
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
Clinical characteristics of acute respiratory distress syndrome survived patients at a tertiary hospital in Jakarta
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v26i1.1470 Med J Indones. 2016;26:35–9
Received: June 06, 2016
Accepted: November 13, 2016
Author affiliation:
1 Department of Internal Medicine, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
2 Department of Internal Medicine, Siloam General Hospital, Manado, Indonesia
Corresponding author:
Zulkfli Amin
E-mail: zulkifliamin52@gmail.com
Background
While a good deal of research on characteristic the different characteristics between surviving and dying patient with ARDS has been conducted globally, such research is scarce in developing countries. This study aimed to obtain clinical profile of ARDS survivors during hospitalization.
Methods
This was a prospective, observational study conducted at a tertiary hospital in Jakarta from October 2015 to April 2016. Primary data was collected from ARDS patients based on Berlin Definition admitted to emergency room, ICU, HCU, ICCU, and all other wards. The patients were followed until they discharged. We only included survivors on the analysis. Descriptive analysis was done using SPSS 21.0.
Results
A total of 43 patients were survived during study period. The majority were below 65 years of age (69.8%) and were male (53.5%). ARDS was mainly mild in severity (62.8%) and early onset (55.8%). Sepsis was the most common causes of ARDS (97.7%). Most of the patients had comorbidities (74.4%). Majority of the patients had APACHE II score <20 (77.3%) with mean 15.6±4.8. The mean of albumin was 2.9±0.6 and the median of procalcitonin was 3 (0.1-252.3).
Conclusion
The clinical profile of ARDS survivors in our study were mostly similar with other studies conducted in developed and other developing countries.
Keywords
ARDS, clinical profile, survivors
Acute respiratory distress syndrome (ARDS) is an acute inflammatory lung injury, characterized by increased pulmonary capillary endothelial cells and alveolar epithelial cells permeability leading to respiratory failure in the absence of cardiac failure.1 ARDS may arise from sepsis and non-sepsis causes.2 Despite recent advances in treatments, overall mortality rate remains high ranging from 25 to 49%.3 Death within 72 hours of admission is mainly caused by the condition that caused ARDS. Meanwhile after 72 hours of admission, nosocomial pneumonia and sepsis were the most common cause of death.4,5
While a good deal of research on different characteristics between surviving patients and dying one has been conducted globally, such research is scarce in developing countries. The aim of this study was to obtain clinical profile of patients with ARDS who survived during hospitalization at a tertiary hospital in Jakarta.
METHODS
This was a prospective, observational study conducted in emergency room, intensive care unit (ICU), high care unit (HCU), intensive coronary care unit (ICCU) and all other wards at a tertiary hospital in Jakarta from October 2015 to April 2016. All patients admitted with ARDS were followed until they discharged. The inclusion criteria were as follows: (1) diagnosed as ARDS based upon Berlin definition 2011, (2) age 18 years and older. The exclusion criteria was death during hospitalization. The protocol of this study has been approved by Medical Ethics Committee od Universitas Indonesia (No. 998/UN2.F1/ETIK/2015).
Variables and measurement
The demographic characteristics included age and gender. The clinical characteristics included etiology of ARDS, ARDS severity, onset of ARDS, days from admission to ARDS onset, duration of mechanical ventilation prior to ARDS, comorbidity, Acute Physiology and Chronic Health Evaluation (APACHE) II score, length of stay, and mean arterial pressure. The laboratory result included hemoglobin (Hb), white blood cells (WBC), platelet count, aspartate transaminase (AST), alanine transaminase (ALT), albumin, random blood glucose, blood urea nitrogen (BUN), serum creatinine, ratio of arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FiO2 ratio), pH, partial pressure of carbon dioxide in arterial blood (PaCO2), partial pressure of oxygen in arterial blood (PaO2), Na, K, Cl, and procalcitonin.
ARDS was defined as a precipitant of lung injury or development of new or worsening respiratory symptoms within one week, in which the presence of bilateral infiltrates on a chest radiograph and pulmonary edema was not caused by cardiac problem. The severity of ARDS was categorized based on the degree of hypoxemia: mild (PaO2/ FiO2 201-300 mmHg), moderate (PaO2/FiO2 101-200 mmHg), and severe (PaO2/FiO2 ≤100 mmHg).6
The etiology of ARDS was categorized into sepsis and non-sepsis causes. Sepsis was diagnosed if there were at least two of the following symptoms: body temperature >38° C or <36°C, heart rate >90x/minute, respiratory rate >24x/ minute or PaCO2<32 mmHg, leucocyte count >12,000 cells/mm3 or <4,000 cells/mm3 or >10% immature form, and definite source of infection.2 Non-sepsis condition may arise from large burn, repeated transfusion, emboli, acute pancreatitis, severe trauma, drowning, inhalation of drug, lung contusion prior to ARDS.2
Early onset ARDS was defined as ARDS developing during the first 48 hours after hospital admission. Comorbidity was defined by documented clinical diagnosis at the end of hospitalization. Its category included diabetes mellitus, chronic kidney disease, systematous lupus erythematous (SLE), liver cirrhosis, cerebrovascular disease (CVD), and acquired immune deficiency syndrome (AIDS). The APACHE II score is a measure of severity of disease and used to assess risk of inhospital mortality.7 It was calculated on the first 24 hour of ARDS and categorized into <20 and ≥20.
Statistical analysis
Data was analyzed using SPSS (SPSS Inc., Chicago, IL, USA) program version 21.0. For qualitative variables, a descriptive analysis was done and presented as frequencies (percentage). Frequency of quantitative variable was calculated and represented using mean±SD or median (interquartile range/IQR) if the data was not normally distributed.
RESULTS
Demographic, clinical characteristics, and laboratory result of the patients are listed in Table 1, 2, and 3 respectively. There were 43 patients who survived of ARDS during the study. The majority were below 65 years old (69.8%) and were male (53.5%).
Table 1. Demographic characteristics
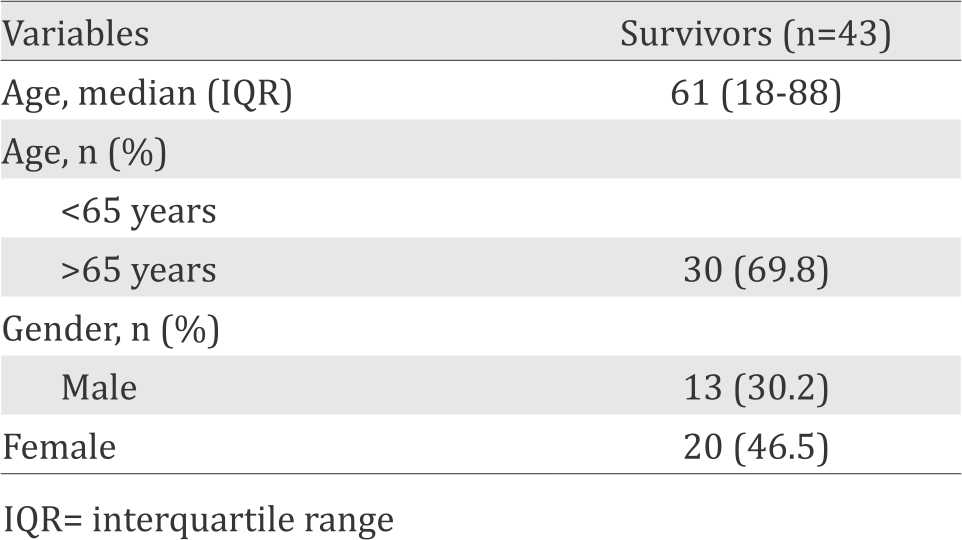
Table 2. Clinical characteristics
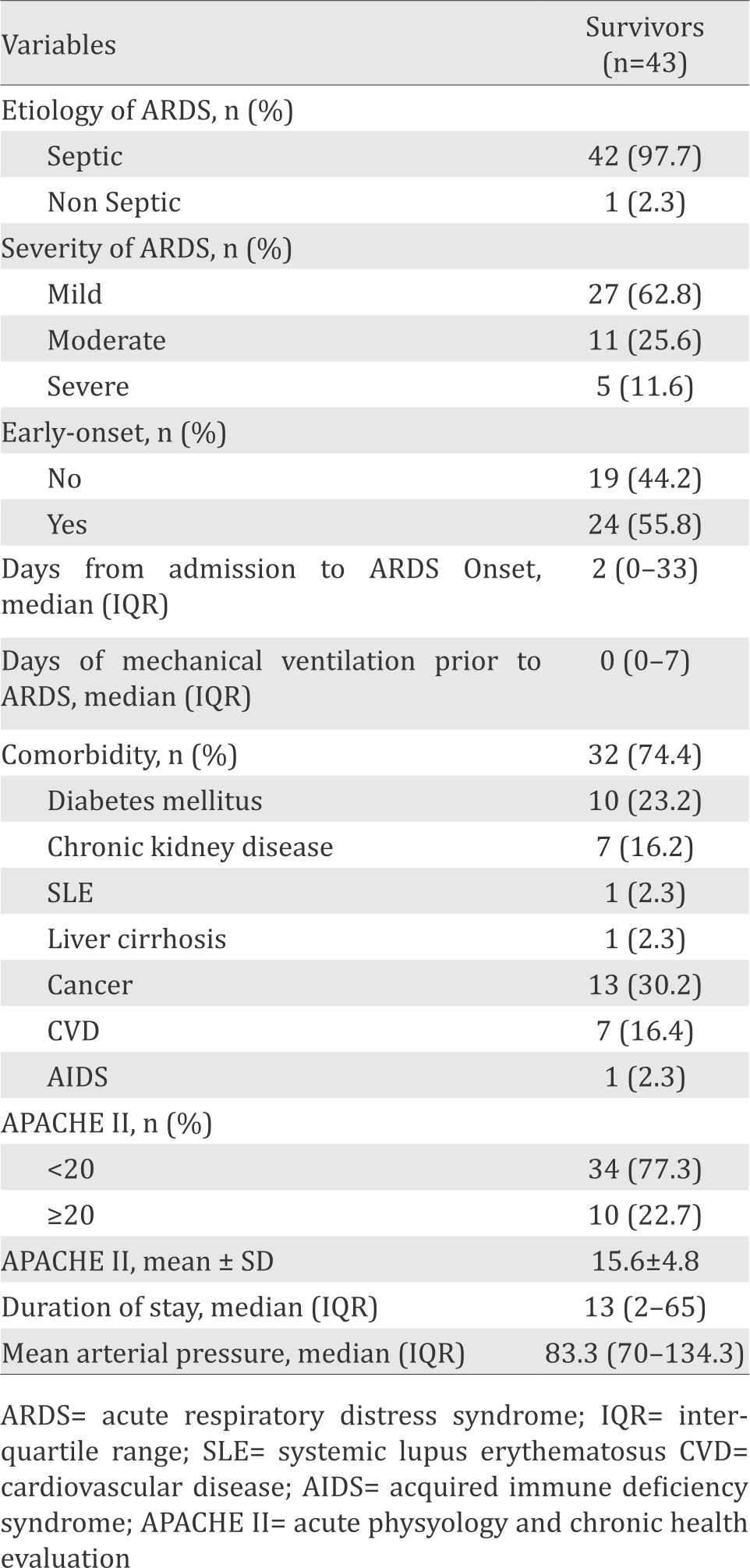
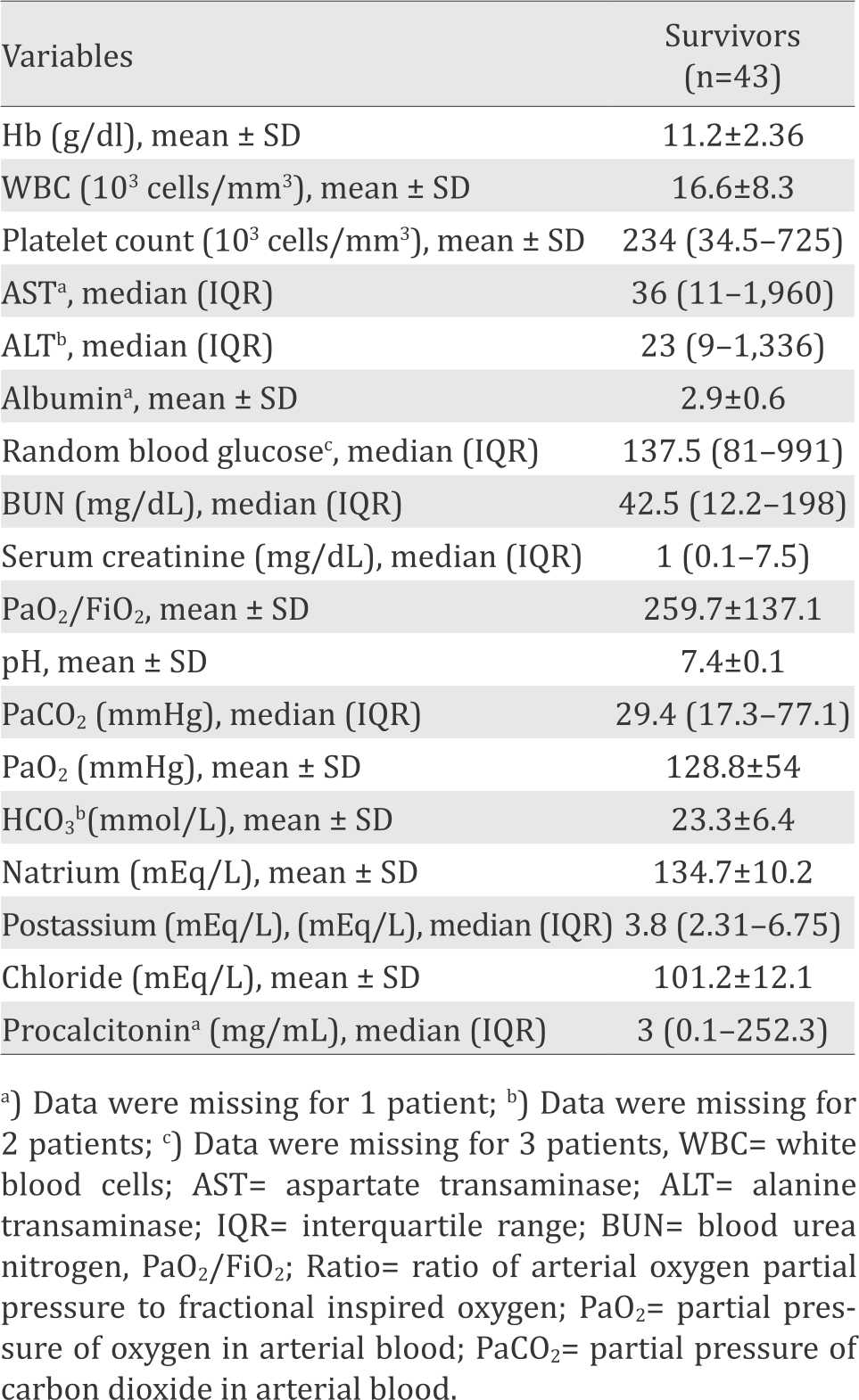
Table 3. Laboratory result
The clinical characteristics that have been identified among the majority are as follows: they developed mild ARDS (62.8%), the cause of ARDS was sepsis (97.7%), their onset was early (55.8%), their APACHE II score was less than 20 (77.3%), they had comorbidities (74.4%), and the length of their stay was 16 (from 2 to 65) days. Comorbidities included diabetes mellitus (23.2%), chronic kidney disease (16.2%), SLE (2.3%), liver cirrhosis (2.3%), cancer (30.2%), cerebrovascular disease (16.2%), and AIDS (2.3%).
DISCUSSION
The present study attempts to obtain clinical profile of patients who survived from ARDS during hospitalization at a tertiary hospital in Jakarta.
In the present study, the majority of ARDS survivors were below 65 years of age with the median of 61 (18-88). This result is similar with the study conducted by Sharif et al8 which found that 90% of the survivors were below 65 years old. It has also been shown by the study from Zilberberg et al9 that older age (>65 years) was independently associated with higher mortality rate among ARDS patients.
Female gender was associated with lower mortality rate in several studies. They attributed it to different genetic susceptibility in response to ARDS and the therapy or hormonal difference.10 However, the predilection of gender was vary among studies. In our study, the majority of survivors were male (53.5%). This result is in accordance with the results by Venet et al11, Bhadade et al12 and Tseng et al13 which stated that most of ARDS survivors were male, with percentage 76.5%, 75.5%, and 57.5%, respectively.
Majority of survived patients in our study developed ARDS due to sepsis. This is due to the fact that although sepsis-related ARDS has higher mortality than non-sepsis related, sepsis is the major cause of ARDS.2
According to Berlin definition, the severity categories of ARDS (mild, moderate, severe) are associated with increased mortality (27%, 32%, and 45%, respectively).6 The majority of ARDS survivors in our study were developed mild ARDS.
The majority of patients developed early-onset ARDS which was similar with the study by Liao et al.14 According to the study, late-onset ARDS contributed to increased mortality. In addition, the duration of mechanical ventilation before the onset of ARDS was also independent risk factors of mortality. In our study, the median of duration of mechanical ventilation prior to ARDS was similar with the result from Liao et al14 (0 (0–7) vs 0.5±0.7).
Almost all of the patients in this study had comorbidities. This finding was similar with other study by Sheu et al2 and Erickson et al15 which shown that 40% of survived ARDS patients had comorbidity. This study conducted in a tertiary care centre which accepts referral patients from other hospitals in Jakarta and other provinces. That’s why patients usually had complex conditions and more than one underlying diseases.
According to the study conducted by Saleh et al16 which compared mortality prediction of different scoring system, APACHE scoring system was recommended to be used rather than other systems because of its superior accuracy. In addition, the APACHE II scoring system also routinely used in our hospital. Higher APACHE II represented severity of diseases and significantly associated with mortality. In our study, 77.3% of patients who survived have APACHE II score <20. This result is consistent with the other study conducted by Sharif N et al8 (75%). The median of APACHE II score (15.6±4.8) was also similar with the results from Estenssoro et al4 (19±6.3) and Luecke et al17 (17.9±4.7).
For the laboratory result, the result we found in our study was quite similar with the study by Liao et al.14 In our study, the mean of WBC (103/mm3) was 16.6±8.3 compared to 15.3±8.7; platelet count (103/mm3) 234 (34.5–725) compared to 226.3±132.4; BUN (mg/dl) 42.5 (12.2–198) compared to 38.5±28.2; serum creatinine 1 (0.1– 7.5) compared to 2.4±2.8.
The median of procalcitonin level was similar with study by Tang et al18 (3 (0.1–455) vs 2.59 (0.95– 6.25)). High level of procalcitonin could be arised from the damage alveolar integrity. Similarity on albumin level was also found between our study and Tseng et al13 (2.9±0.6 vs 2.56±9.67).
Meanwhile, the mean of PaO2/FiO2 (259.7±137.1), pH (7.4±0.1) and the median of PaCO2 (29.4 (17.3–77.1) were different from the results found in the study by Estenssoro et al4 PaO2/FiO2 (149±61) pH (7.32±0.09) and PaCO2 (42.8±13). However, other laboratory results were not included in other study.
There were several limitations in our study. The number of patients included was small due to the short duration of study. In addition, although we used the Berlin Definition in our study, we did not include complete ventilatory parameter due to the lack of data. We also did not include complete biomarker variables in our study.
In conclusion, the majority of patients who survived of ARDS during hospitalization in our hospital are as follows: below 65 years old, male, mild ARDS, caused by, early onset, diabetic comorbidities, APACHE score was <20, mean of albumin was 2.9, and median of procalcitonin was 3. The clinical profile was similar with the other studies from developed and developing countries.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Koh Y. Update in acute respiratory distress syndrome. J Intensive Care. 2014;2(1):2.
- Sheu CC, Gong MN, Zhai R, Chen F, Bajwa EK, Clardy PF, et al. Clinical characteristics and outcomes of sepsis-related vs non-sepsis-related ARDS. Chest. 2010;138(3):559–67.
- Pierakos C, Vincent JL. The changing pattern of acute respiratory distress syndrome over time: a comparison of two periods. Eur Respir J. 2012;40(3):589–95.
- Estenssoro E, Dubin A, Laffaire E, Canales H, Sáenz G, Moseinco M, et al. Incidence, clinical course, and outcome in 217 patients with acute respiratory distress syndrome. Crit Care Med. 2002;30(11):2450–6.
- Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD, Caldwell ES, Steinberg KP. Causes and timing of death in patients with ARDS. Chest. 2005;128(2):525–32.
- Ranieri V, Rubenfeld G, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–33.
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
- Sharif N, Irfan M, Husain J, Khan J. Factors associated within 28 days in-hospital mortality of patients with acute respiratory distress syndrome. Biomed Res Int. 2013;2013(564547):5.
- Zilberberg MD, Epstein SK. Acute lung injury in the medical ICU comorbid conditions, age, etiology, and hospital outcome. Am J Respir Crit Care Med. 1998;157(4Pt1):1159–64.
- Moss M, Mannino D. Race and gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979–1996). Crit Care Med. 2002;30(8):1679–85.
- Venet C, Guyomarc’h S, Pingat J, Michard C, Laporte S, Bertrand M, et al. Prognostic factors in acute respiratory distress syndrome: a retrospective multivariate analysis including prone positioning in management strategy. Intensive Care Med. 2003;29(9):1435–41.
- Bhadade R, de Souza RA, Harde MJ, Khot A. Clinical characteristics and outcomes of patients with acute lung injury and ARDS. J Postgrad Med. 2011;57(4):268–90.
- Tseng CC, Fang WF, Leung SY, Chen HC, Chang YC, Wang CC, et al. Impact of serum biomarkers and clinical factors on intensive care unit mortality and 6-month outcome in relatively healthy patients with severe pneumonia and acute respiratory distress syndrome. Dis Markers. 2014;2014(804654):1–9.
- Liao KM, Chen CW, Hsiue TR, Lin WC. Timing of acute respiratory distress syndrome onset is related to patient outcome. J Formos Med Assoc. 2009;108(9):694–703.
- Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD. Recent trends in acute lung injury mortality: 1996- 2005. Crit Care Med. 2009;37(5):1574–9.
- Saleh A, Ahmed M, Sultan I, Abdel-lateif A. Comparison of the mortality prediction of different ICU scoring systems (APACHE II and III, SAPS II, and SOFA) in a single-center ICU subpopulation with acute respiratory distress syndrome. Egyptian J Chest Dis Tuberculosis. 2015;64(4):843–8.
- Luecke T, Muench E, Roth H, Friess U, Paul T, Kleinhuber K, et al. Predictors of mortality in ARDS patients referred to a tertiary care centre: a pilot study. Eur J Anaesth. 2006;23(5):403–10.
- Tang L, Zhao Y, Wang D, Deng W, Li C, Li Q, et al. Endocan levels in peripheral blood predict outcomes of acute respiratory distress syndrome. Hindawi. 2014;201(652180):180–8.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id