
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
The effects of intra-articular tranexamic acid given intraoperatively and intravenous tranexamic acid given preoperatively on post surgical bleeding and transfusion rate post total knee arthroplasty
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v25i4.1502 Med J Indones. 2016;25:234–9
Received: July 18, 2016
Accepted: November 13, 2016
Author affiliation:
Department of Orthopaedy and Traumatology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Corresponding author:
Aryo N. Triyudanto
E-mail: nugroho.triyudanto@yahoo.com
Background
Despite the advances in the design and fixation of implants in total knee replacement (TKR). the amount of postoperative bleeding is still an important issue that has not been resolved. This study aimed to measure the effectiveness of various tranexamic acid administration.
Methods
This was a randomized controlled trial study, held from August 2014 to February 2016 at Cipto Mangunkusumo Hospital, Jakarta. Twenty two patients having TKR were divided into three groups: the control group, the tranexamic acid intra-articular-intraoperative group, and the intravenous preoperative group. Intraoperative bleeding, haemoglobin (Hb) level on preoperative to five-day-post-surgery, total drain production, total blood tranfusion needed and the drain removal timing were recorded and compared. Numerical data were analyzed by using parametric and non-parametric test, depended on the normality of the data.
Results
The amount of blood transfusion needed in both the intra-articular group (200±SD 100 mL) and the intravenous group (238±SD 53 mL) were significantly different compared to those in the control group (1,016±SD 308.2 mL) (p=0.001). Meanwhile, there was no significant difference between the amount of blood transfusion needed in the intra-articular group and the intravenous group. Total drain production in the intra-articular group (328±SD 193 mL) and intravenous group (391±SD 185 mL) was significantly different compared to the control group (652±SD 150 mL) (p=0.003). No significant difference between the levels of both preoperative and postoperative haemoglobin, the amount of intraoperative bleeding, and the duration of drain usage.
Conclusion
Intravenous and intra-articular tranexamic acid effectively decreased transfusion volume and drain production in patients undergoing TKR.
Keywords
blood transfusion, intravenous, intra-articular, postoperative bleeding, total drain, total knee replacement, tranexamic acid
Osteoarthritis (OA) is a degenerative joint disease that leads to disability with prevalence increasing with ages.1 Despite mechanical factor, systemic process within the body and abnormalities in biomechanic load make joints more vulnerable. About 15% of the world population has OA, and the number is predicted to increase twice in 2020.2
Severe pain caused by progressive destruction of cartilago, intermitten inflamation, and other pathological process will limit the joint movement. Some of non-operative therapy such as non-steroidal anti inflamatory drugs, glucosamine, condhroitin sulphate become noninvasive solution to relieve pain and modified the pathological process with various rate of success.
Total knee arthroplasty (TKA) is thought to be the choice of treatment in OA with Kelgren Lawrence III and IV classification. TKA is aimed to restore the joint function nearly to normal. Yet, this prcedure has blood lost risk estimated from 800–1,700 cc; thus it is estimated that 50% of post TKA patients need blood transfusion. However, blood transfusion is a procedure with diverse risk and adverse effects. Hepatitis B has a transmission risk one in every 350,000 blood unit. Occasionally, blood transfusions lead to transfusion reactions. The reactions may vary from mild to severe. Transfusion related acute lung injury (TRALI) is a serious reaction that occurs one in every 5,000 transfusion. Several attempts have been done to avoid complications post-transfusion. Moreover, some studies showed that fibrin topical and intravenous injection of tranexamic acid (TXA) could decrease the bleeding in TKA.3
Many studies have been done to reveal the effects of tranexamic acid application in bleeding post-TKA. Nevertheless, specific research that compares the effects of intraoperative intraarticular tranexamic acid administration and pre-operative intravenous administration of rivaroxaban anti coagulant as well as modifies Robert Jones bandage has never been done in Indonesia. Therefore, we did a research to compare the effects of intravenous administration and intra-articular intraoperative injection of TXA on patients that underwent TKR in terms of total bleeding and transfusion rate post-TKA.
METHODS
This is a randomized control trial study that was held from August 2014 to February 2016. Twenty two patients (of total 28 patients available) were included according to the inclusion criteria: aged 50–80 years old, visiting outpatient clinic Cipto Mangunkusumo Hospital, Jakarta, and had severe OA end-stage of Grade III and Grade IV Kelgren Lawrence criteria that underwent total knee arthroplasty; while the exclusion criteria were those who consumed anticoagulant and anti-thrombocyte aggregation, had preoperative Hb ≤10.5 g/dl for man and woman, had intraoperative blood loss ≥500 cc, with mental illness, had uncontrolled diabetes mellitus (DM), rheumatoid arthritis, malignancy, and immunosuppression, had infected knee, had abnormal prothrombin time (PT) and activated partial thromboplastin test (APTT). The patients were later divided into three groups of treatment: the control group (Group I), the intraarticular intra operative TXA (Group II), and the intravenous perioperative TXA (Group III). Each sample was allocated randomly to each group of treatment. For intravenous group, tranexamic acid was adminstered by injecting 500 mg of tranexamic acid 10 minutes before tourniquet was extended, while for the intra-articular group, tranexamic acid was given moments after prosthesis was implanted.
For each of the treatment group, a drain was installed into the articular cavity, ensuring routine measurement of drain production. Drain was clamped for six hours after surgery. In addition, a modified-Robert-Jones wrapping and daily rivaroxaban administration were conducted for all of the patients. Bleeding postoperative was considered as the main outcome that was measured by total drain production, haemoglobin rate, and number of transfusion that was needed for each group.
Analysis of data utilized Statistical Package for Social Science (SPSS) v.15 (Chicago, Illinois). Demographic analysis, normality of data, and bi-variate analysis were done on all of the data. The protocol of this study has been approved by Medical Ethics Committee of Faculty of Medicine, Universitas Indonesia (No. 34/UN2.F1/ ETIK/2014) and patients were given verbal and written explanation and asked for consent for each of the groups.
RESULTS
A total of 22 patients were included in the trial. Mean age of the subjects were 65.1 years old (SD±6.82). Most of the samples were female (n=17, 77.3%), and the right knee was the most operated location (n=12, 54.5%). For each of the treatment group, bivariate analysis was done in order to assess homogenicity with a result showing that there was no difference for each of the demographic characteristics.
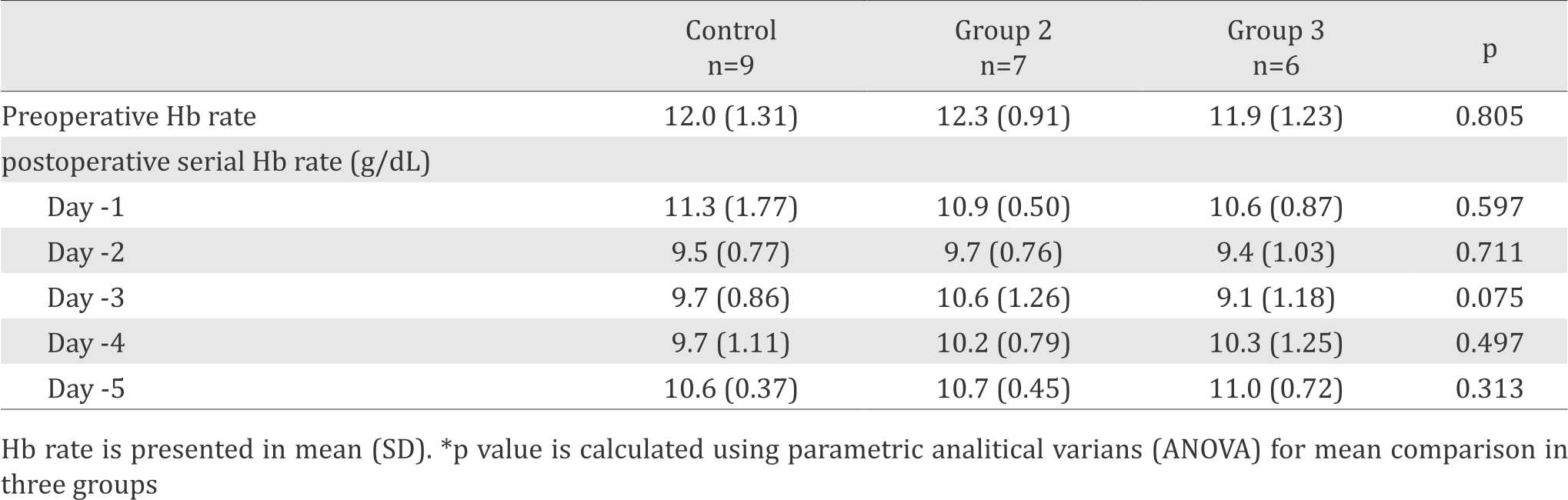
Mean preoperative haemoglobin was 12.1 g/dl (SD±1.13) with median blood loss of 200 ml (range 187–325ml) (Table 1). Haemoglobin (Hb) rate was measured serially before and five days after TKA operation was done. Generally, in all groups, Hb rates tended to decrease in the first and the second day after operation. Hb rate then gradually increased from day three to day five as can be seen in Table 2. There was no signifcant difference (p=0.305) between the groups in Hb rate changes from time to time.
Table 1. Demographic and clinical characteristics of patients with OA Grade III and IV who underwent Total Knee Arthroplasty
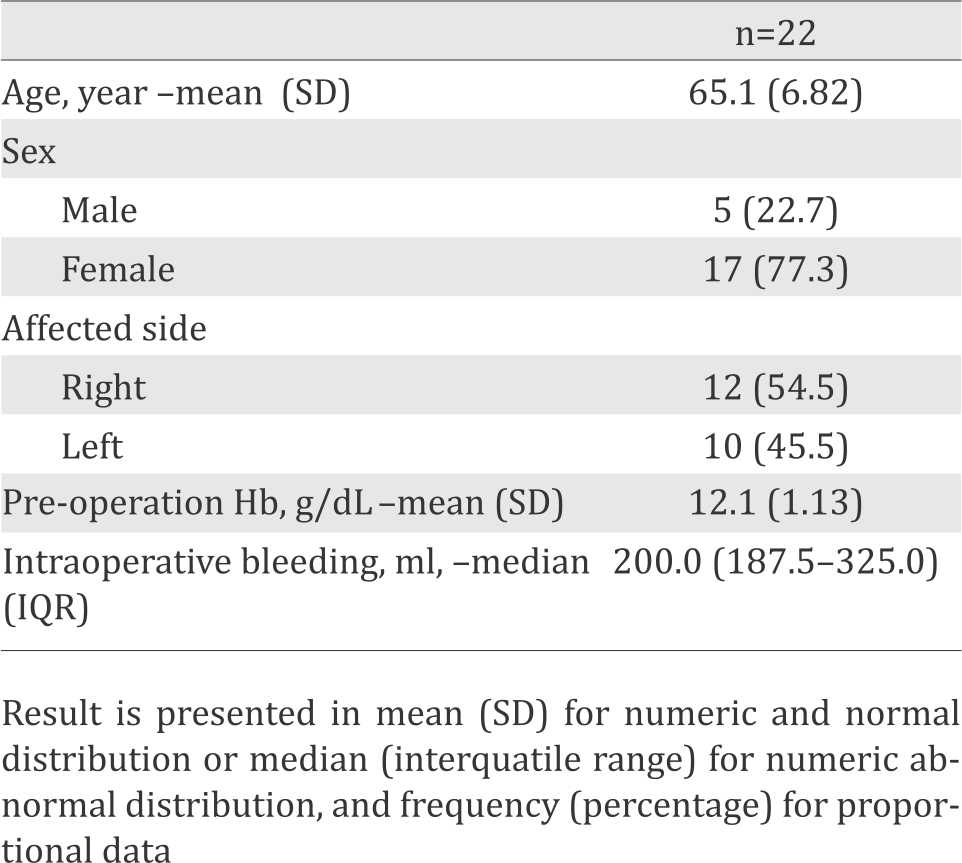
Table 2. Rate of serial haemoglobin Postoperative based on groups, tranexamic acid intra-articular, intravenous and control
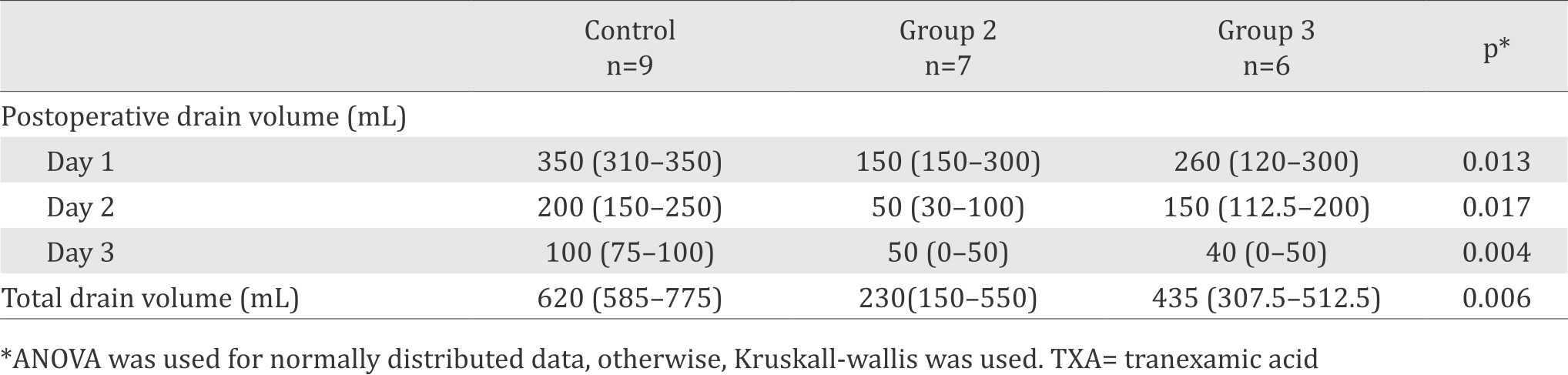
For drain production, the volume decreased for all groups every day during the three-day-follow up. There was a significant difference between each group from day to day and the total drain production. The highest drain volume was measured from the control group with the median of 620 (range: 585–775), while the least volume was measured from the second group with the median of 230 (range: 150–550) (Table 3).
Table 3. Outcome comparison for each group treated with intra-articular and intravenous TXA, and the control group
The median of blood transfusion volume in all patients was 200 (300–1,000) ml. There was a significant difference (p=0,001) between the groups, with control group held the highest transfusion number. However, there was no significant difference between the amount of blood transfusion needed in the second group and the amount needed in the third group (Table 4).
Table 4. Volume of blood transfusion based on interventions, intra-articular tranexamic acid, intravenous tranexamic acid and control
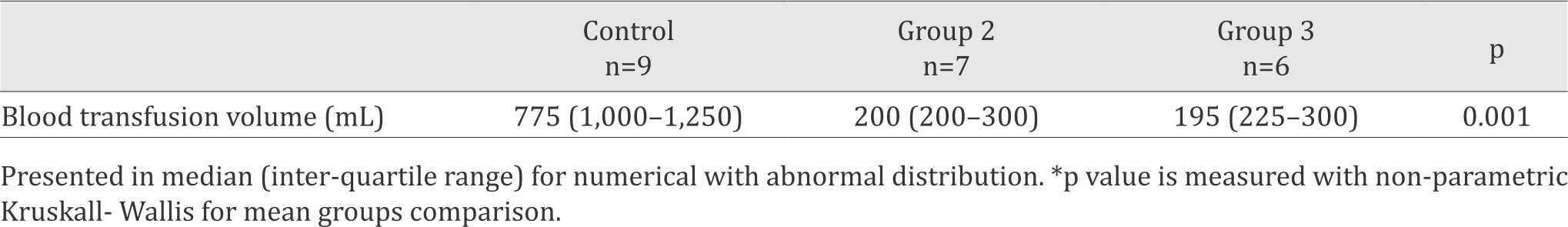
Further analysis was done in between the main treatment groups in order to know the difference of outcome of the groups. Drain volume was compared between the intra-articular and intravenous group, with no significance result (p>0.05) as the difference. Transfusion volume was also compared between the intravenous and intra-articular group, with no significance result (p>0.05) as the difference.
DISCUSSION
OA is a disease which incidentally increased as people get old. A study revealed that 8.9% of adult population are having OA. It implies that the probability of someone having OA is increased as ages.4 This result is concomitant with this study in which the median of subjects’ age was 65.1 years old. Yet, from all the groups above, there was no significant difference in ages.
Another characteristic is female with OA are more in number compared to male with OA. Sharon et al5 showed that anatomic, genetic, and hormonal were assumed to affect this difference in gender.5 Linear to Sharon et al,5 Heidari6 stated that female had a bigger OA risk than males. Yet, in this study the p=0.304 which implied that there was no significant difference between sexes in the groups.
Tranexamic acid is one of the most common anti-bleeding used in clinical practice. However, in orthopedic field, the usage of the tranexamic acid is still debatable due to its benefit and risk balance.7,8 Some research have suggested a beneficial usage for this medicine. Research that was done by Chen et al9 implied that intraarticular tranexamic acid could lessen blood loss in TKR without increasing the surgery duration significantly. This study was conducted to 50 patients who underwent TKR and were given 1,500 mg tranexamic acid. Intravenous tranexamic acid was proven to decrease drain after operation.9
We conducted three main outcome measurements for this study. Drain volume was measured serially from the first day to the third day after operation was done. Blood lost decreased gradually from day one to day four post-operation. There was a significant difference in day one drain volume (p=0.013), day two (p=0.017), and day three (p=0.004) post-operation. The control group had the biggest number of blood in drain volume. Drain volume was significantly different (p=0.006) between groups. Generally, bleeding volume is found in the control group. A study conducted by Zhu10 showed that patients with bilateral TKR significantly bled more than those who was given tranexamic acid intra-articular or intavenous. Moreover, Zhu10 also showed that the less drain volume existed, the less Hb decreased, and the less the need of transfusion in group with tranexamic acid compared to the control group.7 This result clearly implied the rule of tranexamic acid as anti-bleeding. Fibrinolisis was avoided because tranexamic acid competitively blocked the lisin receptor in plasminogen.8
Haemoglobin was measured serially before and until five days after operation. According to Zhu10 Hb measurement was the best way to predict intraoperative blood loss, especially for blood loss that could not be measured by drain. Formby et al11 showed that Hb rate in group which was given tranexamic acid tended to be higher compared to group without tranexamic acid. In all group, there was a trend of Hb decrease up to two days postoperatively. Meanwhile in intravenous tranexamic acid group, it kept on decreasing until the third day. This phenomenon is linear with the study held by Sabatini et al12 where Hb decreased in the first three days after operation. Delta Hb per day was calculated by distracting the preoperative Hb with the postoperative Hb. From this study, we know that the biggest delta Hb was in the intravenous tranexamic group in day two and day three and the control group in day two. Besides, there was no significant difference in delta Hb in each group. The importance of knowing preoperative Hb was explained by Basora et al.13 They concluded that low Hb preoperative was one of the predictor of red blood cell transfusion. Moreover, every 1 g/dL decreasing in Hb would increase the risk of transfusion 3.7 times.10
A good preoperative haemoglobin could predict the need for transfusion in operated patients generally. It was proposed that a low number of preoperative haemoglobin might increase the need for transfusion postoperative, necessitating a good preoperative blood preparation for patients in general. A lower preoperative haemoglobin level might be one of the reasons why the haemoglobin level for the intravenous group kept decreasing after the third day.10,14
Transfusion is the most important aspect in assesing preoperative bleeding. Administration of tranexamic acid intra-articular or intravenous had no significant difference in blood loss or transfusion rate.15-18 However, there was a significant difference between the group that was given tranexamic acid with the control group that was not given tranexamic acid in term of transfusion need. This result is linear with Sabatini et al12 whom stated that tranexamic acid had protective effect in the need of transfusion.
In conclusion, intra-articular and intravenous tranexamic acid group had better result in drain volume and transfusion volume needed in patient with grade III and IV OA who underwent TKA compared to the control group. Intra-articular or intravenous gave the same effects to patients with OA grade III and IV post-TKA. The control group had the biggest drain volume compared to other group and this result established the role of tranexamic acid in blocking bleeding in patients.
Conflicts of Interest
The authors affirm no conflict of interests in this study
Acknowledgment
Authors would like to give their best regards to the Department of Orthopaedy and Traumatology, Faculty of Medicine, Universitas Indonesia, and Cipto Mangunkusumo Hospital, for the support given in completion of this study
REFERENCES
- Civinini R, Nistri L, Martini C, Redl B, Ristori G, Innocenti M. Growth factors in the treatment of early osteoarthritis. Clin Cases Miner Bone Metab. 2013;10(1):26–9.
- Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH. Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc. 2010;42(10):1795–801.
- Molloy DO, Archbold HA, Ogonda L, McConway J, Wilson RK, Beverland BE. Comparison of topical fibrin spray and tranexamic acid on blood loss after total knee replacement: a prospective randomized control trial. J Bone Joint Surg Br. 2007;89(3):306–9.
- Turpie AG, Lassen MR, Davidson BL, Bauer KA, Gent M, Kwong LM, et al. Rivaroxaban versus enoxaparin for thrombophylaxis after total knee arthroplasty (RECORD4): a randomised trial. Lancet. 2009;373(9676):1673–80.
- Hame SL, Alexander RA. Knee osteoarthritis in women. Curr Rev Musculoskelet Med. 2013;6(2):182–7
- Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Casp J Intern Med. 2011;2(2):205–12.
- Karaaslan F, Karaoğlu S, Mermerkaya MU, Baktir A. Reducing blood loss in simultaneous bilateral total knee arthroplasty: combined intravenous-intraarticular tranexamic acid administration. A prospective randomized controlled trial. Knee. 2015;22(2):131–5.
- Iwai T, Tsuji S, Tomita T, Sugamoto K, Hideki Y, Hamada M. Repeat-dose intravenous tranexamic acid further decreases blood loss in total knee arthroplasty. Int Orthop. 2013;37(3):441–5.
- Chen JY, Rikhraj IS, Zhou Z, Tay DK, Chin PL, Chia SL, et al. Can tranexamic acid and hydrogen peroxide reduce blood loss in cemented total knee arthroplasty? Arch Orthop Trauma Surg. 2014;134(7):997–1002.
- Zhu Y YM, Meng HY, Way AY, Guo QY, Wang Y, Peng J. Basic science and clinical application of platelet-rich plasma for cartilage defects and osteoarthritis: a review. Osteoarthritis and Cartilage. 2013:1–11
- Formby P, Pickett AM, Van Blarcum GS, Mack AW, Newman MT. The use of intravenous tranexamic acid in patients undergoing total hip or knee arthroplasty: a retrospective analysis at a single military institution. Mil Med. 2015;180(10):1087–90.
- Sabatini L, Atzori F, Revello S, Scotti L, Debiasi F, Massè A. Intravenous use of tranexamic acid reduces postoperative blood loss in total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134(11):1609–14.
- Basora M, Tió M, Martin M, Lozano L, Salazar F, Sánchez- Etayo G, et al. Should all patients be optimized to the same preoperative haemoglobin level to avoid transfusion in primary knee arthroplasty? Vox San. 2014;107(2):140–52.
- Wong J, Abrishami A, El Beheiry H, Mahomed NN, Roderick Davey J, Gandhi R, et al. Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am. 2010;92(15):2503–14.
- Aguilera X, Martinez-Zapata MJ, Bosch A, Urrútia G, González JC, Jordan M, et al. Efficacy and safety of fibrin glue and tranexamic acid to prevent postoperative blood loss in total knee arthroplasty: a randomized controlled clinical trial. J Bone Joint Surg Am. 2013;95(22):2001–7.
- Panteli M, Papakostidis C, Dahabreh Z, Giannoudis PV. Topical tranexamic acid in total knee replacement: a systematic review and meta-analysis. Knee. 2013;20(5):300–9.
- Iwai T, Tsuji S, Tomita T, Sugamoto K, Hideki Y, Hamada M. Repeat-dose intravenous tranexamic acid further decreases blood loss in total knee arthroplasty. Int Orthop. 2013;37(3):441–5.
- Wang H, Shen B, Zeng Y. Comparison of topical versus intravenous tranexamic acid in primary total knee arthroplasty: a meta-analysis of randomized controlled and prospective cohort trials. Knee. 2014;21(6):987–93.
Copyright @ 2016 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id