Case Report
Pediatric gunshot penetrating head injury: a case report with 2-year follow-up
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v26i4.1472 Med J Indones. 2017;26:302–6
Received: June 8, 2017
Accepted: September 24, 2017
Author affiliation:
Department of Neurosurgery, Universitas Sumatera Utara, H. Adam Malik General Hospital, Medan, Indonesia
Corresponding author:
Steven Tandean
E-mail: steven_tandean@yahoo.com
Gunshot is a rare subset of penetrating head injury, and generally the victim dies before arriving at the hospital. This paper reported a case of an intracranial gunshot injury in a 12 year-old boy that was shot by his friend, whose primary intention was to play around, using a revolver. A missile projectile penetrated from mid frontal and came out from right occipital. Vital signs were stable with GCS 8 from physical examination. A rational management strategy should permit a good outcome. The only complications that occured were hydrocephalus, yet it was managed by VP– shunt. Skull defect was closed using titanium mesh. A twoyear follow-up showed a good result. The patient was able to do daily activity and back to school again.
Keywords
gunshot penetrating head injury, pediatric
The management of gunshot penetrating head injury is challenging for neurosurgeon, especially in pediatrics due to scarcity of experience and literature. Using clinical corollary literature on adults to pediatrics should be carefully considered.1 Gunshot penetrating head injury is usually associated with crime and suicide attempts with mortality rate 70–90% die before hospitalization and 50% die in hospital during resuscitation. According to several literatures, pediatrics has better outcomes in overall mortality and greater tendency for neurological recovery than in adults.1,2
Management of penetrating brain injury focusing solely on head injury should be avoided. Instead, a thorough review by primary and secondary survey of advance trauma life support (ATLS) is highly recommended. Radiology should be performed after the patient is stable. Computer tomographyscan (CT-scan), Skull X-ray anteroposterior (AP) and lateral are the most common and useful tools to evaluate gunshot head injury. The addition of CT 3D, CT angiography, and digital subtraction angiography (DSA) provide a reasonable initial assessment when available. The gunshot wounds can be treated using medication and by surgery. The purpose of medication is to decrease intracranial pressure (ICP) by preventing brain edema (head elevation 30–45°, hyperventilation PaCO2= 30–35 mmHg, mannitol), antiepileptic drugs, antibiotics administration, stress ulcer prevention, and administration tetanus toxoid. Moreover, surgery attempts to prevent not only a secondary injury caused by increasing ICP, but also infection and ischemic. Usual surgery procedures include brain stem decompression, hemostatis, and evacuation of mass lesion like hematoma, bone fragment, missile residual, and the repair of wounds.3,4
Case Report
After getting permission from the patient’s parent, we reported a case of 12-year-old boy who was shot at the head by his friend, whose primary intention was to play around, using his father revolver. The patient arrived at Haji Adam Malik Hospital 10 hours after the incident with chief complaint decrease of consciousness without any history of vomiting and seizure. According to physical examination, vital signs were stable with glasgow coma scale ( GCS ) E2M4V2, pupils are bilaterally equal and reactive, and no lateralization was documented. Based on head inspection, missile was found entering from mid frontal and coming out from right occipital. No other extra-cranial injury was found.
Laboratory blood investigations showed leukocytosis 30,000/mm3, increasing international normalized ratio (INR )1.34, D-dimer 1,600 ng/mL, and hyponatremia 132 mEq/L. Head CT scan showed fracture on the frontal and right occipital,intracerebral hematoma along with the missile track from frontal through right occipital, extensive perifocal edema, basal cistern compression, and midline shift more than 5 mm.
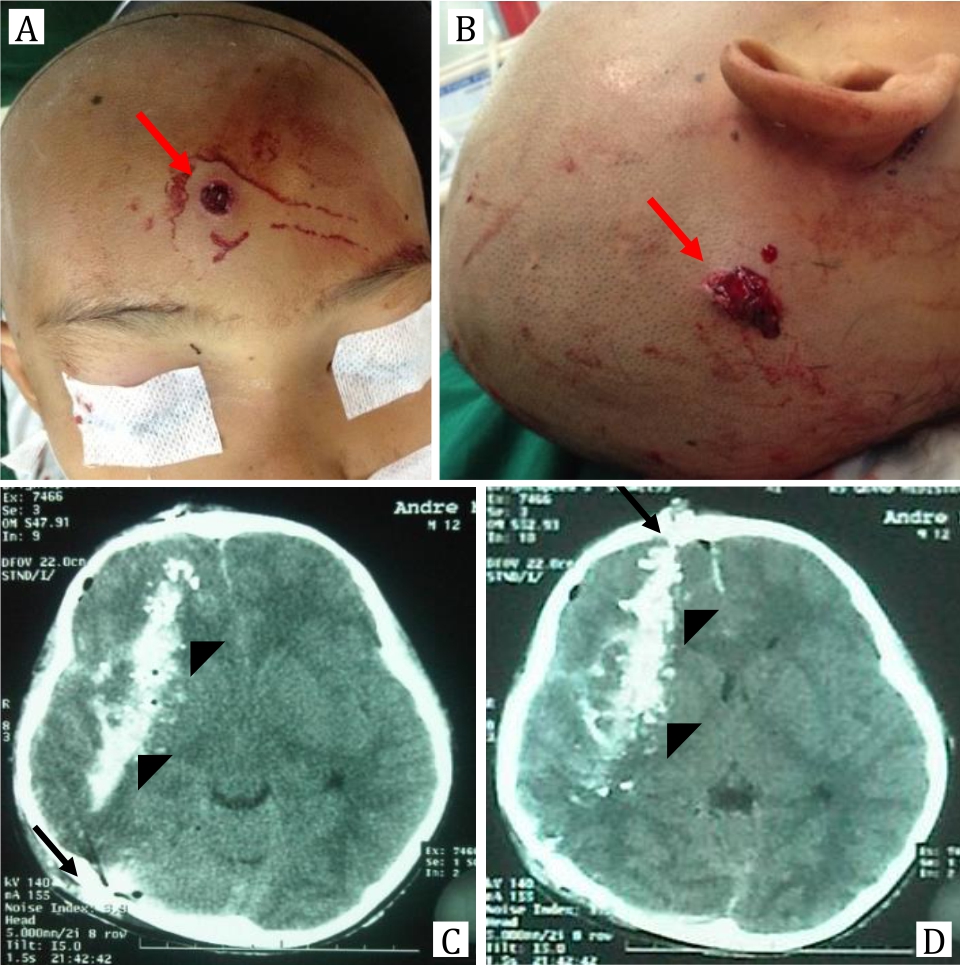
Figure 1. A,B) Missile enters from mid frontal and comes out from right occipital (red arrow); C,D) Head CT scan shows fracture on the frontal and right occipital, intracerebral hematoma (black arrow) along the missile track from frontal through right occipital (arrowhead). Sulcus and gyrus are hard to visualize. Extensive perifocal edema and midline shift are more than 5 mm
Craniectomy and intracerebral hematoma evacuation with source bleeding control wereperformed to the patient. A right pterional incision was done for frontal approach,meanwhile a horse shoe incision was conducted for exit wound approach. Dura was found torn with brain prolapse, source bleeding from cortical artery at the entry wound, and sigmoid sinus at the exit wound. Operation field was then washed with normal saline and hydrogen peroxide several times. Hematoma evacuation and bleeding control with bipolar and surgicel® were also conducted. As missile residual was not found, we continued with duraplasty using fascia. The wound was washed again with saline and hydrogen Peroxide. Finally, the bone was removed, and the skin was closed.
The patient was administered in pediatric intensive care unit (PICU) for 7 days and used the ventilator for 5 days. During the treatment at PICU, the patient was given antibiotic (Ceftriaxone 1 gr/12 hours/ iv and metronidazole 500 mg/8 hours/iv), seizure prophylactic, and mannitol. A CT-scan control on the second day after operation showed absorption of hematoma with perifocal edema, midline shift less than 5 mm, and uncompressed basal cistern. Seizure prophylactic was administered for 7 days and was stopped without any episodes of seizure. Patient was discharged after 15-day care at hospital with GCS 15 and left-sided hemiparesis with muscle strength was 4. Patient was followed up regularly at neurosurgical clinic and had regular physiotherapy.
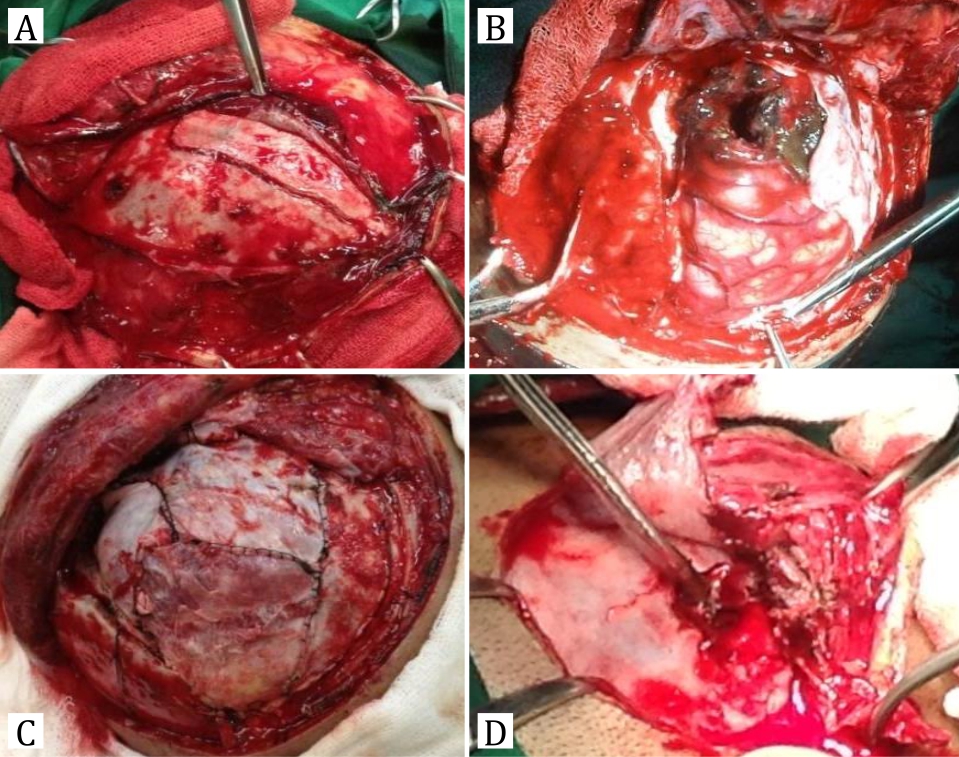
Figure 2. During the operation, A) Missile entered from frontal and caused linear fracture, thus debridement was conducted; B) After opening the dura, brain was prolapsed with subarachnoid hemorrhage and bulging; C) After hematoma evacuation, duraplasty with fascia was performed; D) Exit missile caused skull fracture and brain prolapse
Two months after the discharge, defect was bulging and tense without any episode of vomit and seizure. After regular physiotherapy, left-sided hemiparesis was recovered, and muscle strength was back to 5. Head CT scan was performed with a result of skull defect on the right front temporal and right occipital, cerebromalacia along the missile track and filled with cerebrospinal fluid, dilatation of right ventricle lateral, open basal cistern, and no midline shift. Ventriculoperitoneal (VP) shunt was placed on the left keen. Bulging was reduced after VP shunt, and defect became sunken. Then cranioplasty was performed using titanium mesh to close the skull defect. Patient was discharged in a good condition after 5-day treatment. Patient was still followed up regularly until two years after his first operation at neurosurgical clinic with a good result of neurologic function. Patient can do daily activity independently and was back to school.
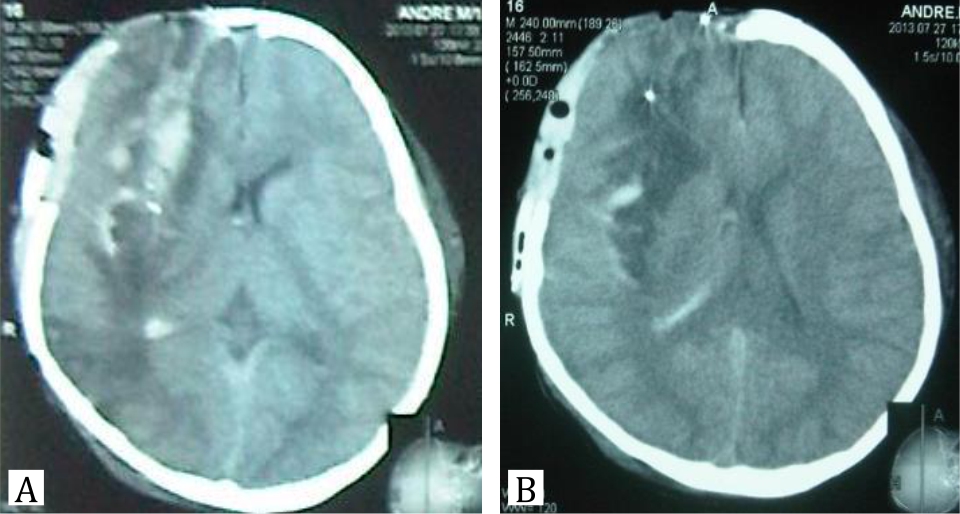
Figure 3. Head CT-scan control after 2-day operation shows absorption of hematoma with perifocal edema and midline shift less than 5 mm
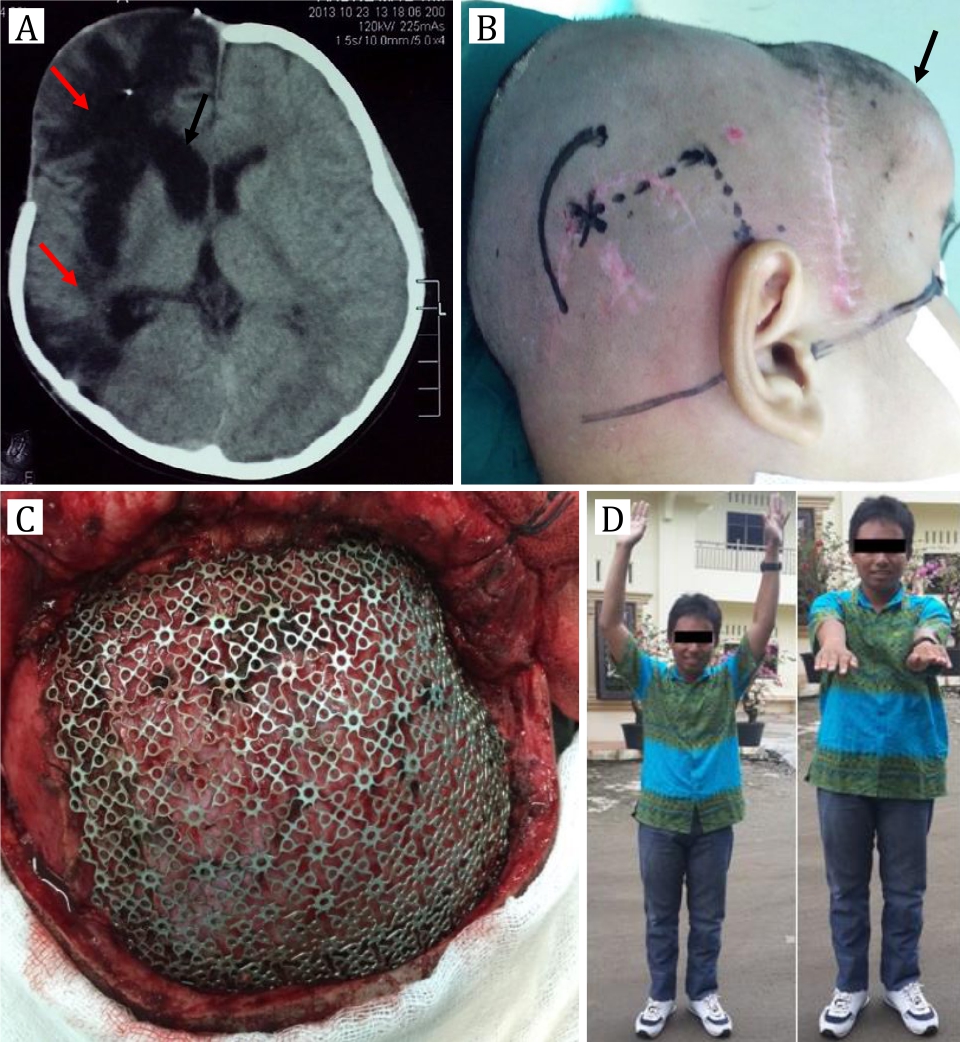
Figure 4. A) Two-month head CT scan after first operation, cerebromalasia along missile track fills with CSF (red arrow) and dilatation of right ventricle lateral (black arrow); B) Design incision and puncture point for VP shunt also shows bulging on the right frontal (black arrow); C). Cranioplasty with titanium mesh after VP shunt; D) Clinical presentation after 2-year follow-up shows a good outcome without any neurologic deficit
DISCUSSION
A gunshot wound to the head is a rare case in emergency rooms, especially in pediatrics. Gunshot penetrating head injury has a high mortality rate around 90% in adults and lower in pediatrics, around 65%. The highest mortality rate is between 70–90% before hospitalization and 50% of the survivals die during resuscitation in emergency rooms. Therefore, the management of gunshot penetrating head injury is very challenging for neurosurgeon, especially in pediatrics due to the scarcity of experience and literature. We could not find any reports of pediatric gunshot penetrating head injury in Indonesia. The use of clinical corollary literature and experiences on adults to pediatrics should be carefully considered.1,5
As a general for traumatic brain injury, pediatrics has a better propensity for neurological recovery than adult population. This caused difficulties in deciding appropriate management and predicting the prognostic. The only tool to guide management decisions and to provide prognostic information for gunshot to the head in pediatrics is St. Louis scale. Positive predictive value of ±90% for survival with St. Louis score ≤4, and negative predictive value of 78%–96.7% for death with St. Louis score ≥5. In our case, patient had score 3 with 2 points from 3 lobes involvement and 1 point from midline shift. Our limitation is that we could not perform ICP monitoring due to the lack of facility. We assumed that ICP was controlled post-operatively from good responses in vital sign and neurologic examination during care at pediatric intensive care unit. In literature, ICP monitoring was also routinely performed postoperatively than pre-operatively.1,6
Decompressive craniectomy around the missile entrance site has been a favored procedure in previous military conflicts. The present recommendation is to perform craniotomy and debridement of the skull with replacement of the bone to avoid cranioplasty in the future if the brain is not severe swelling. Decompressive craniectomy where the bone flap stored in a tissue bank or abdominal wall for future reimplantation was not recommended because of the increased risk for contamination and infection at the implanted site. In this case, decompressive craniectomy was performed because severe brain edema and bone flap were removed. Operation field washed using normal saline and hydrogen peroxide to reduce risk of infection. Then cranioplasty using titanium mesh was conducted to close the skull defect in the next operation.7,8
Decompressive craniectomy will make physiological change in intracranial pressure, cerebrospinal fluid circulation, and cerebral blood flow that caused many complications. A common complication after traumatic brain injury is hydrocephalus with reported incidence between 0–88%. Hydrocephalus will usually occur 1-month post-surgery. Pathophysiology hydrocephalus was caused by CSF malabsorption or obstruction of cerebrospinal fluid (CSF) flow and diminished CSF pulse wave caused by transmission of pulse out through the skull defect. Management for this complication is using VP shunt procedure. In this case, hydrocephalus occured on the second month after surgery. The area of cerebomalasia filled with CSF caused by connection to the right lateral ventricle. Increasing of CSF volume caused herniation and bulging through skull defect. This complication could be managed well by VP shunt procedure with diminished of the bulging after the procedure.9,10
One of the significant factors in the recovery from traumatic brain injury (TBI) is age. Older adults showed less favorable outcomes than younger adults. De la Plata et al11 analyzed the effects of TBI to the brain function using disability rating scale (DRS). The research showed that the 16–26 year old age group has the greatest improvement in disability and lower decline than older patients. It was caused by the increased plasticity of the brain in younger people. Subsequent research showed opposite pattern, young children with immature brain also showed less capable of recovering from damage. Anderson et al12 learned about the effects of TBI in developing brain by analyzing cognitive outcomes. The research showed that older children (8–12 years) had better cognitive recovery patterns than the younger children (3–7 years).11–13
Conclusion, pediatric gunshot penetrating head injury is scarce and challenging case. This patient has good outcome consistent with St. Louis scale for pediatric gunshot head injury. Positive predictive value of ±90% for survival with St. Louis score ≤4 and our patient had St Louis score 3.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- DeCuypere M, Muhlbauer MS, Boop FA, Klimo P. Pediatric intracranial gunshot wounds: The Memphis experience. J Neurosurg Pediatr. 2016;17:595–601.
- Lichte P, Oberbeck R, Binnebosel M, Wildenauer R, Pape H, Kobbe P. A civilian perspective on ballistic trauma and gunshot injuries. Scandinavian journal of trauma, resuscitation and emergency medicine. 2010;18:35–43.
- Van Wyck DW, Grant GA, Laskowitz DT. Penetrating traumatic brain injury: A review of current evaluation and management concepts. J Neurol Neurophysiol. 2015;6(6):336–43.
- Alexiou GA, Sfakianos G, Prodromou N. Pediatric head trauma. J Emerg Trauma Shock. 2011;4(3):403–8.
- Doan N, Nguyen HS, Patel M, Shabani S, Janich K, Montoure A. Management of gunshot wound to the head in pediatric population: Mini-Review. Ann Pediatr Child Health. 2016;4(3):1108–9.
- Bandt SK, Greenberg JK, Yarbrough CK, Schechtman KB, Limbrick DD, Leonard JR. Management of pediatric intracranial gunshot wounds: predictors of favorable clinical outcome and a new proposed treatment paradigm. J Neurosurg Pediatrics. 2012;10:511–7.
- Aarabi B, Armonda R, Bell RS, Stephens FL. Traumatic and penetrating head injuries. In: Winn HR, Bullock MR, Hovda DA, eds. Youmans neurological surgery. 6th eds. Philadelphia: Elsevier Saunders. 2011. p. 3453–64.
- Irfan FB, Hassan RU, Kumar R, Bhutta ZA, Bari E. Craniocerebral gunshot injuries in preschoolers. Childs Nerv Syst. 2010;26(1):61–6.
- Ding J, Guo Y, Tian H. The influence of decompressive craniectomy on the development of hydrocephalus: a review. Arq Neuropsiquiatr. 2014;72(9):715–20.
- Kurland DB, Khaladj-Ghom A, Stokum JA, Carusillo B, Karimy JK, Gerzanich V, et al. Complications associated with decompressive craniectomy: A systematic review. Neurocrit Care. 2015;23(2):292–304.
- De la Plata CM, Hart T, Hammond FM, Frol A, Hudak A, Harper CR, et al. Impact of age on long-term recovery from traumatic brain injury. Arch Phys Med Rehabil. 2008;89(5):896–903.
- Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116(6):1374–82.
- –Giza CC. Lasting effects of pediatric traumatic brain injury. Indian Journal of Neurotrauma. 2006;3(1):19–26.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id
