
Section Abstract Introduction Methods Results Discussion Conflict Of Interest Acknowledgment References
Community Research
Determinants of HIV provider-initiated testing and counseling screening service used by pregnant women in primary health centers in Surabaya
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v26i4.1398 Med J Indones. 2017;26:293–301
Received: March 1, 2017
Accepted: December 15, 2017
Author affiliation:
Department of Public Health and Preventive Medicine, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
Corresponding author:
Samsriyaningsih Handayani
E-mail: samsri.handayani@gmail.com
Background
Offering free HIV screening service for pregnant women in primary health center in Surabaya has become obligatory since 2014, but only 70% used the service. Prior studies on HIV screening mostly focused on Voluntary Counseling and Testing.
Methods
This was a cross-sectional study. Interviews were conducted with 150 pregnant women attending antenatal care in 1 of 9 public health centers (PHCs) in Surabaya and offered HIV screening within the same PHC. The eligibility criterium was pregnant women attending antenatal care in PHCs. The exclusion criteria were having been counseled for HIV prior to the interviews and/or experiencing an obstetric emergency. Using PRECEDE Framework with the concept of a comprehensive framework, this study focuses on identifying determinants of HIV PITC service use in PHCs in Surabaya. Binary logistic regressions and multiple binary logistic regressions were used in analyses.
Results
The service use was associated with self-confidence of getting blood drawn for the test (p<0.001, adjusted OR=12.368, 95% CI=3.237–47.250) and past use of midwife private service for current pregnancy (p=0.029, adjusted OR=3.902, 95% CI=1.150–13.246). Self-confidence of getting blood drawn for HIV test mediated the effect of past use of midwife’s private service on HIV screening use.
Conclusion
Past use of midwife’s private service affected self-confidence of getting blood drawn for HIV test on HIV screening use, and self-confidence affected the use of HIV PITC. This study results suggest that more midwives’ private practices are needed to increase the use of HIV PITC screening in PHC.
Keywords
c oncentrated HIV epidemic area, HIV PITC screening, pregnant women, urban primary health center
Human immunodeficiency virus (HIV) screening among pregnant women is essential to detect both the spread of the infection among women and its maternal transmission to children. In 2012, within voluntary counseling and testing context, out of 43,624 pregnant women tested for HIV in 92 hospitals and 13 public health centers (PHCs) in 31 Indonesian provinces providing mother-to-child transmission (MTCT) services, 1,329 (3.01%) were positive.1 In 2013, the issuance of the Decree of the Minister of Health of the Republic of Indonesia marked the shift of the HIV screening policy from client-initiated testing (CIT) and voluntary HIV counseling and testing (VCT) to provider-initiated testing and counseling (PITC) for pregnant women in low and concentrated epidemic areas in Indonesia.2 In the new policy, pregnant women are informed about the aim of the screening and consented if they agree to take the procedure. Prior to get their blood drawn, pre-HIV-test counseling is replaced by an informational session while post- HIV-test counseling is obligatory.3
Surabaya was appointed as the site of a pilot project of the new policy implementation. In January 2014, an opt-out HIV PITC screening for expectant mothers as part of prevention of MTCT program begin following the World Health Organization (WHO) guidelines.4 In its implementation, PITC is integrated into the routine antenatal care in every PHC in Surabaya besides the existing hepatitis B and sexually-transmitted infection screenings, urinalysis, nutritional assessment and dental check that take approximately one hour. PITC would affect approximately 47,567 estimated pregnant women in Surabaya, 40% of whom attended antenatal care in PHCs.5 Private practicing midwives were informed about the new policy and encouraged to refer their clients to PHCs in the areas as they did not meet the qualification to counsel and test. Test positive expectant mothers are referred to appointed public hospitals to start anti-retroviral therapy at no cost. In the mid-year of the pilot project of free HIV PITC screenings in 2014 for expectant mothers, it was noted that not all accepted the screening. Of the 100% targeted pregnant women in PHCs, 30% disagreed to take the test.6 Therefore, identification of factors contributing to the acceptance of the screening was needed.
PRECEDE framework provides comprehensive and systematic procedures, organized in a conceptual framework of possible relationships. Studies on HIV screening among pregnant women did not either use the comprehensive PRECEDE framework8–10 or focused on VCT,11,12 allowing misidentification of which factors that actually played the bigger role. This misidentification could lead to program’s financial misallocation of HIV PITC screening. Hence, this study was aimed at identifying determinants of HIV PITC screening service.
This study aimed at determining factors associated with the use of HIV screening service by pregnant women through PITC in Surabaya using diagnostic components of the PRECEDE-PROCEED framework.7 PRECEDE stands for predisposing, reinforcing and enabling constructs in educational diagnosis and evaluation, while PROCEED stands for policy, regulatory, and Organizational Constructs in Educational and Environmental Development. Only PRECEDE was applied in this study.
METHODS
This was a cross sectional study. Nine PHCs in 9 Surabaya areas where most pregnant women resided were chosen. Convenience sampling was applied for easiness, i.e. for convenience, a day per week was chosen for data collection time. That was the day pre-determined by PHCs as weekly elective antenatal visit day. All eligible pregnant women coming for antenatal care in a chosen day were recruited. New pregnant women came in any day outside the pre-determined day was served by PHCs but were not included in the study. Random sampling could not be applied because the antenatal care (ANC) clinics were walking-in sites. There was no need to make appointments prior to the visits, thus a list of patients where a random sampling would be based on could not be obtained. An interview using a structured questionnaire was conducted by a trained female interviewer in the PHC just after the participant used the routine antenatal care service. Participants were excluded from the study if they have been counseled in other health facilities prior to their visits to the participating PHCs and or were in obstetric emergency situations.
This study used Green’s and Kreuter’s definitions of predisposing, reinforcing and enabling factors of health service use. Predisposing factors refer to individual characteristics that motivate behavior. Knowledge, attitude, belief, personal preferences, skills, and self-efficacy fall within this group.7 In this study, predisposing factors were explored by asking participants to self-report their perception on their knowledge on HIV and answer standard questions on HIV composed by the Joint United Nations Programme on HIV/AIDS UNAIDS13: “Can the risk of HIV transmission be reduced by having sex with only one uninfected partner who has no other partners?”, “Can a person reduce the risk of getting HIV by using a condom every time they have sex?”, “Can a healthy-looking person have HIV?”, “Can a person get HIV from mosquito bites?” and “Can a person get HIV by sharing food with someone who is infected?”
Participants were also asked to self-report their self-confidence to get their blood drawn and attend post-HIV-test counseling with this question: “Do you feel that you are confident to get blood drawn/take post-HIV-test counseling?” Participants were also asked to report their awareness of examinations or tests to detect HIV, HIV medication, and prophylaxis for HIV motherto- child transmission and to rate their selfconfidence of using HCT service. These questions were pilot-tested and minor revisions were made. Reinforcing factors refer to “rewards or punishments following or anticipated as a consequence of a behavior.”7 In this study, they were husband’s advice to participants to get tested and husband’s reminder to participant to get health checked in PHC, assuming that the women anticipated to gain at least verbal rewards after taking their advice. Past use of midwife service for current pregnancy was also a reinforcing factor, assuming that they would get better services when they were referred back to referring midwives. Midwives working in solo private and non-PHC facilities committed to send pregnant women to PHC for HIV checks. The agreement was reached between the Surabayan chapter of the Midwife Professional Association (Ikatan Bidan Indonesia Surabaya). After the screening was done, women’s were referred back to the referring midwives.
Enabling factors refer to “Environmental characteristics that facilitate action and skills or access to resources or services needed to adopt certain behavior”.7 These factors were explored by asking participants to self-report the order of their current pregnancy, the number of antenatal care they attended in the current PHC they were visiting, the distance between their residences and PHCs, the time needed to access the testing service, their preference on service hours, husbands’ advice to get tested for HIV, husbands’ reminder to get health checked in the PHC, and whether they used midwife services for the current pregnancy prior to their current visit to PHC. The study flow is presented in Figure 1.
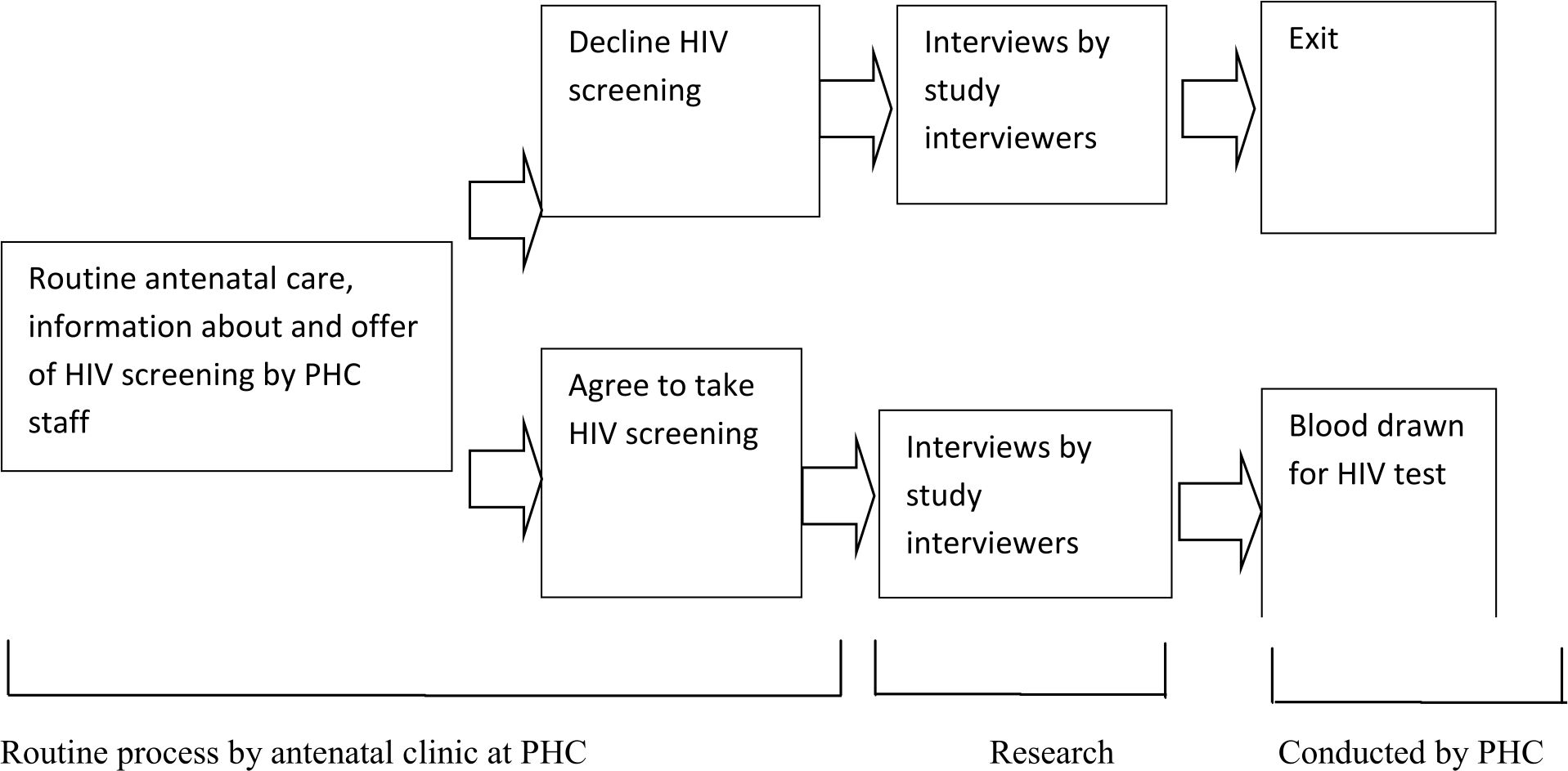
Figure 1. Study flow. PHC= primary health center
Ethical consideration
Ethical permission No. 315/EC/KPEK/ FKUA/2014 was granted by the Institutional Review Board of Universitas Airlangga Faculty of Medicine). Participants or their parents were asked for consents before the interviews started and a written informed consent was obtained prior to each interview. Under-aged participants were accompanied by at least one of their parents. Participation in the study was voluntary. All data were kept confidentially. After each interview, participants were told about the correct answers to HIV knowledge questions. Some monetary compensation was provided for the time the participants dedicated to this study.
Data analysis
Categorical data were dichotomously re-coded. “Don’t know” and “decline to answer“ responses to HIV knowledge questions were treated as incorrect answers and coded “1”. “Don’t know” and “decline to answer“ responses to other questions were treated as missing values. Lower values and orders were coded “1”. Multiple imputations14,15 using Statistical Package for the Social Sciences (SPSS) version 17 was applied to replace missing values. Descriptive analyses were applied to all variables. Determinants of HIV screening service use were analyzed with bivariate binary logistic regressions. Factors with p<0.05 were included in the respective multivariate binary logistic regressions. The procedure of Baron and Kenny16 was run on variables to detect mediation and moderation effect.
RESULTS
Data were collected in 2014 from 150 participants in 9 participating PHCs. Twenty one (14%) participants declined and 129 (86%) agreed to use HIV screening services.
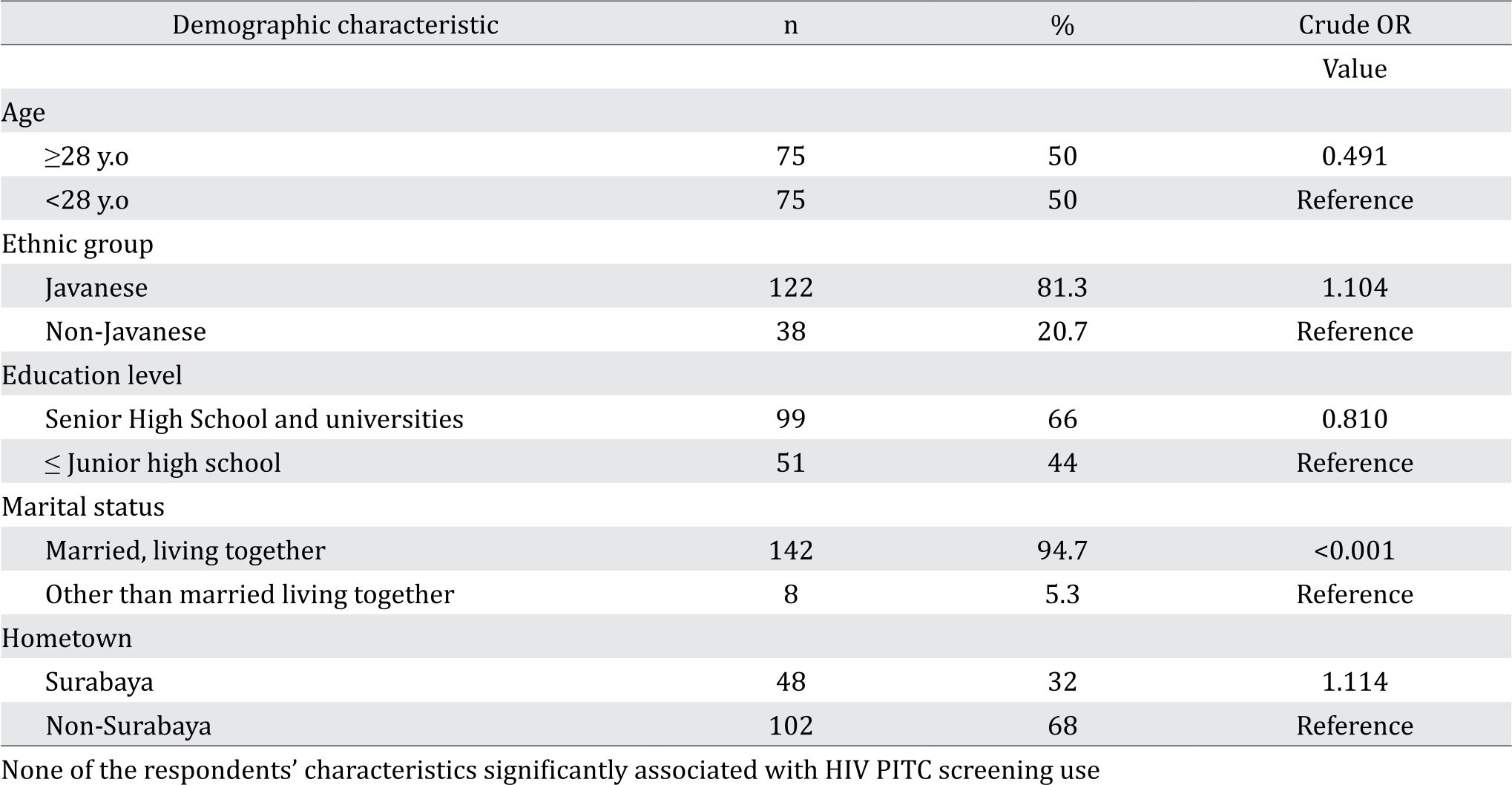
Demographic characteristics
Frequency distribution of demographic characteristics is presented in Table 1.
Table 1. Respondent characteristics and results of logistic regression on the use of HIV screening service
Predisposing, reinforcing and enabling factors and HIV screening service use
Table 2 presents the detailed frequency distribution of predisposing, reinforcing and enabling factors and the results of bi-variate binary logistic regressions of the use of HIV screening service. Multivariate binary logistic regressions on the PITC HIV use were applied within each group of factors to determine significant associations.
Table 2. Frequency distribution of predisposing, reinforcing and enabling factors and results of bivariate and multivariate binary logistic regressions of the use of HIV screening service
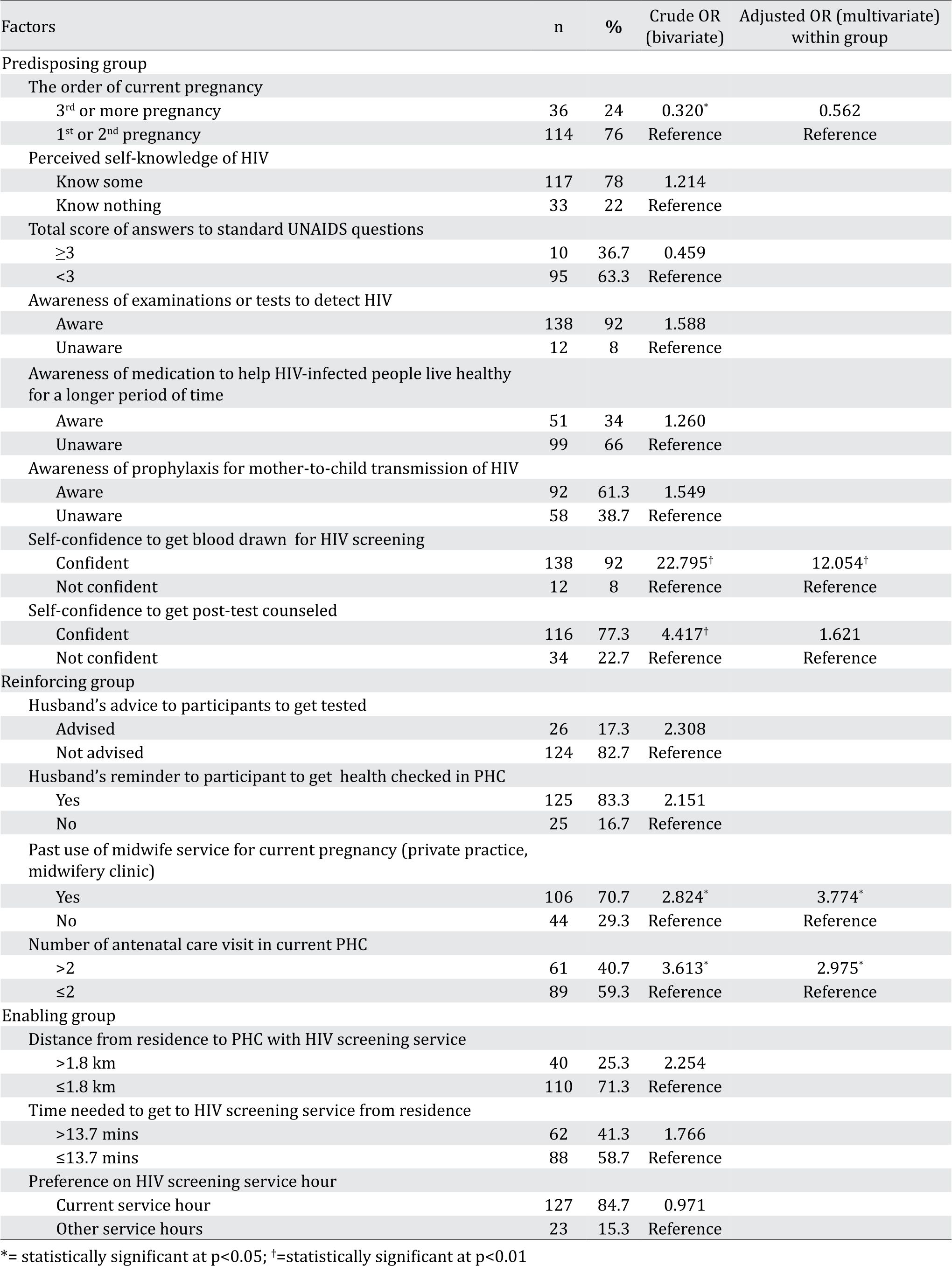
The distance between participants’ residence and the service unit ranged from 100 meters to 10 km (mean ± SD=1.8±1.6 km). The time needed to access HIV screening service ranged from 2 to 60 minutes (mean ± SD=13.07±8.4). The number of antenatal care in the PHC ranged from 1 to 9.
A further statistical analysis was applied to predisposing, reinforcing and enabling factors that had been previously proven as statistically significant. Table 3 shows the results. Factors determining the use of HIV screening were self-confidence of getting blood drawn for HIV screening and the past use of midwife’s service (Table 3).
Table 3. Results of multiple binary logistic regressions of previously shown significant factors on HIV screening service use
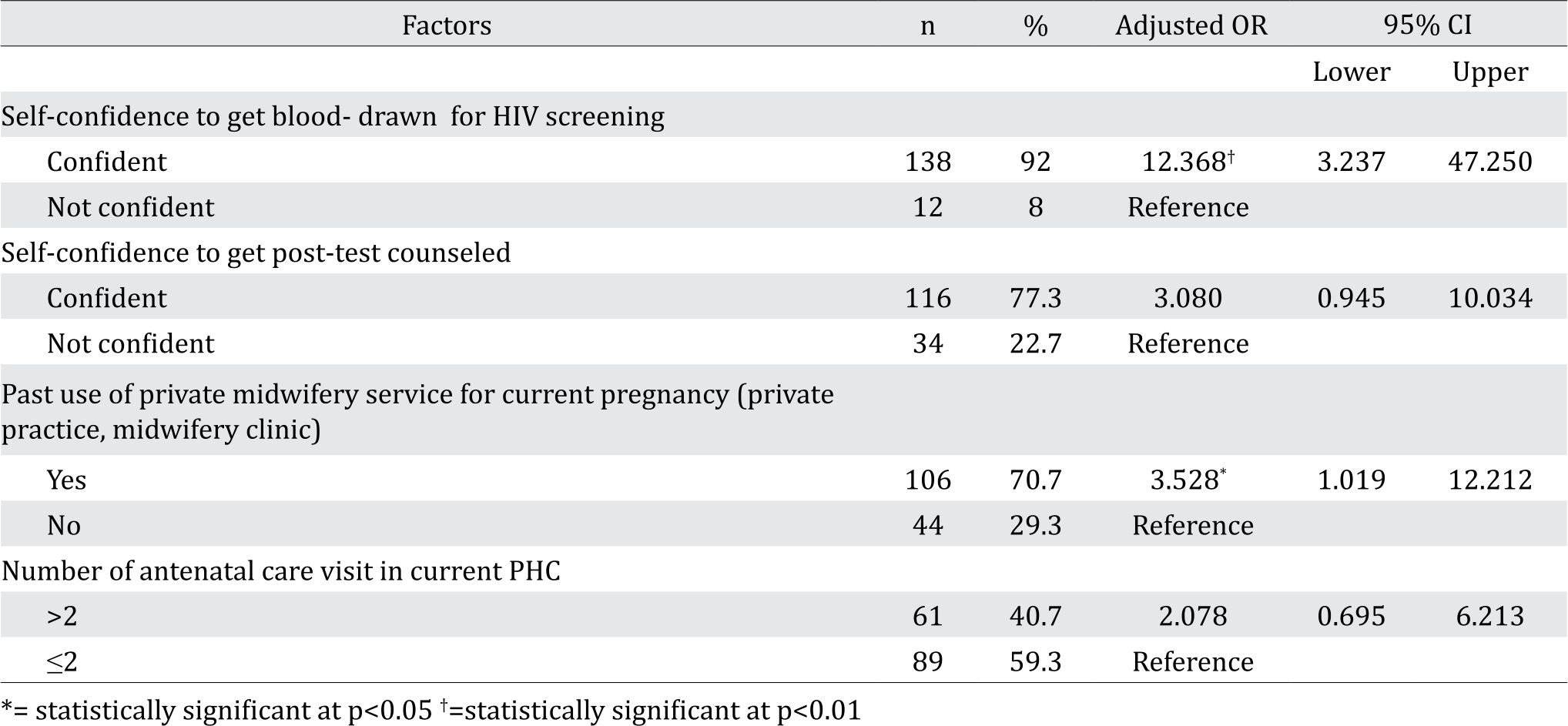
The procedure of Baron and Kenny16 was run, resulting in the mediating effect of self-confidence over the effect of prior use of midwife’s service on HIV screening use, meaning that prior use of midwife’s service affected self-confidence, then the later affected HIV screening use.
DISCUSSION
The shift in policy from HIV VCT to PITC in Surabaya most likely contribute to involuntary increased acceptance as was found in a systematic review of 10 studies in the US, Scotland and 7 African countries comparing HIV PITC screening and VCT. The non Surabayan studies revealed that the acceptance of HIV VCT versus PITC ranged from 34.8% to 99.9% versus 5.5%–78.7%.8 The study did not explore aspects that influenced the increased acceptance. In this study, the use of HIV PITC screening service in PHC was higher than it was at the beginning of this study (70% vs 86% among this study participants), indicating that there was an increased adoption of free HIV screening among pregnant women over time. According to the 2015 report, there was also an overall increase to 17,027 acceptances or 76% of the women attending antenatal care offered in PHC or 40% of overall pregnant women in Surabaya.17 However, the adoption may not fit with stages of change according to diffusion of innovation theory18, i.e gradual acceptance of an innovation change through persuasion. Diffusion of innovation theory may be more suitable for voluntary counseling and testing (VCT). In line with national policy, the Surabayan HIV PITC is introduced to pregnant women attending antenatal care as a routine examination like the existing hepatitis B, STI screenings and nutritional assessment, in which an informational session is included but the procedure of pre- HIV-test counseling is omitted. Pregnant women who choose to opt-out will be advised to attend VCT sessions where pre-HIV-test counseling is provided regardless the women’s decision to take the test. Compared to HIV PITC by pregnant women at its initial phase of study among urban Ethiopian (65.5%)19 in 2007 and Kenyan (84% )20 in 2008, the Surabayan figure in this study was higher. The difference might due to the different settings, i.e. Surabaya is a low prevalence with concentrated epidemic HIV setting, while in urban Ethiopia the prevalence was 7.7% and rural Kenya (15%). The increasing rates of acceptance of PITC HIV at the end of this Surabayan study was (16% in 10 months) almost similar to the Kenyan’s study (14% in 9 months), regardless of the epidemic setting differences. In Cambodia, Myanmar, Nepal, Papua new Guinea, Thailand and Vietnam, pregnant women who knew their HIV status, implying their use of VCT service, were 74%, 35%, 13%, 24%, 94% and 52% respectively.20 Although those Asian countries have more or less ethnic similarities with Surabayans, several governments of the studied countries might not see that PITC HIV policy was urgently needed as VCT was sufficiently accepted or there was limited manpower resources in case of countries the lower acceptance of HIV testing.
Much has been relied to formal education advancement for remedies to health issues. In this study as well as the Ethiopian study,19 however, education was not essential in increasing HIV PITC uptakes. Additionally, lack of education on HIV for pregnant women in this study did not associate with HIV PITC uptakes. Further, these findings also confirmed by lack of difference between general knowledge scores of those who refused and agreed to take HIV test. In fact, the policy of HIV screening in antenatal visit does not mention about health workers’ obligation prior to HIV testing to elevate women’s knowledge about HIV transmission in general, mother-to-child HV transmission and medication to prevent motherto- child transmission.2
More frequent antenatal visits at PHC are also expected to build more pregnant women’s trust towards health workers in PHCs, but this was not the case in this study. There was no association between antenatal visit frequency and HIV PITC test uptake found in this study. Interestingly, the test uptake significantly associated with prior antenatal visits to midwives at private practice sites as well as midwifery clinics outside PHCs, general clinics and general hospitals. Midwives’ service at these private practices and midwifery clinics usually are small and exclusively designed for maternal services, offering more intimate communication between midwives and patients, and among patients. These midwives are bounded to their professional organization’s commitment to send their patients to PHC. Visits to physicians’ solo private practices did not relate to test uptakes although it offers more private doctorpatient communication, most likely because the physicians are not interested in sending pregnant women to PHCs for HIV tests, as private physicians know that they are perceived more valuable by the Indonesian community than the more affordable public services at PHCs. In addition, the medical doctor professional organization does not have commitments to send pregnant women to PHCs in support of government’s free HIV test policy. These findings are different from the Ethiopian study’s19 where antenatal visit frequency significantly associated with the test uptake in clinics and hospital. The difference might be due to the higher HIV prevalence in Ethiopia that leads to more rigorous testing policy, including patient-health worker communication in the pre- HIV-test counseling.
This study revealed that test uptakes significantly related to self-confidence to get blood drawn for HIV test. With an adjusted OR of 12.368, selfconfidence to get blood drawn was the most important factor for the test uptake. Again, trust might have a role in that self-confidence development gained from more intimate communications between midwives and patients in for women only facilities. From the trust gained, midwife might encourage patients to take an HIV test that cannot be more painful than to get blood drawn like in other existing antenatal laboratory tests. While mother-to-child HIV transmission may be halted through increased HIV PITC testing and medication, incomplete-consented patients for this testing can be an ethical issue.
C Framework that was applied in this study considered both husband’s and midwife’s roles. However, this study did not find the role of husbands on the women’s decision to take HIV screening. In Indonesia, detailed domestic health businesses within the households have traditionally belonged to female’s domain. This is different from results of other studies conducted in other areas of similar epidemic level9,10 that underlined the husbands’ or male partners’ role of discouraging women’s decision to take HIV screening. In those studies, worry about husbands’ disapproval to take HIV test was the reason of declining the test, implying that the husbands doubted the institutions credibility or already knew about the consequence of being tested positive. In Kenya, where HIV prevalence is higher than Surabaya, anticipated stigma from male partners was strongly associated with HIV test refusal.11
In line with our study findings, husbands may be targeted by the PHC to increase their wives’ antenatal HIV screening at PHCs as husbands’ reminder is important to the wives to get to the PHCs. Efforts to generate more knowledgeable husbands needs to be carefully designed in order to support pregnant women’s decision in such ways that will not result in women’s discouragement on using HIV screening service.
The implementation of HIV screening policy could be improved if midwife service is expanded to HIV education for women so that their selfconfidence to take HIV test will also be developed based on increased knowledge in addition to trust or other non-rational processes. Inside the PHCs, an already missed opportunity of educating pregnant women about HIV before HIV test should be recaptured by providing an information session or distributing printed materials.
The contrasting results of this study compared to previous studies’ suggest that midwives in urban, concentrated HIV epidemic region of Surabaya can be better prepared to boost pregnant women’s selfconfidence in order to increase the HIV screening uptake. The service of midwives in their private practice has not been covered by the national health insurance scheme through direct financing, but rather through their networking with primary care institutions. This issue should be addressed by including midwives’ service to improve access that may lead to increased HIV PITC use.
The extrapolation of the study results may be limited to urban primary health centers where midwives’ services are available in solo private practices, primary health cares and midwifery clinics. The external validity of the study may be improved through random sampling. In addition, the study was cross-sectional in nature. Hence the directions of associations remain vague. A bigger sample size may be needed to avoid under-power. As only 40% pregnant women used antenatal services in PHC, studies on HIV PITC screening in other primary health care facilities are needed. Physician’s role in advising pregnant women to get HIV checks at PHC needs to be studied.
In conclusion, HIV PITC screening use was affected by a predisposing factor, i.e self-confidence of getting blood drawn for HIV test. The selfconfidence was affected by past use of midwife’s service affected on HIV screening use. The use of HIV screening service at PHCs may be indirectly improved by increasing husbands’ involvement in reminding their wives to get their health checked.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
The authors would like to express their gratitude to Surabaya Health Department for the initial information on the use of HIV screening among pregnant women, the President of Universitas Airlangga for providing the study fund and the participants of this study. The gratitude is also extended to Prof. P.J. van den Broek for his advice on this manuscript’s initial development. The funding was granted by BOPTN Universitas Airlangga nr 1047/UN3.6/KU/PPK/2014
REFERENCES
- Ministry of Health of the Republic of Indonesia [Internet]. Rencana aksi pencegahan penularan HIV dari ibu ke anak (PPIA) - Indonesia 2013-2017. [updated 2015 Sep, 2015; cited 2015 Dec] Available from: http://www.kebijakanaidsindonesia.net/id/dokumenkebijakan/ send/6-publikasi-publication/709-rencanaaksi- nasional-pencegahan-penularan-hiv-dari-ibu-keanak- ppia-indonesia-2013-2017. Indonesian.
- inistry of Health of the Republic of Indonesia [Internet]. Surat Edaran Menteri Kesehatan No. GK/ Menkes/001/I/2013 tentang layanan pencegahan penularan human immunodeficiency virus (HIV) dari ibu ke anak (PPIA). [updated 2014, cited 2015 Dec]. Available from: http://www.kebijakanaidsindonesia. net/id/dokumen-kebijakan/send/17-peraturan-pusatnational- regulation/495-surat-edaran-menkes-ri-no-1- tahun-2013-tentang-layanan-pencegahan-penularanhuman- immunodeficiency-virus-hiv-dari-ibu-ke-anakppia. Indonesian.
- Ministry of Health of the Republic of Indonesia [Internet]. Pedoman nasional tes dan konseling HIV dan AIDS. [cited 2015 Dec 15]. Available from: https:// aidsfree.usaid.gov/sites/default/files/hts_policy_ indonesia_2014.pdf. Indonesian.
- World Health Organization [Internet]. Guidance on provider-initiated HIV testing and counseling in health facilities, 2007. Geneva. [updated 2007 Jun, cited 2015 Dec 15]. Available from: http://apps.who.int/iris/ bitstream/10665/43688/1/9789241595568_eng.pdf
- Surabaya Health Department. Profil kesehatan Surabaya. Surabaya; 2013. Indonesian.
- Surabaya Health Department. Laporan Tiga Bulanan HIV Surabaya; 2014. Indonesian.
- Green L, Kreuter M. Health program planning: An educational and ecological approach. 4th edition. New York, NY: McGraw Hill; 2005.
- Hensen B, Baggaley R, Wong VJ, Grabbe KL, Shaffer N, Lo YRJ, Hargreaves J. Universal voluntary HIV testing in antenatal care settings: a review of the contribution of provider-initiated testing & counseling. Trop Med Int Health. 2012;17(1):59–70.
- Dinh TH, Detels R, Nguyen MA. Factors associated with declining HIV testing and failure to return for results among pregnant women in Vietnam. AIDS. 2005;19(11):1234–6.
- Kwapong GD, Boateng, Agyei-Baffour P, Addy EA. Health service barriers to HIV testing and counseling among pregnant women attending antenatal clinic; a crosssectional study. BMC Health Serv Res. 2014;14:267.
- Turan J M, Bukusi EA, Onono M, Holzemer WL, Miller S, Cohen CR. HIV/AIDS Stigma and Refusal of HIV Testing Among Pregnant Women in Rural Kenya: Results from the MAMAS Study. AIDS Behav. 2011;15:1111–20.
- euro.who.int [Internet]. Towards the elimination of mther-to-child transmission of HIV in low-prevalence and concentrated epidemic settings in Eastern Europe and Central Asia. Geneva, Copenhagen. [updated 2011, cited 2015 Dec 15]. Available from: http://www.euro. who.int/__data/assets/pdf_file/0004/136273/e94882. pdf
- aidsdatahub.org [Internet]. Global AIDS response progress reporting 2014. Construction of core indicators for monitoring the 2011 United Nations political declaration on HIV and AIDS. [updated 2014, cited 2015 Dec 15]. Available from: http://www. aidsdatahub.org/sites/default/files/toolandguide/ document/GARPR_2014_guidelines_en.pdf
- Tufis CD. Multiple imputation as a solution to the missing data problem in social sciences. Calitatea Vieti. 2008;19(1–2):199–212.
- Finch, WH. Imputation methods for missing categorical questionnaire data: a comparison of approaches. J Data Sci. 2010;8:361–78.
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. J Pers Social Psychol. 1986;51(6):1173–82.
- Surabaya Health Department [Internet]. Kunjungi Pelaksanaan Pelayanan Pencegahan HIV ke Anak. [updated 2015; cited 2016 Jan 15] Available from http://dinkes.surabaya.go.id/portal/berita/ kunjungi-pelaksanaan-pelayanan-pencegahan-hivke- anak/
- Rogers EM. Diffusion of Innovation. 5th Ed. New York: Free Press; 2003: 163-206.
- Malaju MT, Alene GD. Assessment of utilization of provider-initiated HIV testing and counseling as an intervention for prevention of mother to child transmission of HIV and associated factors among pregnant women in Gondar Town, North West Ethiopia. BMC Public Health. 2012;12:226.
- Fujita M, Poudel KC, Green K, Wi T, Abeyewickreme I, Ghidinelli M, et al . HIV service delivery models toward ‘Zero AIDS-related Deaths’: a collaborative case study of 6 Asia and Pacific countries. BMC Health Serv Res. 2015;15:176.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id