
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
Effectiveness of combined laser-puncture and conventional wound care to accelerate diabetic foot ulcer healing
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v26i1.1401 Med J Indones. 2017;26:26–34
Received: March 06, 2016
Accepted: April 10, 2017
Author affiliation:
1 Department of Medical Acupuncture, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
2 Department of Internal Medicine, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Corresponding author:
Irma Nareswari
E-mail: i.nareswari@yahoo.com
Background
Impaired wound healing is a common complication of diabetes. It has complex pathophysiologic mechanisms and often necessitates amputation. Our study aimed to evaluate the effectiveness of combined laserpuncture and conventional wound care in the treatment of diabetic foot ulcers.
Methods
This was a double-blind controlled randomized clinical trial on 36 patients, conducted at the Metabolic Endocrine Outpatient Clinic, Cipto Mangunkusumo Hospital, Jakarta, between May and August 2015. Stimulation by laser-puncture (the treatment group) or sham stimulation (the control group) were performed on top of the standard wound care. Laser-puncture or sham were done on several acupuncture points i.e. LI4 Hegu, ST36 Zusanli, SP6 Sanyinjiao and KI3 Taixi bilaterally, combined with irradiation on the ulcers itself twice a week for four weeks. The mean reduction in ulcer sizes (week 2–1, week 3–1, week 4–1) were measured every week and compared between the two groups and analyzed by Mann-Whitney test.
Results
The initial median ulcer size were 4.75 (0.10–9.94) cm2 and 2.33 (0.90–9.88) cm2 in laser-puncture and sham groups, respectively (p=0.027). The median reduction of ulcer size at week 2–1 was -1.079 (-3.25 to -0.09) vs -0.36 (-0.81 to -1.47) cm2, (p=0.000); at week 3–1 was -1.70 (-3.15 to -0.01) vs -0.36 (-0.80 to -0.28) cm2, (p=0.000); and at week 4–1 was -1.22 (-2.72 to 0.00) vs -0.38 (-0.74 to -0.57) cm2, (p=0.012).
Conclusion
Combined laser-puncture and conventional wound care treatment are effective in accelerating the healing of diabetic foot ulcer.
Keywords
accelerate wound healing rate, diabetic foot ulcer, laser-puncture
Diabetic foot ulcer (DFU) is a complicated problem and causes long-term impacts on morbidity, mortality, and quality of life.1,2 Unlike other chronic ulcers, DFU often becomes more problematic due to major changes in diabetic status such as neuropathy and vascular disease.3
In DFU, there is a decrease in wound strength, impaired angiogenesis, and poor wound contraction. Disruption of clot formation, disregulation of inflammatory phase, as well as prolonged and excessive inflammatory response are found in DFU.4,5 Delayed healing DFUs are resistant to conventional treatment.6 Among recent methods in improving wound healing process is the use of low-level laser therapy (LLLT). In-vitro irradiation by LLLT has shown a favorable cell response, including irradiation of diabetic cells.7
Laser-puncture irradiation uses energy of 20 W/cm2, a value equivalent to the effect of stimulation with acupuncture needles,8 so that stimulation of acupuncture points by a needle or laser beam would result in an equivalent effect.8,9 Quah-Smith et al10 indicated that laser-puncture stimulates nerve fibers A-β and non-nociceptive C, while needle acupuncture stimulates the activity of the nerve fibers A-β, A-δ and C (nociceptive and nonnociceptive) that activates precentral gyrus.10
Application of laser-puncture for wound healing would be shorter in time compared to conventional acupuncture.9–11 However, clinical studies on the effects of laser-puncture in promoting ulcer repair have never been conducted in Indonesia. Therefore, the objective of our study is to evaluate the effectiveness of combined laser-puncture and conventional wound treatment compared to sham laser-puncture and conventional wound treatment on the healing of diabetic foot ulcers.
METHODS
This was a double-blind randomized controlled trial on diabetic foot ulcer at the Metabolic Endocrine Outpatient Clinic, Cipto Mangunkusumo National Central General Hospital Jakarta between May and August 2015. The protocol of this study has been approved by the Ethics Committee of the Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital (FKUI-RSCM) (No. 355/UN2.F1/ETHICS/2015). Permission in taking the data was obtained from the Research Division of Cipto Mangunkusumo Hospital (No. LB.02.01/X.2/302/2015). Written informed consent was obtained from each subject before participating the study.
The subjects in this study were recruited by consecutive sampling and were randomized into treatment (laser puncture) and control (sham acupuncture) groups. Inclusion criteria were male or female subjects aged between 18 and 75 years old, with well to moderately controlled type 2 diabetes as confirmed by HbA1c, level, ankle brachial index (ABI) of 0.9–1.3, and had diabetic foot ulcer. The diagnosis of diabetic foot ulcer was based on perfusion, extension, depth, infection, sensation (PEDIS) classification12 (perfusion grade 1 & 2, the extent ≤10 cm2, the depth of grade 1 & 2, infection grade 1 & 2, sensory grade 1 & 2) and the subjects were willing to follow the study schedule as well as to sign the informed consent form. Exclusion criteria were any conditions that require surgical intervention at the site of laser-puncture irradiation, history of malignant tumors, irradiation in the abdominal area for pregnant women, history of untreated epilepsy, irradiation on the retina, and the subject refused to participate in the study. Subject missing two consecutive laser-puncture therapy were dropped out from the study.
Sample size calculation was performed based on formula for two group comparison. The sample size needed for each group was 16 subjects. After an adjustment with anticipation for drop out, 18 subjects were recruited for each group.
Procedures
Measurement of ulcer was performed by the nurses at the Metabolic Endocrine Outpatient Clinic who had been trained for wound care management and had no conflict of interest in the study. After cleansing the ulcers with 0.9% saline solution, the subjects who met the criteria would be informed about the study and asked to sign informed consent form if they were willing to participate. Subjects were then subjected to history-taking (age, gender, health insurance, education, employment, and duration of diabetes, ulcer duration, causes of ulcers, ulcers locations), physical examination (general condition, consciousness, blood pressure, pulse, respiratory rate, temperature), foot and ulcer examinations (in accordance with the classification of PEDIS on inclusion criteria and ankle brachial index (ABI)), laboratory examinations (HbA1c, fasting-and two hours post-prandial blood glucose), and ulcer photo documentations.
Characteristics of ulcer based on PEDIS classification
Determination of PEDIS classification for measuring ulcer carracteristics are as follows.12 Degree of perfusion was classified as grade 1 and 2, where grade 1 showed no symptoms or sign of peripheral arterial disease (PAD) in the affected foot, in combination with palpable dorsal pedal and posterior tibial artery, while grade 2 showed symptoms or sign of PAD, but not of critical limb ischemia. The extent of the wound should be ≤10 cm2 as measured after debridement. The depth of wound or tissue loss was classified as grade 1 with superficial full-thickness ulcer, not penetrating any structure deeper than the dermis, and grade 2 was deep ulcer, penetrating below the dermis to subcutaneous structures, involving fascia, muscle or tendon. Infection category was defined as grade 1 when no symptoms or sign of infection, and grade 2 that involved infection of the skin and subcutaneous tissue. In sensation category, this study assign sensation category as grade 1 when no loss of protective sensation on the affected foot, and grade 2 with loss of protective sensation on the affected foot.12 However, no information on the cause of the loss of protective sensation, nor the severity of the sensory loss were obtained.
Ulcer measurement
Healing of each ulcer was evaluated by digital photography. Ulcer area in each photograph was then measured using ImageJ® software. For this analysis, the edge of each ulcer, i.e. the junction between full thickness skin and the ulcer was first delineated, and then the computer automatically computed the area of each ulcer. Repeated measurements were performed on a weekly basis for four weeks, and the reduction of ulcer area was compared between the treatment group and the control group.
Treatment
Subjects in the treatment group received combined laser-puncture and conventional wound care, while those in the control group received sham laser-puncture combined with conventional wound care. The laser-puncture on acupuncture points was performed according to stimulation method using laser pen instrument of low-level diode laser (MicroPAD Gl+™) with 630 nm wavelength, red light, resonance mode, power 100 mW, at dose of 4 Joule for one minute with contact technique. In addition, low-level laser therapy stimulation on diabetic ulcer was done by a stimulation method using laser pen instrument of low-level diode laser (MicroPAD Gl+™) on the ulcer site by non-contact scanning technique, i.e. the distance between the tip of laser pen and the tissue was maintained at 5 mm. The laser pen was then guided by hand to stimulate all of wound tissue. The duration of laser radiation for the wound on the foot depended on the extent of wound, i.e. wound area of ≤3 cm2 required two minutes and 55 seconds of treatment; while for the wound area of 4–6 cm2, the treatment was conducted for five minutes and one second, and for the wound area of 7–9 cm2, eight minutes and five seconds were necessary. For the subjects in the control group, the laser pen instrument was directed on the site of diabetic foot ulcer and the instrument was attached to the acupuncture points, i.e. the LI4 Hegu, ST36 Zusanli, SP6 Sanyinjiao and KI3 Taixi points; however, the laser was not activated. Laser-puncture therapy was performed twice a week for eight times during the four weeks of therapy.
For the purpose of safety, all patients were instructed to wear safety goggles as well as the researcher. Since LLLT provides no sensory cues such as thermal or acoustic effect, wearing goggles also blinded the patients to the procedure of LLLT at the same time.
Statistical analysis
Comparisons of paired numerical variables with normal distribution were done using paired T test, or Wilcoxon test when data distribution is not normal. The difference of wound area each week were analyzed with Mann Whitney test. All statistical procedure were conducted using SPSS 11.5 software.
RESULTS
This study was conducted on 36 patients with diabetic foot ulcers who met the inclusion and exclusion criteria. Subjects were randomly divided into two groups of 18. Subjects participated in the study for four weeks, and no subject dropped out until the study completed.
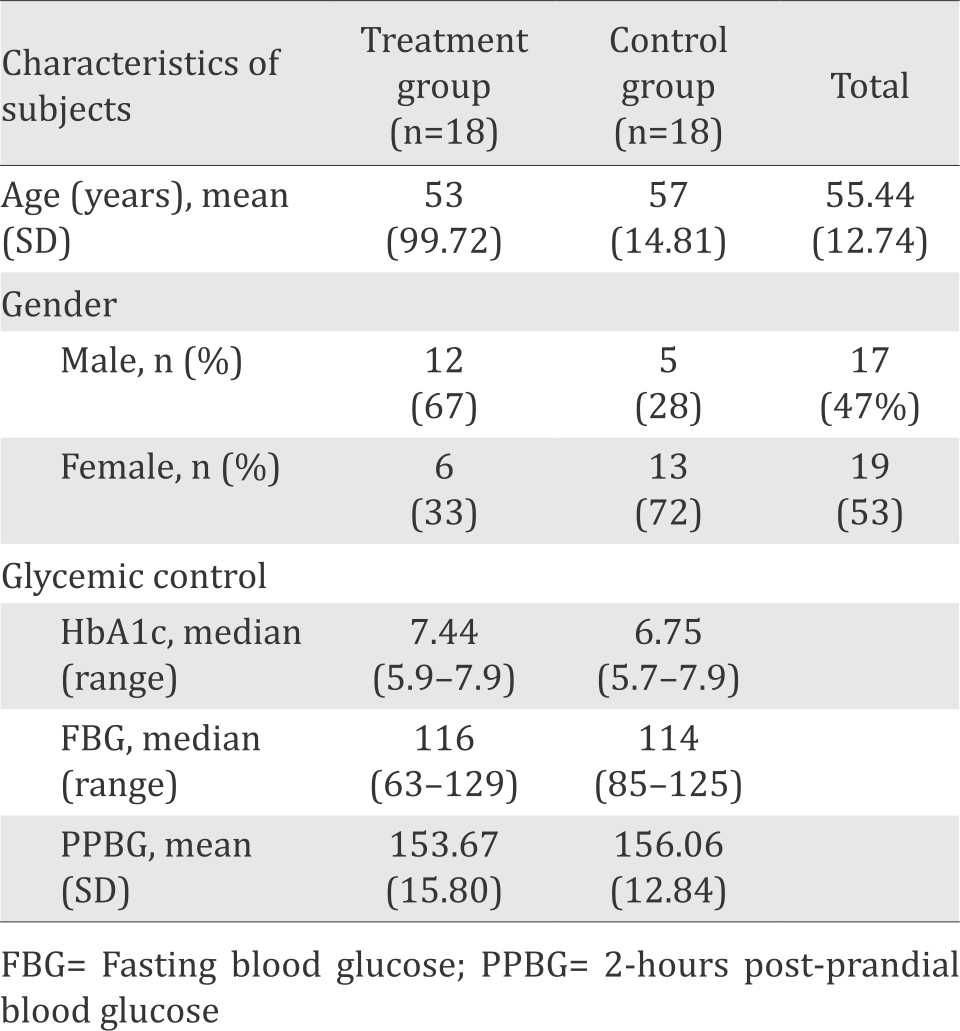
Subjects characteristics
The mean age of the study subjects was 55 years old and most of them (52.83%) were female. HbA1c, fasting blood glucose and two hour post-prandial glucose showed that both groups were well to moderately controlled diabetics (Table 1).
Table 1. Characteristics of subjects
Most of subjects had diabetic foot ulcer for less than three months at the time of entering the study. Spontaneous ulcers appeared in 22 subjects, followed by mechanical trauma and thermal trauma as the cause of diabetic foot ulcer. There was a significant difference in ulcer location (p=0.041), with plantar side as the most prominent location.
In this study, criteria of perfusion was represented by the median value of ankle brachial index (ABI) that was 1.09 (ranged 0.93-1.23). Mann Whitney test showed no significant difference between the treatment group and the control group in the depth, infection, and sensory (p=0.897) categories.
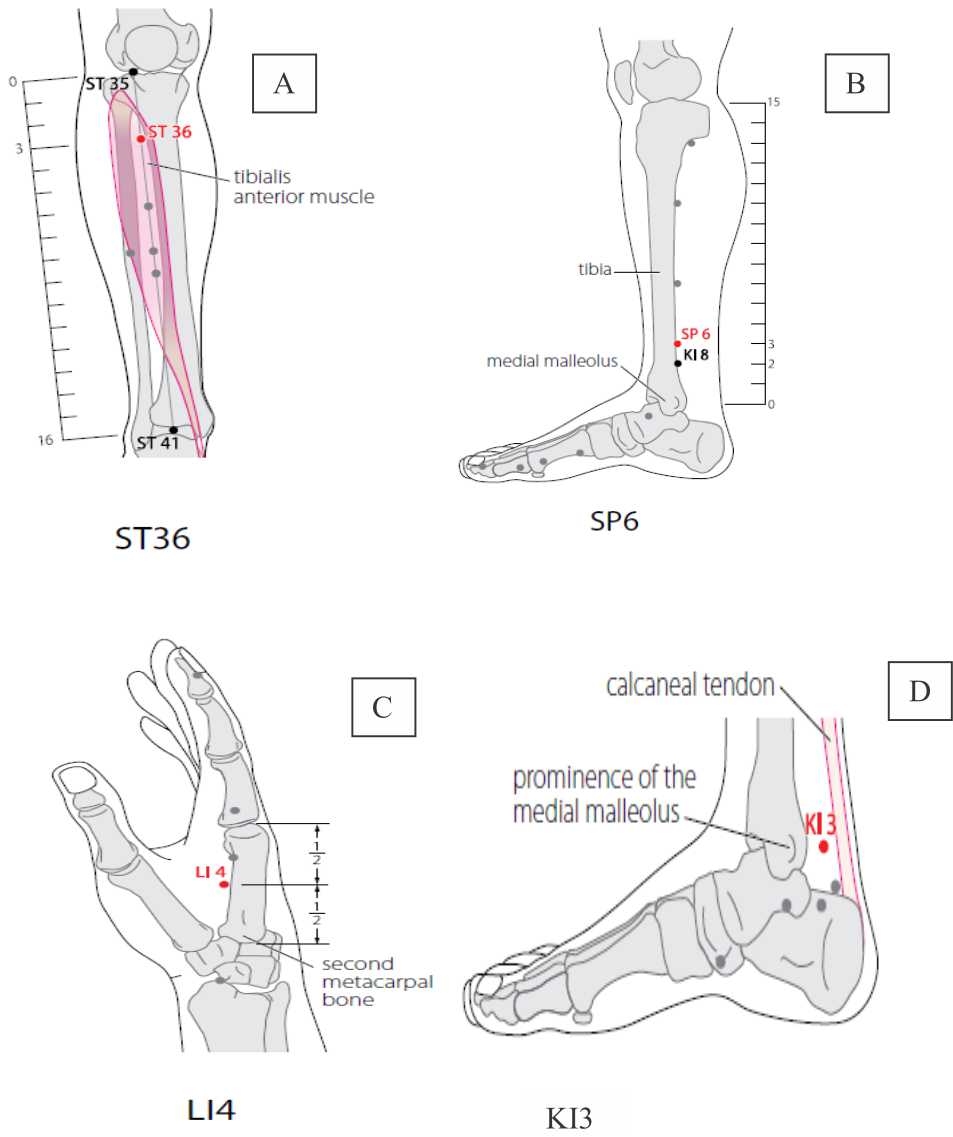
Figure 1. Location of acupuncture points based on the World Health Organization standard acupuncture point locations in the Western Pacific region. 2008. A. ST26 Zusanli. B. SP6 Sanyinjiao. C. LI4 Hegu. D. KI3 Taixi
Evolution of wound size
Mann Whitney test showed a significant difference in initial wound size between the treatment group {4.75 cm2 (0.10–9.94)} compared to the control group {2.33 cm2 (0.90–9.88)} (p=0.027) (Table 2). However, the wound in the treatment group healed faster and at the end of the study, the wound in the treatment group {0.24 cm2 (0.00–2.54)} became significantly smaller compared to the control group {1.25 cm2 (0.00–8.11)}. Figure 2 shows that the weekly reduction of wound area is consistently higher in the treatment group compared to the control group. No adverse effect of any kind was reported as a result of the treatment.
Table 2. Characteristics of diabetic foot ulcer of subjects
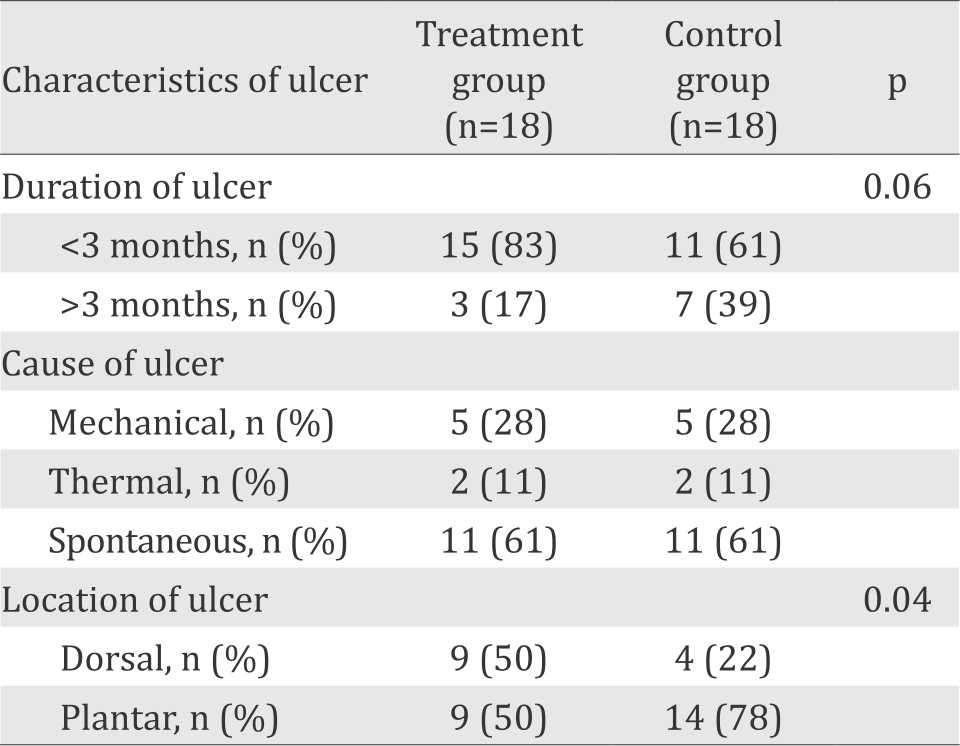
Table 3. The comparison in median wound area every week between the treatment group and the control group
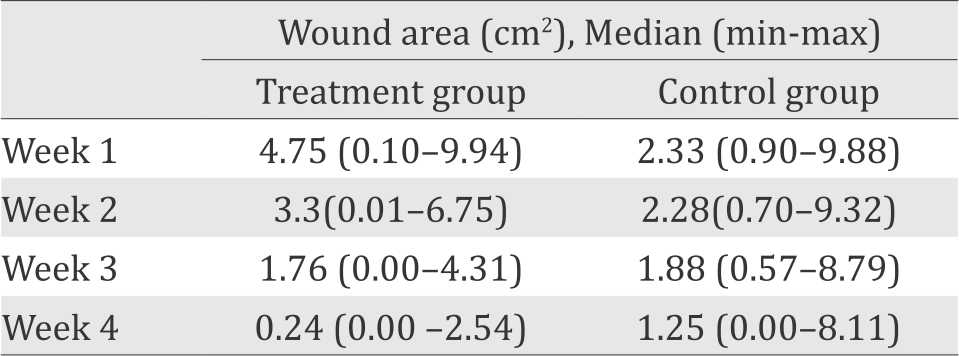
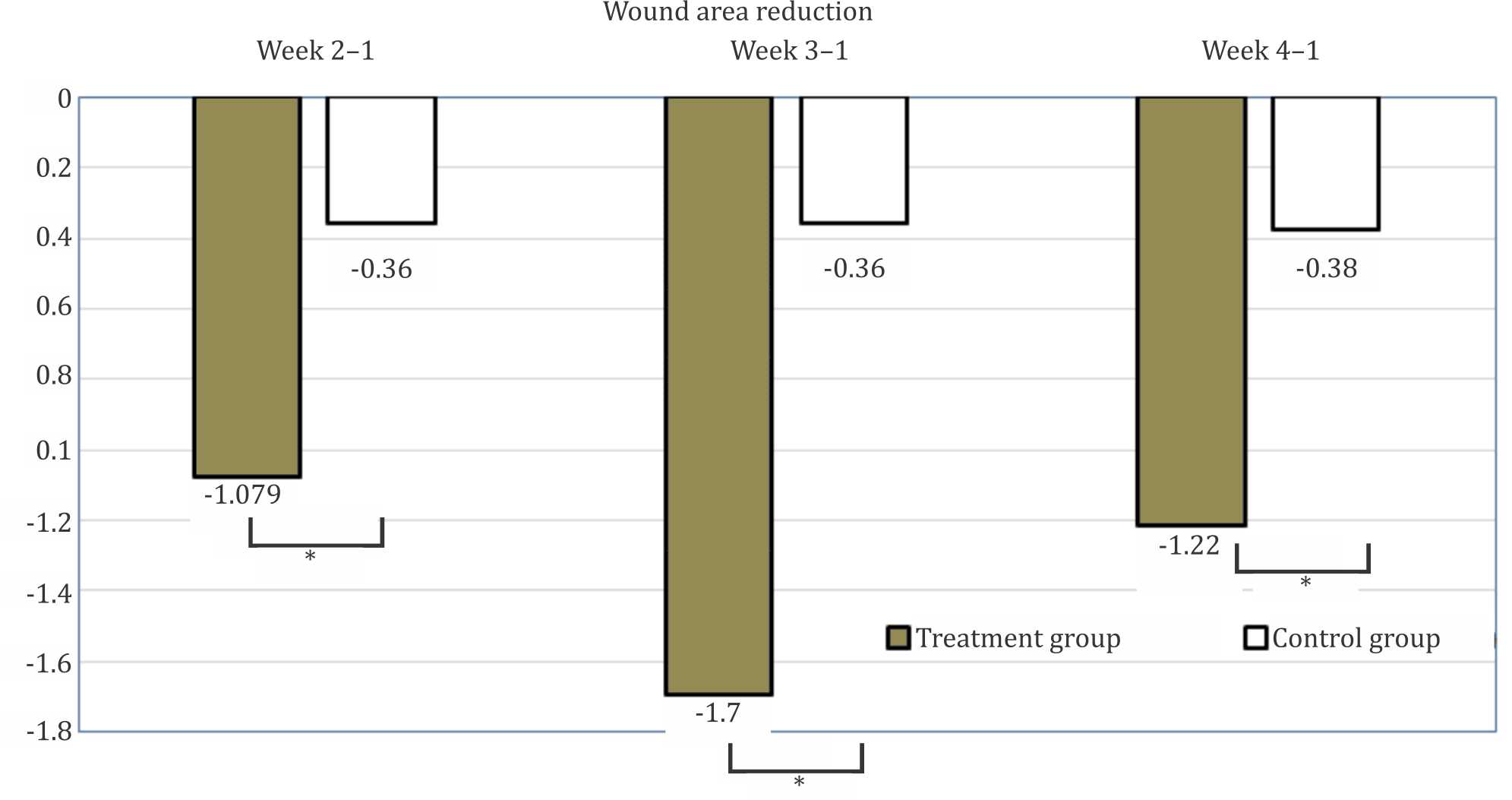
Figure 2. Median of wound area reduction in treatment and control group. *p<0.05 treatment vs control group
DISCUSSION
Assessment of diabetic foot ulcers in this study was based on PEDIS classification, where perfusion assessment categories represented by ABI values as well as on the categories of depth, infection, and sensation between the two groups showed no significant difference. This classification was choosen because it is routinely used to classify DFU at the Metabolic Endocrine Outpatient Clinic, Cipto Mangunkusumo National Central General Hospital, Jakarta, and this classification is also suggested by the International Working Group of the Diabetic Foot (IWGDF).
Most of the subjects in this study were unemployed and used government insurance to pay the DFU care. The frequencies of wound care covered by the insurance were only twice a week, so this study adjusted the timing of therapy according to this regulation in an effort to maintain compliance of the study subjects. Most of the subjects were female, with the mean of age 55 years and worked as housewives. A study conducted by Wibowo13 also showed the same result, that most patients found in the Outpatient Clinic of Metabolic Endocrine were females and worked as housewives.13 This data was essential because when a patient needed to increase the frequency of wound care, they had to pay for the treatment. Therefore, laser-puncture was expected to be an adjunct therapy in conventional wound care, in order to accelerate wound healing.
In this study, the subject characteristics (age and gender) showed no significant difference between the treatment group and the control group. Thus, in these terms, the groups could be regarded as equal. A dissertation by Waspadji14 found some of the factors influenced the occurrence of DFU including lower education (OR=2.29, p=0.016) and low socio-economic conditions (OR=2.64, p=0.005). These conditions were associated with less knowledge about diabetes and its complication prevention, also less financial capacity to seek proper treatment.14 In this study, the conventional wound care obtained by subjects at the hospital was only twice a week, and subjects should be able to treat the ulcer by themselves at home. In order to maintain proper wound care, education should be shared with family members caring for the subjects at home, especially for the subjects with a history of low education. Another characteristic of subjects was glycemic control that was categorized as good and moderate based on the value of HbA1c, fasting blood glucose, and two-hour-post-prandial glucose, which results did not differ significantly between the two groups. Christman et al15 specifically proved that for every 1.0% increase in HbA1c value, the rate of healing ulcer area decreased daily by 0.028 cm2/day; thus metabolic factor also influenced the rate of wound healing.
In this study, the characteristics of ulcer duration and location of ulcers in diabetic foot ulcers showed no significant difference between the two groups. The most common cause of ulcer emergence in this study was spontaneous, which could be related to the most common etiology of diabetic foot ulcers that is neuropathy.16 Another cause of ulcer emergence was sensory loss16 that led to thermal and mechanical injuries. The most prominent side of ulcer location was plantar side, but in this study, the total reduction in ulcer area was not affected by the location of the ulcer. Mechanical controls also affected the speed of ulcer healing because it aimed in resting the injured leg. Therefore, the foot could avoid constant pressure when walking.17 Although plantar side was the location of most ulcers, there were still subjects that did not rest the injured leg side, which might be due to shyness or financial limitation to buy a walking aid. In addition, initial wound size was significantly different, in which the treatment group showed larger wound areas.
The result of this study after intervention showed a reduction in median wound area from the initial measurement, on the second and third week until the final measurement. On the initial wound measurement, the median of the treatment group was larger than the control group (p=0.003). However, median wound size of the treatment group was smaller compared to the control group at the end of the measurement. It can be explained by the difference of wound area that measured every week. The velocity of wound healing was faster in the treatment group than the control group. Therefore, it could be concluded that wound healing was much faster under laserpuncture compared to sham puncture.
The results of this study differed from the study of Wibowo13 which showed no significant difference between the two groups until fifth weeks of treatment. The present study used similar intervention as used by Wibowo13 i.e. with the frequency of twice a week. However, in our study the radiation was not only limited to ulcer area, but also to the acupuncture points including the LI4 Hegu, ST36 Zusanli, SP6 Sanyinjiao, and KI3 Taixi points bilaterally. Therefore, we can conclude that the addition of acupuncture points was effective in accelerating the healing of diabetic food ulcer.
Kaviani et al18 conducted a preliminary study in 23 subjects randomized to receive LLLT therapy (685 nm, energy density of 10 J/cm2, 200 sec, power density 50 mW/cm2) and conventional therapy, six times per week for at least two successive weeks and then every other day up to complete healing with non-contact irradiation technique. The results accessed on the fourth week showed that the wound size was significantly smaller in the group of LLLT. After 20 weeks, there were eight subjects who had complete healing in LLLT group, whereas it was only three subjects in the placebo group.18 Our treatment time was limited by the regulations of insurance. Taking into account the possible difficulties of subject’s compliance, we decided to provide therapy twice a week. Although the total of our treatment time was only eight sessions in four weeks, our results showed that laser-puncture played a significant role in accelerating the healing of DFU.
A randomized clinical trial by Minatel et al19 also provided evidences that a twice-weekly radiation showed significant results in the treatment group with increased healing time for diabetic foot ulcer as much as 79.2% and a 56% increase of granulation in the treatment group. On the 90th day, 58.3% subjects in the treatment group reached complete healing, and 75% subjects had 90-100% healing.19 Ulcer area and the area of granulation in the study of Minatel et al19 was measured using ImageJ software, the same software that was used in our study. However, the area of granulation was not included as an outcome in our study even though this variable can be used to measure tissue repair by exploring the relationship between the rate of tissue granulation and wound closure rate, and this fact was a limitation of our study. Moreover, both studies could not measure or determine ulcer volume even though by digitally and computerized photograph to obtain precise computation of ulcer sizes. Therefore, further studies is needed to assess these variables.
A case report conducted by Kazemi-Khoo20 had shown that a radiation on LI11 Quchi, LI6 Pianli, SP6 Sanyinjiao, PC6 Neiguan, ST36 Zusanli and GB34 Yanglingquan acupuncture points provided a complete healing after an average of 19 times treatment on seven subjects. Based on the report, the wound healed completely in three months, which means with higher frequency of therapy. Moreover, they also used various intervention methods such as shower laser, intravenous laser, and laser-puncture.20 In addition, laser tools used by Kazemi-Khoo20 had also more variables in dealing with these cases, including the use of intravenous laser, which required high caution, and was not available in our study.
Kajagar et al6 had performed an intervention to 68 patients with diabetic foot ulcer every day for 15 days, and they found a significant difference between the treatment group and the control group regarding the mean reduction of ulcer area. All ulcers in both groups belonged to Meggitt-Wagner grade I and had a depth of 5 mm, so the ulcers were superficial and did not involve tendon.6 However, in our study, we used PEDIS classification for ulcer characteristics and to categorize the grading of ulcer depth, we used grade 1 and 2 which involved not only superficial ulcer, but also muscle and tendon. The ulcer size in the study by Kajagar et al6 was larger than our study which is 6x6 cm2 with the duration of exposure of 2–4J/cm2 at 60 mW, 5 kHz. This result showed that LLLT was an effective modality to enhance wound healing in patients suffering from diabetes and could be used as an adjunct to conventional mode of treatment for healing of diabetic wounds.
One of the reasons of the point selection is based on the etiology of diabetic foot ulcers, which are neuropathy, ischemia, and neuro-ischemia that can affect healing. Yotsu et al21 showed that the most common cause of DFU is neuropathy, and this study was done in 73 DFU patients. This finding is one of the reasons for researchers to choose the acupuncture points that have a role on diabetic neuropathy. Based on a systematic review by Chen et al22 acupuncture points most often used in dealing with diabetic neuropathy are ST36 Zusanli, GB34 Yanglingquan, SP6 Sanyinjiao, KI3 Taixi on the lower extremities, whereas in the upper limb are LI11 Quchi, LI4 Hegu, SJ5 Waiguan, and PC6 Neiguan. Kim et al23 conducted another systematic review on several experimental studies to see the effect of electro-acupuncture on neuropathic pain. This study showed that stimulation of acupuncture points ST36 Zusanli and SP6 Sanyinjiao could activate μ and δ opioid, GABA-ergic, cholinergic, and 5-HT3 serotonergic receptors in the central nervous system, which not only played a role in various areas of pain,23 but also in the cellular mechanisms of laser-puncture on wound healing.4 In addition, the stimulation on ST36 Zusanli and SP6 Sanyinjiao acupuncture points may affect connective tissue through mechanical forces transferred to the extracellular matrix. Using the extracellular matrix (ECM), the mechano-tranduction can be translated from the acupuncture points, which involves local tissues and cells. Cells in the local tissues that have received mechano-transduction induce various kinds of nitrite oxide (NO) production that can cause changes in systemic and local circulation.6 The ST36 and SP6 points have also been proven to have a role in suppressing the production of various inflammatory cytokines such as interleukin-6 (IL-6) and interleukin-10 (IL-10) and in stimulating endogenous antioxidants, superoxide dismutase (SOD), and glutathione peroxidase (GPx).24 Reduced inflammation and stress oxidative process can also suppress the production of proteinase such as matrix metalloproteinase (MMP).25
Stimulation of acupuncture point LI4 Hegu was shown to affect microvascular perfusion and significantly regulate body’s blood flow as described by Huang et al26 Moreover, Peplow et al27 showed the effect of stimulation of point KI3 Taixi, which could lower blood sugar and improve insulin sensitivity, and affect blood flow in the feet. The study by Chen et al22 revealed another role of KI3 Taixi point that affected sensory nerve conduction velocity, as well as in motor peroneal and median calf nerves in cases of diabetic neuropathy. Moreover, the stimulation by laserpuncture on LI4 Hegu and KI3 Taixi points also have anti-inflammatory effects that may help in accelerating wound healing. In addition, there is supression of inducible nitric oxide synthase (iNOS) production and increase in production of neuronal nitric oxide synthase (nNOS) and endothelial nitric oxide synthase (eNOS).6,28,29 The production of nNOS and eNOS has a positive role in NO production, which causes vasodilatation and increases blood circulation that may lead to acceleration of wound healing.6
The limitations of our study were the absence of biomarker examination that can support patophysiology and mechanism of action of the acupuncture. Therefore, further studies are needed to address these issues into consideration. Longer study period is also necessary to monitor complete healing in all study subjects of diabetic foot ulcer.
In conclusion, the combined laser-puncture and conventional wound care treatment was effective in accelerating the healing of diabetic foot ulcer.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Best practice guidelines: Wound Management in Diabetic Foot Ulcers (Update 31 March 2017, Cited 23 October 2015). London; 2013. Available from: http://www.woundsinternational.com/media/ bestpractices/_/673/files/dfubestpracticeforweb.pdf
- Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366(9498):1719–24.
- National Institute for Health and Clinical Excellence. Diabetic foot problems: inpatient management of diabetic foot problems. London: NICE; 2011. p 9–27.
- Houreld NN. Shedding light on a new treatment for diabetic wound healing: a review on phototherapy. Scientific World Journal. 2014;2014:398412.
- Brem H, Tomic-Canic M. Cellular and molecular basis of wound healing in diabetes. J Clin Invest. 2007;117(5):1219–22.
- Kajagar BM, Godhi AS, Pandit A, Khatri S. Efficacy of low level laser therapy on wound healing in patients with chronic diabetic foot ulcers-a randomised control trial. Indian J Surg. 2012;74(5):359–63.
- Gao X, Xing D. Molecular mechanisms of cell proliferation induced by low power laser irradiation. J Biomed Sci. 2009;16(1):4.
- Schikora D. Laserneedle acupuncture: a critical review and recent results. Medical Acupuncture. 2008;20(1):37–42.
- Kreisel V, Weber M. In: A Practical Handbook Laser Acupuncture. 1st ed. High-Tech Acupuncture with Laser Light. Fuchtenbusch. 2012. p. 14–33.
- Quah-Smith I, Williams MA, Lundeberg T, Suo C, Sachdev P. Differential brain effects of laser and needle acupuncture at LR8 using functional MRI. Acupunct Med. 2013;31(3):282–9.
- Round R, Litscher G, Bahr F. Auricular acupuncture with laser. Evidence-Based Complementary and Alternative Medicine. 2013;2013:984763.
- Schaper NC. Diabetic foot ulcer classification system for research purposes: a progress report on criteria for including patients in research studies. Diabetes Metab Res Rev. 2004;20(1):90–5.
- Wibowo RI [Thesis]. Pengaruh stimulasi low level laser therapy terhadap proses penyembuhan ulkus kaki diabetes. Jakarta: Universitas Indonesia. 2009. p. 21–57. Indonesian.
- Waspadji S [Dissertation]. Telaah mengenai hubungan faktor metabolik dan respon imun pada pasien diabetes melitus tipe 2: kaitannya dengan ulkus dan ganggren diabetik. Jakarta: Universitas Indonesia. 2000. p. 83– 110. Indonesian.
- Christman AL, Selvin E, Margolis DJ, Lazarus GS, Garza LA. Hemoglobin A1c is a predictor of healing rate in diabetic wounds. J Invest Dermatol. 2011;131(10):2121–7.
- Cook JJ, Simonson DC. Epidemiology and health care cost of diabetic foot problems. In: Veves A. et al, editors. The diabetic foot: medical and surgical management, contemporary diabetes. New York: Springer ScienceBusiness Media. 2012. p.17–32.
- Pengurus Besar Perkumpulan Endokrinologi Indonesia (PB. PERKENI). Pedoman Penatalaksanaan Kaki Diabetik. In: PB. PERKENI. Pendekatan diagnostik kaki diabetes dan Penatalaksanaan holistik kaki diabetes. Jakarta: PB. PERKENI. 2009. p. 5–19. Indonesian.
- Kaviani A, Djavid GE, Ataie-Fashtami L, Fateh M, Ghodsi M, Salami M, et al. A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg. 2011;29(2):109–14.
- Minatel DG, Frade MA, França SC, Enwemeka CS. Phototherapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med. 2009;41(6):433–41.
- Kazemi-Khoo N. Successful treatment of diabetic foot ulcers with low-level laser therapy. The Foot. 2006;16(4):184–7.
- Yotsu RR, Pham NM, Oe M, Nagase T, Sanada H, Hara H, et al. Comparison of characteristics and healing course of diabetic foot ulcers by etiological classification: neuropathic, ischemic, and neuro-ischemic type. J Diabetes Complications. 2014;28(4):528–35.
- Chen W, Yang GY, Liu B, Manheimer E, Liu JP. Manual acupuncture for treatment of diabetic peripheral neuropathy: a systematic review of randomized controlled trials. PLoS One. 2013;8(9):e73764.
- Kim W, Kim SK, Byung-Il M. Mechanisms of electroacupuncture-induced analgesia on neuropathic pain in animal model. Evid Based Complement Alternat Med. 2013;2013: 436913.
- Wang H, Pan Y, Xue B, Wang X, Zhao F, Jia J, et al. The antioxidative effect of electro-acupuncture in a mouse model of Parkinson’s disease. PLoS One. 2011;6(5):e19790.
- Muller M, Trocme C, Lardy B, Morel F, Halimi S, Benhamou PY. Matrix metalloproteinases and diabetic foot ulcers: the ratio of MMP-1 to TIMP- 1 is a predictor of wound healing. Diabet Med. 2008;25(4):419–26.
- Huang T, Yang LJ, Zhang WB, Jia SY, Tian YY, Wang GJ, et al. Observation of microvascular perfusion in the Hegu (LI4) acupoint area after deqi acupuncture at Quchi (LI11) acupoint using speckle laser blood flow scanning technology. Evid Based Complement Alternat Med. 2012;2012:604590.
- Peplow PV, Baxter GD. Electroacupuncture for control of blood glucose in diabetes: literature review. J Acupunct Meridian Stud. 2012;5(1):1–10.
- Kilík R, Lakyová L, Sabo J, Kruzliak P, Lacjaková K, Vasilenko T, et al. Effect of equal daily doses achieved by different power densities of low-level laser therapy at 635nm on open skin wound healing in normal and diabetic rats. Biomed Res Int. 2014;2014:269253.
- Park SI, Sunwoo YY, Jung YJ, Chang WC, Park MS, Chung YA, et al. Therapeutic effects of acupuncture through enhancement of functional angiogenesis and granulogenesis in rat wound healing. Evid Based Complement Alternat Med. 2012;2012: 464586.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id