
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Community Research
Association between obesity and behavioral/emotional disorders in primary schoolaged children: a cross-sectional study
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v26i1.1564 Med J Indones. 2017;26:70–5
Received: September 08, 2016
Accepted: February 17, 2017
Author affiliation:
Department of Child Health, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Corresponding author:
Rini Sekartini
E-mail: rsekartini@yahoo.com
Background
Obesity in children can increase the risks of various chronic diseases. Mental disorders associated with obesity in children include: depression, anxiety, low selfesteem, hyperkinetic disorders, and increased aggressiveness. This relationship is estimated due to vulnerable genetic expressions in obese individuals. This study aimed to find the association between obesity and behavioral/emotional disorder in primary school-aged children.
Methods
This cross-sectional study was conducted on 384 children at Menteng 1 Elementary School, Jakarta from July to September 2015. The study was conducted to find the association between the children’s nutritional status and behavioral/emotional disorders screened by the 17-item Pediatric Symptom Checklist (PSC-17). Chi square analysis was applied in this study.
Results
The prevalence of obese children at Menteng 1 Elementary School, Jakarta reached 23.2%, which is higher than Jakarta’s prevalence (14%). 8.7% of the subjects were obese and 13.6% of them were having behavioral/emotional disorders. 20.0% of the obese subjects had behavioral/emotional disorders. The prevalence was higher for internalizing subscale, which was consistent with other studies. Association between obesity and behavioral/emotional disorders was significant for externalizing sub-scale (p=0.036). Externalizing problems caused by obesity might be affected by the social stigma of their peer group. However, obesity in children did not have a statistically significant relationship in internalization sub-scale, attention, and PSC-17 total score (p>0.05). No significant associations towards those sub-scales were thought to be influenced by other factors, playing a role in causing mental disorders in children.
Conclusion
In general, obesity was not associated with behavioral and emotional disorders in children, but obesity was related to externalizing behavioral/emotional disorders.
Keywords
behavioral disorders, children, emotional disorders, obesity, PSC-17
Obesity in children is a pandemic problem, commonly found not only in developed countries, but also in developing countries.1 In 2013, there were 18.8% of children aged five to 12 years in Indonesia who were overweight and obese, which 10.8% of them classified as overweight and 8% obese. The highest prevalence was found in Jakarta, as many as 30.1% including 14% obese and 16.1% overweight.2 The increasing prevalence of obesity in children is important to be explored further because obesity can increase the risk of various chronic diseases both physically and mentally. Obesity in children is associated with mental illnesses such as: depression, anxiety, low selfesteem, eating disorders (bulimia), hyperkinetic disorders, and increased aggressiveness.3,4
In Jakarta, Harahap et al5 found that there were 22% obese children with emotional and behavioral problems. This study was conducted using the 17-item Pediatric Symptom Checklist (PSC-17), which was as good as the gold standard method to screen emotional and behavioral problems in children. This was the first study to evaluate emotional and behavioral problems in Indonesian children, in which the association between obesity and emotional/behavioral problems was still not well acknowledged.5 Therefore, the purpose of this study is to further find the association between obesity and behavioral/emotional disorders in Indonesian children.
METHODS
A cross-sectional study was conducted from July to September 2015 at Menteng 1 Elementary School, Jakarta. The protocol of the study has been approved by Medical Ethics Committee of Universitas Indonesia (No. 583/UN2.F1.D1/ KBK/PDP.01/2015). An amendment of ethical clearance for the revision of this study’s title had also been approved by the same institution (No. 828/UN2.F1.D1/KBK/PDP.01/2015). All 384 students enrolled in the school during the period of study were included. The parents were asked to fill a written consent of their child’s enrollment in this study. All subjects underwent anthropometric (height and weight) measurements to determine each subject nutritional status based on their body mass index (BMI). We supervised each data collection using the same tools: one height scale (Seca-206) and one weight scale (Seca-704) for all subjects to prevent bias. Each subject’s height and weight were measured three times, and the mean value from those measurements was taken into BMI calculation. Both scales were calibrated by putting the scales back to zero every time before the next subject’s measurements. Height measurements were taken by instructing the subjects to stand upright with both ankles touching the wall behind them, while maintaining their heads and eyes straight forward.
We obtained all of the subjects’ nutritional status by plotting each subject’s height and weight to the National Center for Health Statistics-Centers for Disease Control and Prevention (NCHS-CDC) growth charts. BMI was retrieved by dividing their weights (kg) by the square of their heights (m2). The subjects were classified as obese when their BMI using CDC-NCHS (kg/m2) were at the 95th percentiles and above.6
We then gave the 17-item PSC-17 to 384 subjects who had done the measurements. Eighteen subjects were excluded because they wrote down in the informed consent (given in a bundle with the questionnaires) that they did not want to participate in this study. Ten subjects did not complete all the questions and/or put more than two answers in the same question, so their questionnaires became invalid and were dropped out from the study. In the end, 103 subjects completed valid PSC-17 questionnaires, and therefore were included in the data analysis.
Each parent of the subjects completed the PSC- 17 based on their observation toward their child’s behavior. This screening tool consists of 17 items as a short form of PSC, which is divided in three sub-scales: internalizing, externalizing, and attention. Internalizing subscale covers emotional disorders such as depression and anxiety, which are screened by these symptoms: “feels sad, unhappy”, “feels hopeless”, “is down to self”, “seems to be having less fun”, and “worries a lot”. Externalizing sub-scale covers behavior disorders such as conduct disorder and aggressive-disruptive behavior, which are screened by these symptoms: “refuses to share”, “does not understand other people’s feelings”, “fights with other children”, “blames others for his/her troubles”, “does not listen to rules”, “teases others”, and “takes things that do not belong to him/her”. Furthermore, attention sub-scale covers attention deficit-hyperactivity disorder, which is screened by following symptoms: “fidgety, unable to sit still”, “daydreams too much”, “has trouble concentrating”, “acts as if driven by a motor”, and “distracted easily”.5
Parents rated each item based on the frequency of “never”, “sometimes”, or “often”. Their responses were then scored as 0, 1, or 2, respectively. We used the cut off score ≥5 for internalization sub-scale, ≥7 for externalization sub-scale, ≥7 for attention sub-scale, and ≥15 for total score.5 Gardner et al7 instructed to give the number 0 on items that were not answered, and the questionnaire was still considered valid if there was maximal one unanswered item for each subscale. This policy was applied in this study. Hence, some questionnaires with two answers in one question were considered invalid.
The independent variable in this study was the nutritional status, whereas the dependent variable was the PSC-17 result. We used the chisquare test to find the association between obesity of each subscale (internalizing, externalizing, attention), the total score, and the positive PSC-17 result.
RESULTS
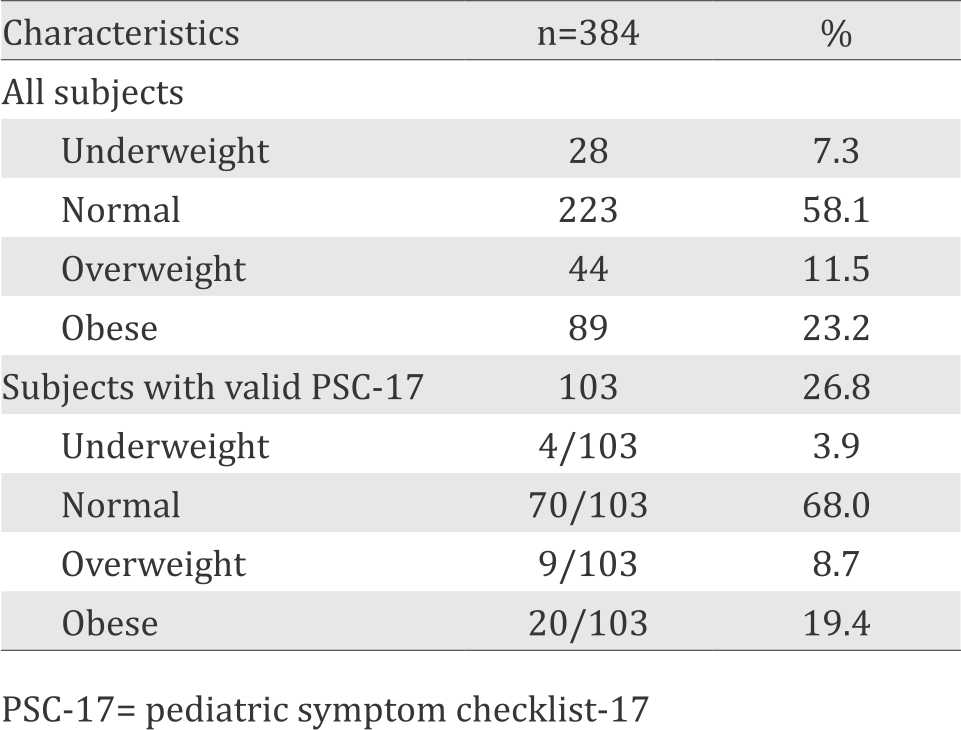
We calculated 384 eligible subjects’ BMI to find their nutritional status. Their age ranged from six to 12 years, with 199 subjects (51.8%) were male. We found that 89 children (23.2%) were obese, with composition of 60 (15.6%) males and 29 (7.6%) females. Only 103 of 384 subjects (26.8%) returned and completed the valid PSC- 17 questionnaires. Twenty children (19.4%) were obese, with 14 males and six females (Table 1).
Table 1. Subjects’ nutritional status
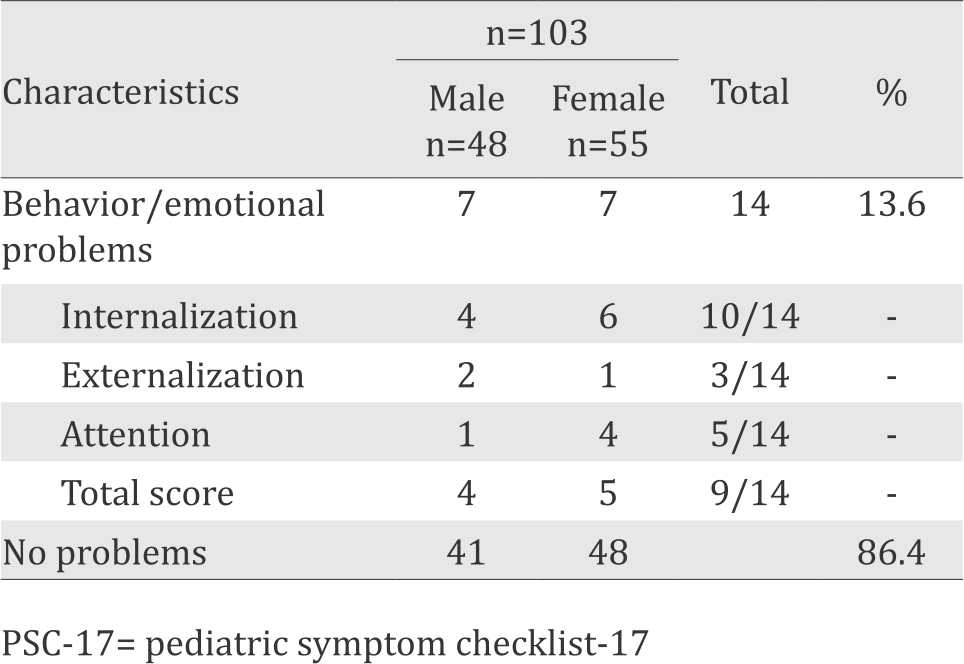
PSC-17 detected that 14 of 103 (13.6%) children had behavioral/emotional problems (table 2). Ten children were positive for internalization sub-scale, three for externalization sub-scale, and five for attention sub-scale. There were also nine children who were positive based on total score cut off. There were two of 20 obese children with behavioral/emotional disorders.
Table 2. PSC-17 results
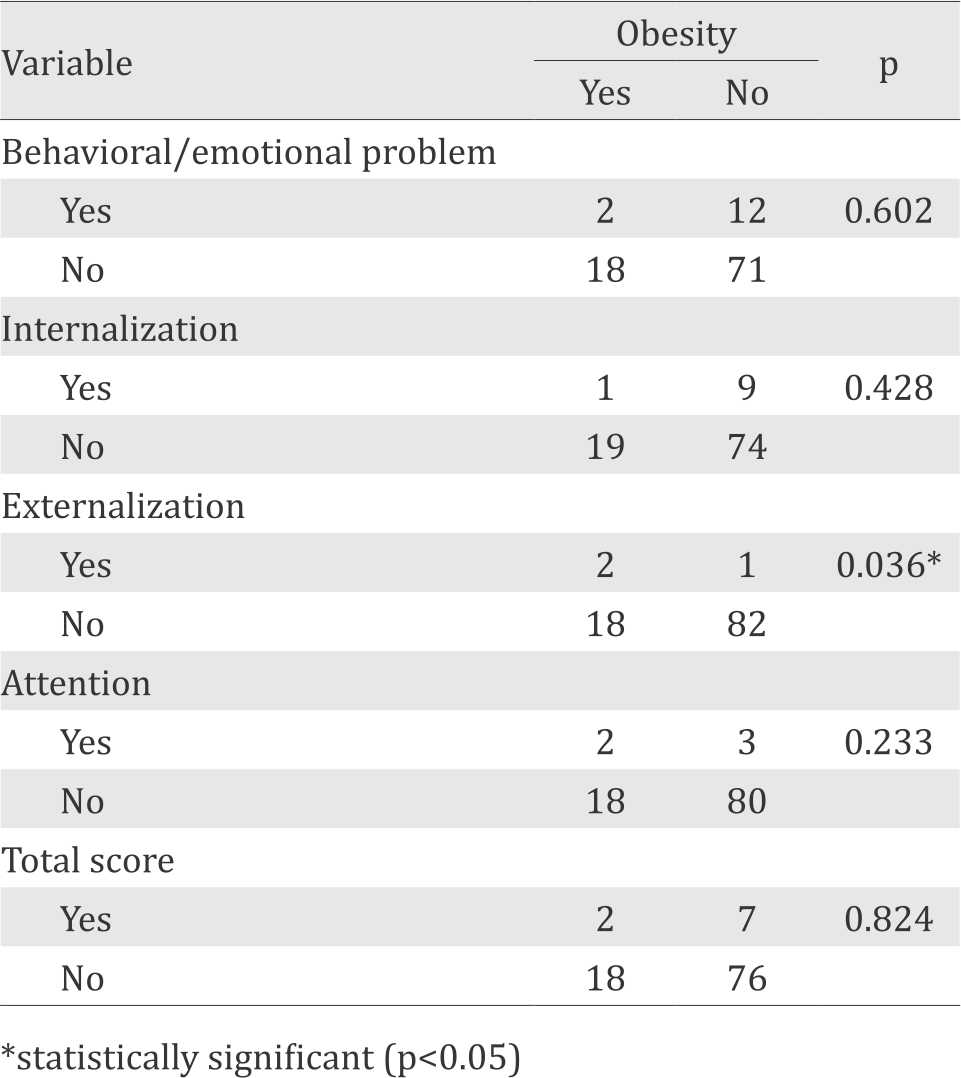
We analyzed the data using the chi-square test and found that the association was significant between obesity and externalization sub-scale (p=0.036). There were no significant association (p>0.05) between obesity and internalization sub-scale, attention sub-scale, total score, and emotional/behavior in general (positive PSC-17 result) (Table 3).
Table 3. Association between obesity and behavioral/emotional disorders
DISCUSSION
This was the first study in Indonesia to find the relationship between obesity and behavioral/ emotional disorder in primary school-aged children using PSC-17. The prevalence of obese children at Menteng 1 Elementary School, Jakarta reached 23.2% (Table 1). This prevalence was higher than the prevalence of obese children aged 5-12 years according to the basic health research in 2013 for Jakarta province, which was 14%.2
The use of PSC-17 is quite fast and easy to complete. However, the questionnaire return rate was only 34.1%. It was because the study method needed the child’s responsibility to bring home the questionnaire and return it afterward by themselves. From data in table 1, it could be concluded that the proportion of the samples with valid PSC-17 were still comparable to the school’s population; therefore, the low questionnaire return rate should not be regarded as a problem.
Based on the screening done by PSC-17, positive results were obtained as 13.6% of the total sample (Table 2). This was lower compared to other studies in Indonesia, which showed positive prevalence of 22-29%.5,8 This difference was predicted to be caused by different sample sizes and data retrieval method. The PSC-17 data collection in one study was done using verbal interviews to parents instead of self-filled.8
Internalization sub-scale had higher prevalence compared with other sub-scales (10 of 14). It was consistent with Harahap et al5 (17 of 21) and Handayani et al8 (25 of 36). This aligned with the theory that internalization disorders (i.e. depression, low self-esteem, anxiety) was the dominant psychopathology at the age of 6–12 years. At this age, children’s cognitive develops self-evaluation and recognition towards other people’s judgement. They will be more susceptible to feel depressed or anxious because they feel themselves not as good as their friends or the society’s expectation.9
In general, there was no significant association between obesity and behavioral/emotional disorders in primary school-aged children (Table 3). According to other studies, there should be a significant association between obesity and behavioral/emotional disorders. It was associated with changes in gene expression in susceptible obese individuals.10-12 However, no clear mechanism had been found yet.13 Also, epidemiological differences should be considered knowing that those studies were not conducted in Indonesia, which could influence the genetic expression. Moreover, although PSC-17 was fast and easy to use, this tool had generally low sensitivity (40–60%) to screen behavior/ emotional disorders.7 We recommend to use more sensitive tools for further studies.
This study found no significant association for internalizing sub-scale (p>0.05). Erickson et al14 suggests that there was a significant association between obesity and depression in third grade girls using the Children’s Depression Inventory (CDI). This difference was presumably caused by the fact that CDI was more sensitive to screen depression than PSC-17.14 Anxiety disorders had the highest prevalence in school-aged children7,8 and was higher than depression.7 However, the PSC-17 was less sensitive to detect children with anxiety disorders because there was only one item that refers to anxiety7. Thus, the association between obesity and anxiety disorders was difficult to assess using this tool.
Moreover, there was a significant association between obesity and externalizing disorders (p=0.036). This was consistent with Zeller et al15 which studied children aged 8–16 years and found the association between obesity and aggressivedisruptive disorders. It is suggested that people will tend to judge a group of obese individuals with aggressive-disruptive behavior (p=0.03).15 The social stigma of peer group was probably related to an increase in aggressive-disruptive behavior. Halfon et al4 also noted a statistically significant association between obesity and conduct disorders including defiant disorders (p<0.001) in children aged 10–17 years.4
Studies in the US and Germany suggested that there was a significant association between obesity and attention deficit-hyperactivity disorder (ADHD) (p<0.05).16,17 However, it was not clearly known whether obesity caused ADHD or otherwise. One theory suggested that obesity was a result of increased appetite caused by stimulant consumption for ADHD treatment.16,18 Another theory suggested that there was a similar neurological dysfunction in obesity and ADHD.18 The difference in this study compared to other studies were likely due to the sensitivity of PSC-17, which was not adequate for diagnosing ADHD.7
Obesity also has no significant relationship with the results of the PSC-17 total score (p=0.824). There was no research data that specifically addressed this topic. Serrano-Gonzalez et al. suggested a positive association between high levels of non-HDL cholesterol to high PSC scores (p=0.02).19 However, our study showed different results because we used PSC-17 instead of PSC-35, which had more items than PSC-17, as in the previous studies. In addition, sensitivity of the PSC-17 based on cut-off 15 points for total score was only 42%. It means that the positive results of PSC-17 only detected 42% of the total population truly having behavioral/emotional disorder compared to gold standard.7 Thus, the insignificant association in this study could be ignored.
This study was limited by no control towards whether the parents filled the PSC-17 based on their child real behavior or not because we found that there were a lot of parents who filled the questionnaire as “never” for all items, which could not be consistent with their children true behaviors. We thought that the society in Indonesia still thinks that mental disorder is something to be ashamed of, so they would not truly fill the form to find out the truth. Crosssectional method in this study also limited us to evaluate the duration of obesity a child had until the onset of behavioral/emotional disorders. Therefore, no association between obesity and behavioral/emotional disorders was caused by the possibility that the subjects had not yet built up significant symptoms to be detected as a disorder by PSC-17 because most of mental illnesses are chronic diseases. To assess this topic, further research should be done with the cohort method and using more sensitive screening tools for detecting mental disorders in children.
In conclusion, there was no significant association between obesity and behavioral/emotional disorders in primary school-aged children. However, there was a significant association between obesity and behavioral/emotional disorders in primary school-aged children for externalizing sub-scale.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None
REFERENCES
- Ng M, Fleming T, Robinsin M, Thomson B, Greaetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
- Kementerian Kesehatan Republik Indonesia. Riset Kesehatan Dasar. Jakarta: Badan Penelitian dan Pengembangan Kesehatan; 2013. p. 217–8.
- Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360(9331):473–82.
- Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr. 2013;13(1):6–13.
- Harahap DF, Sjarif DR, Soedjatmiko, Widodo DP, Tedjasaputra MS. Identification of emotional and behavior problems in obese children using Child Behavior Checklist (CBCL) and 17-items Pediatric Symptom Checklist (PSC- 17). Paediatr Indones. 2010; 50(1):42–8.
- Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl4):164–92.
- Gardner W, Lucas A, Kolko DJ, Campo JV. Comparison of the PSC-17 and alternative mental health screens in an at-risk primary care sample. J Am Acad Child Adolesc Psychiatry. 2007;46(5):611–8.
- Handayani D, Rismarini, Kesuma Y, Purnamasari R, Husin S. Hubungan defisiensi besi dengan perilaku anak usia sekolah di kota Palembang. Sari Pediatr. 2015;16(5):307–14. Indonesian.
- Feigelman S. Middle childhood. Chapter 11. In: Kliegman RM, Stanton BF, Schor NF, St Geme JW, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia (PA): Elsevier Saunders; 2011. p36–9.
- Cortese S, Vincenzi B. Obesity and ADHD: clinical and neurobiological implications. Curr Top Behav Neurosci. 2012;9:199–218.
- Breuillaud L, Clara Rossetti, Elsa MM, Cristophe Mérinat, Olivier Halfon, Pierre Magistretti, et al. Deletion of CREB-regulated transcription coactivator 1 induces pathological aggression, depression-related behaviors, and neuroplasticity genes dysregulation in mice. Biol Psychiatry. 2012;72(7):528–36.
- Williams MJ, Goergen P, Rajendran J, Klockars A, Kasagiannis A, Fredriksson R, et al. Regulation of aggression by obesity-linked genes TfAP-2 and Twz through octopamine signaling in Drosophila. Genetics. 2014;196(1):349–62.
- Benson LP, Williams RJ, Novick MB. Pediatric obesity and depression: a cross- sectional analysis of absolute BMI as it relates to children’s depression index scores in obese 7- to 17-year-old children. Clin Pediatr (Phila). 2013;52(1):24–9.
- Erickson SJ, Robinson TN, Haydel KF, Killen JD. Are overweight children unhappy?: Body mass index, depressive symptoms, and overweight concerns in elementary school children. Arch Pediatr Adolesc Med. 2000;154(9):931–5.
- Zeller MH, Reiter-Purtill J, Ramey C. Negative peer perceptions of obese children in the classroom environment. Obesity (Silver Spring). 2008;16(4):755–62.
- Curtin C, Bandini LG, Perrin EC, Tybor DJ, Must A. Prevalence of overweight in children and adolescents with attention deficit hyperactivity disorder and autism spectrum disorders: a chart review. BMC Pediatr. 2005;5:48.
- Holtkamp K, Konrad K, Müller B, Heussen N, Herpertz S, Herpertz-Dahlmann B, et al. Overweight and obesity in children with attention- deficit/ hyperactivity disorder. Int J Obes Relat Metab Disord. 2004;28(5):685–9.
- Cortese S, Angriman M, Maffeis C, Isnard P, Konofal E, Lecendreux M, et al. Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Crit Rev Food Sci Nutr. 2008;48(6):524–37.
- Serrano-Gonzalez M, McConnel C, Bokhary M, Oden J, Lopez X. Association of non- high-density lipoprotein cholesterol with psychosocial dysfunction in children and adolescents with obesity. Child Obes. 2015;11(5):647–9.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id