
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
Prevalence and risk factors of persistent stress urinary incontinence at three months postpartum in Indonesian women
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v25i3.1407 Med J Indones. 2016;25:163–70
Received: March 13, 2016
Accepted: August 19, 2016
Author affiliation:
1 Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Riau, Pekanbaru, Indonesia
2 Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Corresponding author:
Edy Fakhrizal
E-mail: dredy_spog@yahoo.co.id
Background
Mode of delivery and some certain risk factors have a relationship to postpartum stress urinary incontinence (SUI). For that reason, the objective of this study was to assess the prevalence of postpartum stress urinary incontinence (SUI), the relationship between postpartum SUI and mode of delivery; and the association between SUI and other demographic and obstetric factors.
Methods
In this prospective observational cohort study, all primiparous women who were under postpartum care in obstetric and gynecologic ward were recruited. Four hundreds primiparous women with no history of urinary incontinence (UI) who fulfilled the criteria and would like to participate in this study were followed up for three months after delivery. The analysis was done using Stata 12. Bivariate analysis using Chi-square test and multivariate analysis using logistic regression test were done to obtain associated risk factors to postpartum SUI.
Results
The prevalence of postpartum SUI was 8.8%. The mode of delivery was significantly associated with postpartum SUI, there were more women who got vaginal delivery that had stress urinary incontinence (14.1%) compared to women caesarean section (7.1%) with OR=2.1 (95% CI=1.05-4.31), this risk increased when vaginal delivery was assisted with vacuum instrument (OR=9.1, 95% CI=3.9-21.6). There was no statistical difference of stress urinary incontinence incidences in patients with emergency or elective caesarean section with OR=0.84 (95% CI=0.28-2.57). Based on multivariate analysis BMI ≥30 kg/m2 at labor, vacuum assisted delivery, birth weight more than 3,360 g, and second stage labor more than 60 minutes appeared to be associated with an increased rate of postpartum SUI.
Conclusion
Stress urinary incontinence increased in the early postpartum period of a primiparous woman. Although vaginal delivery increased the risk of postpartum SUI, elective nor emergency caesarean delivery without vaginal delivery id not appear to increase the risk of stress urinary incontinence.
Keywords
prevalence, postpartum stress urinary incontinence, risk factor
Urinary incontinence is a worldwide public health problem that affects the life of millions of women and causes serious socio-economical, physical and psychological problems. It will also affect sexual intercourse that causes a decrease in quality of life, depression, and lower self-esteem. Urinary incontinence could harm women’s emotional state, which will cause lower self-esteem and fear of sexual intercourse.1 In a study, it was stated that urinary incontinence, Alzheimer’s disease and stroke were the three chronic diseases that would badly affect and decrease the quality of health.2
World Health Organization (WHO) stated that urinary incontinence was a major health problem, and there were more than 200 million populations in the world having problems with micturition.3 The increasing cost related to urinary incontinence treatment became government’s awareness whereas billions of dollar were issued every year in United States.4,5
Urinary incontinence prevalence among women was about 3-55% depending on the limits and age groups, which were varied in each country due to several factors.6 According to systematic review by Thom and Rortveit7, acquired urinary incontinence postpartum prevalence was 33%, half of whom was stress urinary incontinence prevalence.7 In Indonesia, urinary incontinence prevalence was still unknown because there was an assumption that urinary incontinence was a normal condition in postpartum women and a lot of women tended to feel shy to check their condition to health professionals.8 It was also estimated that the people seek treatment to nonformal health providers, causing a lot of cases unregistered and the data were less accurate. Although this problem was rather disturbing and affected the quality of life, patients rarely seek for medical treatment.9
Stress and urge urinary incontinence are the two most frequent types. Stress urinary incontinence is a type of urinary incontinence related to physical activity, defined by uncontrolled urinary excretion during activity, sneezing or coughing.10 Stress urinary incontinence and prolapsed pelvic organs are common incidence and need to be repaired on operation in 11% women near 80 years old, with a possibility of reoperation as 30%. This incidence is related to vaginal delivery and parity which cause pelvic floor dysfunction.11 Boyles et al showed that the first labor influenced the most towards the mechanism of continence.12 However, it was still questioned whether caesarean section could prevent pelvic floor trauma.1,13–15
In a study, it was reported that women with persistent stress urinary incontinence at three months postpartum, 92% would continue to stress urinary incontinence for five years postpartum.16–18 This study aimed to know the prevalence and risk factors of postpartum stress urinary incontinence (SUI) in Indonesia.
METHODS
This study was an observational cohort study which included all primiparous women who were hospitalized after labor in obstetric and gynecology ward in Arifin Achmad Hospital, Pekanbaru, Riau during July 1st – December 31st 2014. Primiparous women with no history of urinary incontinence (UI) who fulfilled the criteria were recruited. The inclusion criteria were single gestation, gestational age while labor is equal or more than 37 weeks, birth weight more than 2,500 grams, and would like to join this study by signing informed consent form. Then, subjects were asked to fill questionnaire sheet of urinary incontinence called the questionnaire for urinary incontinence diagnosis (QUID)19 validated in Bahasa Indonesia with an assistance from research team who had been trained regarding the filling of QUID questionnaire. The adopted QUID questionnaire was translated by sworn translator and validated by urogynecology consultants in urogynecology division of Cipto Mangunkusumo Hospital (RSCM) Jakarta. Presampling of QUID questionnaire was done in urogynecology clinic at RSCM using 30 random samples and the validation test result was reliable with Cronbach’s alpha value was 0.97 for SUI type questionnaire and 0.96 for urgency urinary incontinence (UUI) type questionnaire.20 Patient’s data regarding demography risk factors likes age, body weight before gestation and during the labor, body masss index (BMI) as well as obstetric risk factors like delivery mode, length of second stage (started from full dilation to expulsion of the baby), baby’s body weight at birth, presence or absence of episiotomy and presence or absence of perineal laceration with its severity were collected from medical record. After that, researcher conducted cough test by himself. Before conducting the test, the subjects were instructed to do a spontaneous micturition followed by drinking two glasses of water (16oz=450ml) and waiting for two hours. After that, subjects were asked for coughing loudly in lithotomy position. Cough test was positive when urinary excretes from external urethral meatus. If there was no urinary excreted from external urethral meatus, then the test was repeated in the standing position. In a monitoring at three months postpartum, subjects were asked to refill QUID questionnaire and we underwent cough test again. Subjects suffering stress urinary incontinence before gestation and having incomplete data were excluded from this study. The protocol of this study has been approved by Ethical Review Board for Medicine and Health research Universitas Riau Faculty of Medicine, Pekanbaru-Riau, Indonesia (No. 10/UN19.1.28/UEPKK/2014).
The analysis of this study was processed with statistic data analysis (Stata) 12. Data distribution of subject was processed by univariate descriptive analysis and presented in number (n) and percent (%), based on the dummy descriptive data table. The relationship between risk factors (demography and obstetric) and postpartum stress urinary incontinence was conducted with bivariate analysis. After that, we conducted a selection for variables that fulfilled criteria to be included into multivariate analysis using stepwise backward method. The p value was significant if it was less than 5% with 95% confidence interval. The results of the analysis were reported in frequency, p value percentage, and odd ratio (OR). After conducting multivariate analysis for independent variable, we conducted calibration test (Hosmer and Lemeshow) and area under curve (AUC) discrimination test.21
RESULTS
During July until December 2014, a total of 447 primiparous women shortlisted by inclusion and exclusion criteria were willing to join this study on the first examination right after their deliveries. In this population, 137 subjects (31.6%) suffered urinary incontinence with distribution of urinary incontinence type as follows: 40 subjects (8.9%) were stress urinary incontinence, 51 subjects (11.4%) were urge urinary incontinence, and 46 subjects (10.3%) showed mixed urinary incontinence. From 447 subjects, 400 subjects (89.5%) were willing to come and complete this study on second examination at three months postpartum. In this population, 81 subjects (20.3%) suffered urinary incontinence, 75 subjects (54.7%) were persistent urinary incontinence at three months postpartum and six subjects (7.41%) were new cases. From 81 population suffering urinary incontinence, 35 subjects (8.8%) were stress urinary incontinence, 25 subjects (6.3%) were urge urinary incontinence and 21 subjects (5.3%) showed mixed urinary incontinence as seen in figure 1.
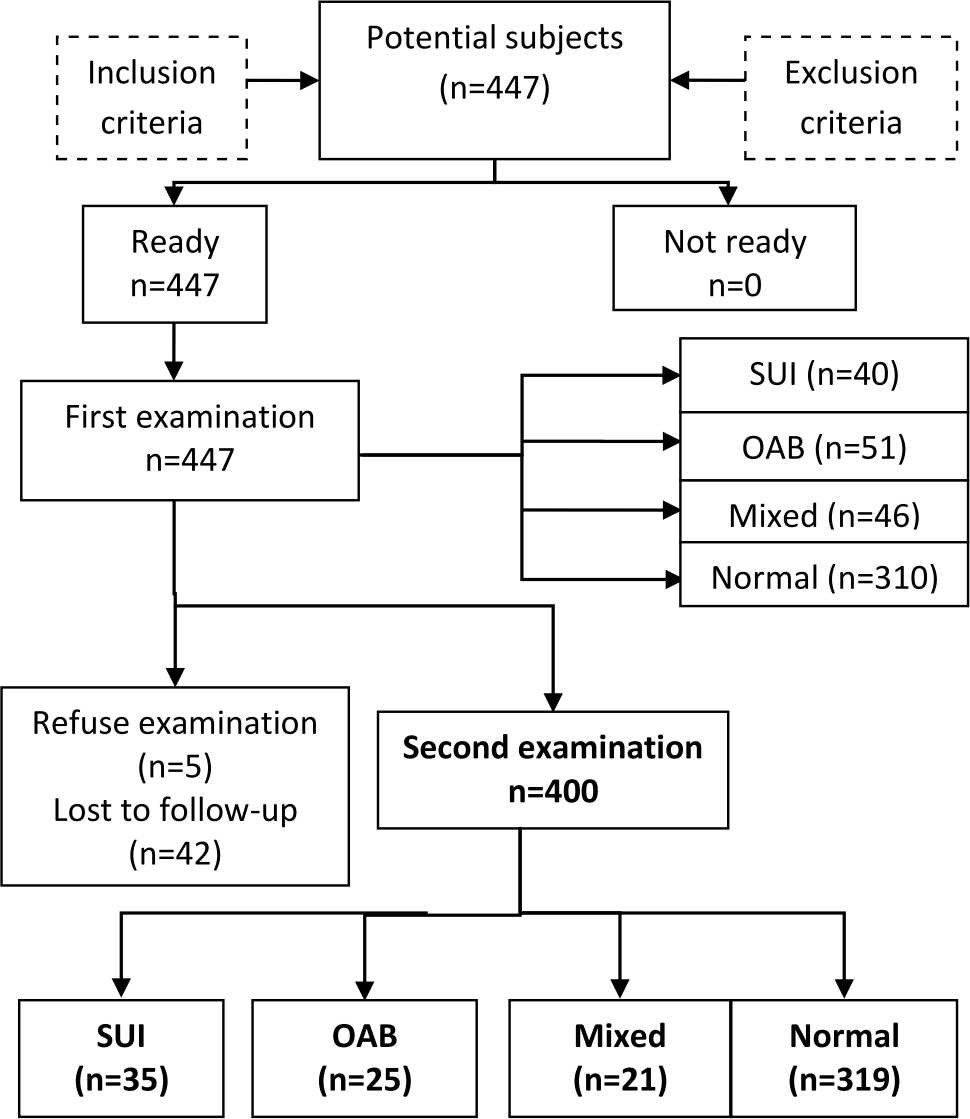
Figure 1. Flow chart of the study. SUI: stress urinary incontinence; OAB: overactive bladder
Subjects characteristic
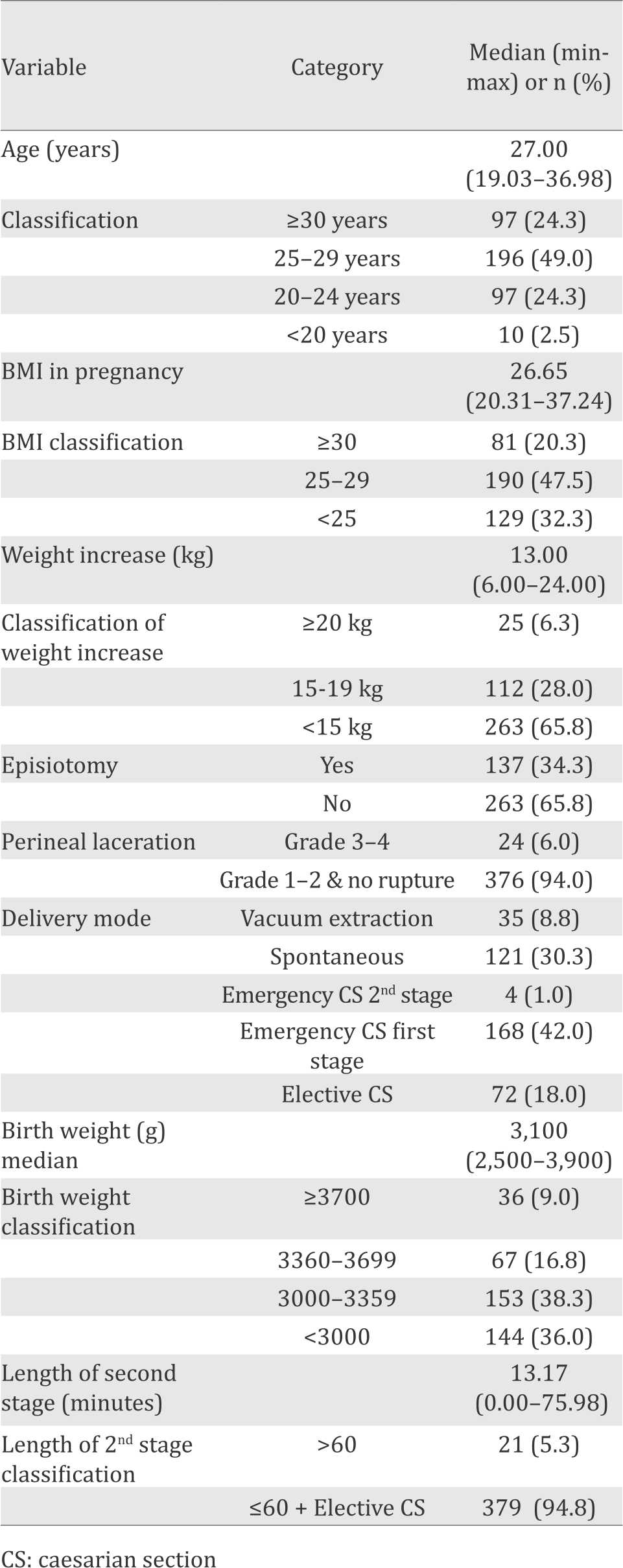
There were 400 subjects that had undergone second examination at three months postpartum (Table 1).
Table 1. Characteristic of the subjects
Bivariate analysis
From 354 primiparous women, no abnormalities were found in 319 subjects, whereas 35 subjects were diagnosed with persistent postpartum stress urinary incontinence which became the analytical subjects in this study. The relationship between independent variable (risk factors) and dependent variable (persistent SUI) was analyzed in table 2.
Table 2. Bivariate analysis correlation between risk factors and persistent postpartum SUI
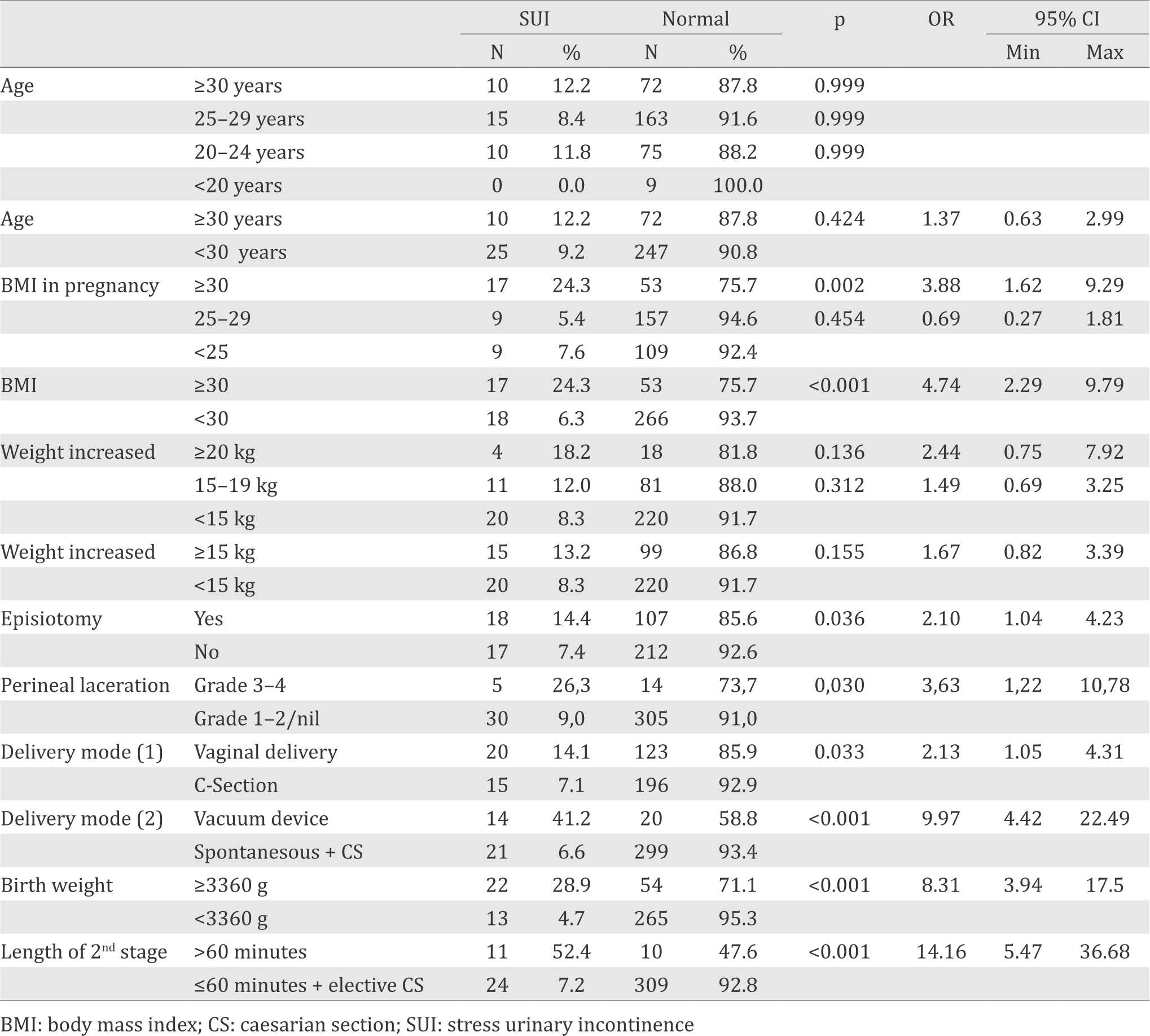
Chi-square variables with p<0.250 in the bivariate analysis was considered having relationship to the incidence of postpartum SUI and further qualified included into the multivariate analysis. Bivariate analysis showed that BMI classification ≥30, weight increased ≥15kg, episiotomy, perineal laceration stage 3-4, vacuum delivery, birth weight ≥3,360 g, and length of second stage ≥60 minutes had relationship with the persistent SUI at three months postpartum in primiparous women as table 2.
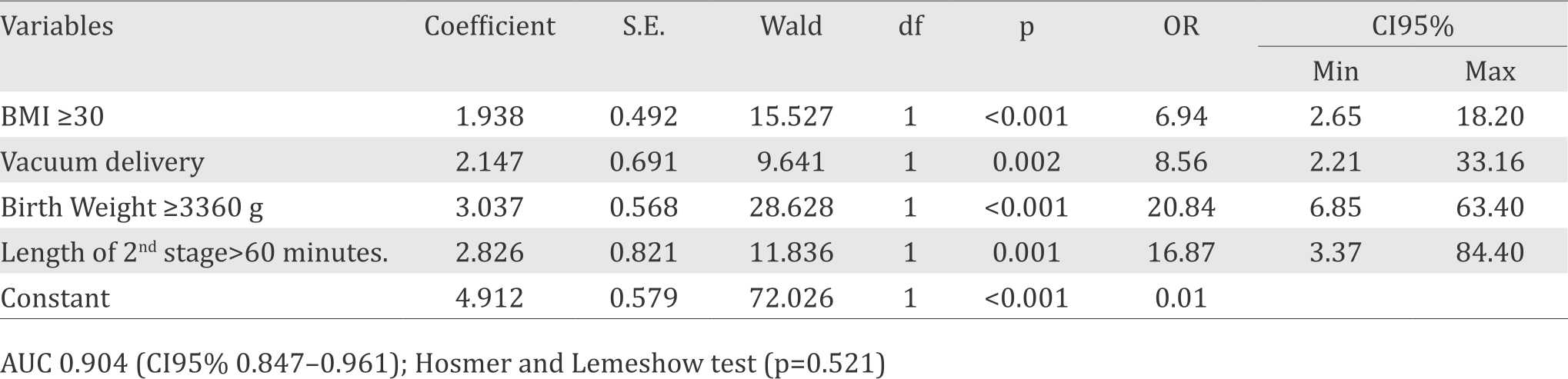
Multivariate analysis
All of the risk factors related to the persistent SUI at three months postpartum which had been selected with bivariate analysis were further included into the multivariate analysis using backward stepwise method. This process would stop when all variables left had p value less than 0.05. Therefore, the risk factors that significantly associated with persistent three months postpartum SUI were BMI >30 kg/m2, vacuum delivery, birth weight >3,360 g and length of second stage ≥60 minutes (Table 3). To rate the quality of multivariate analysis, calibration test was done using Hosmer & Lemeshow test (p=0.521) and discrimination test AUC value 90.4% (95% CI=0.847–0.961). Statistically, this analysis had a good quality and strong aspects of calibration (p>0.05 in Hosmer & Lemeshow test) and discrimination AUC >80% (95% CI).21
Table 3. Multivariate analysis of logistic regression (final model)
DISCUSSION
In this study, 81 subjects (20.3%) developed urinary incontinence at three months postpartum. This finding was higher than the result by Boyles et al12 in Oregon, USA (17.1%), but lower than the result of study in Scotland by Glazener et al22 (29%) and meta-analysis by Thom and Rortveit (28.7%).7
Out of 81 subjects who had urinary incontinence, 35 subjects (8.8%) had SUI, 25 subjects (6.3%) urge urinary incontinence/overactive bladder (UUI/OAB), and 21 subjects (5.3%) had mixed type. Compared to previous studies, the prevalence of persistent SUI at three months postpartum in primiparity in this study was similar to the study by Tincello et al (8.7%),23 higher than findings by Viktrup et al (6.1%),16 and lower than the result by Glazener et al22 (13.5%). This finding was also lower than the result of a meta-analysis by Thom and Rortveit7 with SUI prevalence average of 12.6%.7 Based on the distribution of urinary incontinence type, 43% of subjects had stress urinary incontinence, 31% had OAB, and 26% had mixed urinary incontinence (Figure 1). This finding was similar to the result found by Glazener et al22 and meta-analysis by Thom and Rortveit.7,22 The study by Glazener et al22 showed that 48% subjects had SUI, 22% had OAB, and 30% had mixed type, while Thom and Rortveit7 found that the frequency of SUI was 46%, about twice the prevalence of OAB.
This study also found an increased risk of SUI at three months postpartum in women with BMI >30 kg/m2 (OR=4.74, 95% CI=2.29–9.79). However, increase of maternal weight throughout gestation did not increase the risk of postpartum SUI (OR=1.67, 95% CI=0.82–3.39). Study by Boyle et al12 found that BMI >30 kg/m2 at delivery would increase the risk of SUI (OR=1.88, 95% CI=1.17–3.01),12 but no correlation between SUI and weight gain during gestation. Eftekhar et al found that BMI >30 increased the risk of SUI within four months postpartum (p=0.001; χ2=17.6).24
Among 143 subjects who had vaginal delivery and 211 subjects who undergone caesarean section, 20 subjects (14.15%), and 15 subjects (7.1%) respectively developed SUI. The risk of developing persistent SUI within three months postpartum was higher in primiparity with vaginal delivery than those who had caesarean section (OR=2.1, 95% CI=1.05–4.31). The risk was increased if the vaginal delivery was assisted by vacuum device (OR=9.1, 95% CI=3.9–21.6). This result agreed with the findings by Glazener et al22 that showed an increased risk of postpartum SUI in vaginal delivery (21%) compared to caesarean section (6%) with OR=3.97 (95% CI=2.69–5.81).22 Meta-analysis by Thom and Rortveit7 also found a higher incidence of SUI in vaginal delivery (average of 30.8%) compared to caesarean section (average of 14.8%).7
This study also showed that emergency cesarean section did not increase the risk of SUI compared to elective caesarean section (OR=0.84, 95% CI=0.28–2.57). Study by Boyles et al12 also found similar results that there was no significant difference between the incidence of urinary incontinence in the elective caesarean section (6.1%) and emergency caesarean section before labor (5.7%) or caesarean section during labor (6.4%).12 This finding supported the theory that the risk of postpartum urinary incontinence was relatively the same between caesarean section done before labor and during labor.12 Therefore, labor process did not reduce the protective effect of cesarean section to the risk of SUI. This finding was clinically important since most primigravid patients tried to give vaginal delivery before having a caesarean section, thus vaginal delivery that ended up with caesarean section did not increase the risk of SUI. Although the result of this study and Boyle’s study showed that the risk of SUI within three months postpartum was increased in subjects who undergone vaginal delivery, this finding was only consistent for short term outcome (three months).12 This was relevant to the recommendation issued by National Institutes of Health State of the Science conference: Caesarean Delivery on Maternal Request in 2006. It stated that within three months postpartum, the group of women who had planned cesarean section developed less urinary incontinence compared to the group of women who had vaginal delivery. However, two years afterwards, the incidence of urinary incontinence in both groups was the same.24
This study results also showed that birth weight more than 3,360 g was increasing the risk of SUI with OR=8.31 (95% CI=3.94–17.50) and much more when reaching >3,700 g with OR=9.99 (95% CI=4.09–24.37). Eftekhar et al25 showed that birth weight >3,000 g are increasing the risk of SUI at four months postpartum (p<0.001; χ2=22.5). Glazener et al22 obtained increasing risk of SUI with birth weight was >3,700 with OR=1.56 (95% CI=1.12–2.19). Boyles et al12 showed that birth weight had no influence to urinary incontinence in caesarean section subjects, but birth weight of 4,000 g or more in vaginal birth would increase the risk of urinary incontinence with OR=1.22 (95% CI=1.03–1.45).12
The increasing risk of SUI in subjects with the longer duration of the second stage of labor, by 60 minutes, was denoted in this study (52.4%), compared with less than 60 minutes in duration (7.2%) with OR=14.16 (95% CI=5.47–36.68). Boyle et al obtained increasing risk of urinary incontinence in subjects with duration of the second stage of labor >45 minutes (61.5%) compared with subjects with duration <45 minutes (51.5%) with p=0.001.12
The result of this study gave important information to patients, clinicians, and stakeholders related to options of giving delivery mode with its risk of SUI later. Clinicians’ awareness in antenatal care to motivate and give advice to pregnant women to maintain ideal body weight during pregnancy had a big role in preventing the negative impact of SUI in their quality of life in the future.
In conclusion, results from this study reveal that vaginal delivery is associated with a higher risk of stress urinary incontinence than caesarean delivery. Labor did not affect the protective effect of cesarean delivery. Modifiable risk factors for stress urinary incontinence, such as obtaining an ideal body weight, and preventing a traumatic and long process of vaginal delivery were identified and hold promise as potential preventive measures for postpartum stress urinary incontinence.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
Thank you to my family and all people who has contributed in organizing this study
REFERENCES
- Amaro JL, Macharelli CA, Yamamoto H, Kawano PR, Padovani CV, Agostinho AD. Prevalence and risk factors for urinary and fecal incontinence in Brazilian women. Int Braz J Urol. 2009;35(5):592–7.
- Schultz SE, Kopec JA. Impact of chronic conditions. Health Rep. 2003;14(4):41–53.
- Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900–7.
- Carpenter DA, Visovsky C. Stress urinary incontinence: a review of treatment options. AORN J. 2010;91(4):471–8. Medical Journal of Indonesia
- Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001;98(3):398–406.
- Holroyd-Leduc JM, Straus SE. Management of urinary incontinence in women: scientific review. JAMA. 2004;291(8):986–95.
- Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstet Gynecol Scand. 2010;89(12):1511–22.
- Bajuadji HS. Stres inkontinensia urin pascapersalinan [thesis]. Jakarta: Universitas Indonesia; 2004. p. 71.
- Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA) / International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
- Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
- Memon HU, Handa VL. Vaginal childbirth and pelvic floor disorders. Womens Health (Lond Engl). 2013;9(3):1–18.
- Boyles SH, Li H, Mori T, Osterweil P, Guise JM. Effect of mode of delivery on the incidence of urinary incontinence in primiparous women. Obstet Gynecol. 2009;113(1):134–41.
- Groutz A, Rimon E, Peled S, Gold R, Pauzner D, Lessing JB, et al. Cesarean section: does it really prevent the development of postpartum stress urinary incontinence? A prospective study of 363 women one year after their first delivery. Neurourol Urodyn. 2004;23(1):2–6.
- McKinnie V, Swift SE, Wang W, Woodman P, O’Boyle A, Kahn M, et al. The effect of pregnancy and mode of delivery on the prevalence of urinary and fecal incontinence. Am J Obstet Gynecol. 2005;193(2):512–7.
- MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000;107(12):1460–70.
- Viktrup L, Lose G, Rolff M, Barfoed K. The symptom of stress incontinence caused by pregnancy or delivery in primiparas. Obstet Gynecol. 1992;79(6):945–9.
- Viktrup L, Lose G. The risk of stress incontinence 5 years after first delivery. Am J Obstet Gynecol. 2001;185(1):82–7.
- Burgio KL, Zyczynski H, Locher JL, Richter HE, Redden DT, Wright KC. Urinary incontinence in the 12-month postpartum period. Obstet Gynecol. 2003;102(6):1291–8.
- Bradley CS, Rovner ES, Morgan MA, Berlin M, Novi JM, Shea JA, et al. A new questionnaire for urinary incontinence diagnosis in women: development and testing. Am J Obstet Gynecol. 2005;192(1):66–73.
- Rijal C. Prevalensi inkontinensia urin dan faktor-faktor risiko yang berhubungan pada wanita yang tinggal di panti werdha [thesis]. Jakarta: Universitas Indonesia; 2013. p. 55. Indonesian.
- Dahlan MS. Mendiagnosis dan menatalaksana 13 penyakit statistik disertai aplikasi program stata. Jakarta: Penerbit Salemba Medika; 2010. p. 285. Indonesian.
- Glazener CM, Herbison GP, MacArthur C, Lancashire R, McGee MA, Grant AM, et al. New postnatal urinary incontinence: obstetric and other risk factors in primiparae. BJOG. 2006;113(2):208–17.
- Tincello DG, Adams EJ, Richmond DH. Antenatal screening for postpartum urinary incontinence in http://mji.ui.ac.id nulliparous women: a pilot study. Eur J Obstet Gynecol Reprod Biol. 2002;101(1):70–3.
- National Instutes of Health. NIH state-of-the-science conference: Cesarean delivery on maternal request. William H. Natcher Conference Center. 2006.
- Eftekhar T, Hajibaratali B, Ramezanzadeh F, Shariat M. Postpartum evaluation of stress urinaryincontinence among primiparas. Int J Gyneacol Obstet. 2006; 94(2):114–8.
Copyright @ 2016 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id