analyses. Schweiz Med Wochenschr. 1998;128(48):1893–901. Germany.
- community.cochrane.org [Internet]. Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. Available from: http:// community.cochrane.org/tools/review-productiontools/ revman-5
- Saltzman MD, Nuber GW, Gryzlo SM, Marecek GS, Koh JL. Efficacy of surgical preparation solutions in shoulder surgery. J Bone Joint Surg Am. 2009;91(8):1949–53.
- Veiga DF, Damasceno CA, Veiga-Filho J, Figueiras RG, Veira RB, Florenzano FH, et al. Plast Reconstr Surg. 2008;122(5):170e–1e.
- Srinivas A, Kaman L, Raj P, Gautam V, Dahiya D, Singh G, et al. Comparison of the efficacy of chlorhexidine gluconate versus povidone iodine as preoperative skin preparation for the prevention of surgical site infections in clean-contaminated upper abdominal surgeries. Surg Today. 2015;45(11):1378–84.
- Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2015;28(5):573–7.
- Paocharoen V, Mingmalairak C, Apisarnthanarak A. Comparison of surgical wound infection after preoperative skin preparation with 4% chlorhexidine [correction of chlohexidine] and povidone iodine: a prospective randomized trial. J Med Assoc Thai. 2009;92(7):898–902.
- Lee I, Agarwal RK, Lee BY, Fishman NO, Umscheid CA. Systematic review and cost analysis comparing use of chlorhexidine with use of iodine for preoperative skin antisepsis to prevent surgical site infection. Infect Control Hosp Epidemiol. 2010;31(12):1219–29.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id