
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Community Research
Association between public knowledge regarding antibiotics and self-medication with antibiotics in Teling Atas Community Health Center, East Indonesia
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v26i1.1589 Med J Indones. 2017;26:62–9
Received: September 26, 2016
Accepted: February 20, 2017
Author affiliation:
1 General Practitioner, Teling Atas Primary Health Care, Manado, Indonesia
2 Department of Pharmacology and Therapy, Faculty of Medicine, Sam Ratulangi University, Manado, Indonesia
Corresponding author:
Kurniawan
E-mail: kurniawan.fatoni@hotmail.com
Background
Self-medication with antibiotics increases the risk of resistance, which leads to higher morbidity and mortality. The community plays an important role in preventing and controlling the spread of antibiotic resistance. This study aims to determine factors associated with antibiotics self-medication practices in the community, which are the key to developing effective intervention programs.
Methods
This cross-sectional study was conducted between September and October 2015 at Teling Atas Community Health Center in Wanea, a sub-district of East Indonesia region. Data was collected by a questionnaire-guided interview. There were 35 questions which cover respondent demographics, antibiotic use, and respondents’ knowledge about antibiotics. Logistic regression was used to analyze the association between self-medication with antibiotics and respondents’ level of knowledge as well as other factors.
Results
Among 400 respondents, there were 240 (60%) who had used antibiotics within 6 months prior to the interview and 180 (45.0%) who had self-medicated. Wounds or skin diseases (32.2%) were main reasons for self-medication. The majority of respondents self-medicated on their own initiatives (70.6%) and purchased antibiotics in pharmacies (52.2%). The mean score for respondent knowledge about antibiotic was categorized as “moderate” (score 7.14±2.49). Respondents with lower knowledge scores had higher probabilities to self-medicate with antibiotics than those with higher scores (OR= 16.86; 95% CI= 4.25–66.83).
Conclusion
Self-medication practices with antibiotics in this study are associated with age, family income, and knowledge. Since poorer knowledge about antibiotics is associated with a higher probability of self-medication with antibiotics, education programs to improve public awareness are needed.
Keywords
antibiotics, knowledge, resistance, self-medication
Since the discovery of Penicillin in 1928, antibiotics have been playing an important role in the treatment of infectious diseases, one of the leading causes of death.1,2 Unfortunately, many antibiotics have been less efficacious due to increased resistance. This condition has become a global health problem.2–5
The impact of antibiotic resistance is devastating to patients, the community, and healthcare. It reduces the efficacy of treatment which subsequently poses patients to higher morbidity and mortality up to two-folds and longer duration of treatment.1,5,6 Patients may also need second or even third-line antibiotics to cure their infections and will be burdened with higher cost consequently.1,2,6 At worst, the increasing number and spreading of resistant bacteria put us on the cusp of a post-antibiotic era when common infections and minor injuries could cause death.1
A study conducted in Surabaya and Semarang showed that 54% of individuals, either in the community or hospitals, had carried resistant Escherichia coli.7 Self-medication has been proven to be one of the causes of antibiotic resistance.8,9 Widayati et al10 found that the 7.3% of people in Yogyakarta had self-medicated with antibiotics. The prevalence was higher (17%) in another study held in teaching hospitals and public health centers in Surabaya and Semarang.11 In those studies, self-medication practices were predisposed by multiple factors, such as lack of knowledge about antibiotics, poor access to the health facilities, highcost low-quality health services, poor regulation, and lack of control by the government.8–10
The role of the community in controlling the spread of resistance is essential. Appropriate use, such as not taking antibiotics without a prescription, taking antibiotics exactly as directed, not using leftover antibiotics from previous treatments, and not giving nor suggesting antibiotics to others based on prior personal medical history, can help prevent the grim prospect of antibiotic resistance mentioned previously.12
The World Health Organization (WHO) has urged its members to start educating and increasing people’s awareness towards proper antibiotic use as one way to control the spread of antibiotic resistance.2,4–6 Since self-medication is not only influenced by knowledge and belief at individual level but also by economic and socio-demographic factors which differ across regions, it is important to first identify what factors contribute to it.5,6,8,13,14 Unfortunately, those data are still limited in Indonesia, and most of the studies were conducted in Java.
The purpose of this study is to determine public knowledge regarding antibiotics and other determinants of self-medication with antibiotics. The result of this study is expected to be a valuable input to develop effective community education programs to raise public awareness of antibiotic resistance as well as appropriate use of antibiotics.
METHODS
This cross-sectional study was conducted in Wanea, a sub-district of Manado, North Sulawesi, East Indonesia, between September and October 2015. A questionnaire-structured interview with each subject was performed to collect data. This study had been approved by the Integrated Health Research Unit, Prof. Dr. R. D. Kandou General Hospital (No. 082/EC-UPKT/IX/2015). Each respondent was asked for a written consent after being provided information about the study.
The study population was Teling Atas Community Health Center visitors, the only community health center in Wanea, North Sulawesi, Indonesia. A total of 400 samples were recruited using consecutive sampling. Inclusion criteria were as follows: (1) patients who were Wanea sub-district residents, (2) aged ≥18 years old, (3) able to speak Bahasa Indonesia, and (4) willing to participate in this study.
Visitors who fulfilled the above criteria were then informed about the purpose, benefit, and procedure of this study. Those who agreed to participate were asked for a written consent by the interviewer. The next step was the interview guided by a questionnaire which had been adapted from previous studies.4–6,14,15 An interview was considered finished when a respondent had answered all questions or withdrew his/her participation from this study. Incomplete questionnaires were excluded from the study. Data collection was performed by the first author, assisted by six medical doctors.
A total of 35 questions in the questionnaire were divided into three sections as follows: (1) 8 questions about respondent demographics, (2) 13 questions about recent antibiotic use by the respondent within the past six months, and (3) 14 questions about the respondent’s knowledge regarding antibiotics (the role of antibiotics, identification of antibiotics, adverse effects of antibiotics, and antibiotic use). Self-medication was defined as the use of any antibiotics without a prescription within six months prior to the interview.4–6,16
Respondents’ knowledge about antibiotics was assessed based on 14 questions in the third section of the questionnaire; all of which must have been answered with “yes”, “no”, or “do not know”. Each correct answer was given 1 point while each wrong or “do not know” answer was given 0 point. Hence, the maximum possible score was 14. Respondents’ levels of knowledge were classified into 3 categories, i.e. low (score 0–4), moderate (score 5–9), and high (score 10–14). Before being used for the survey, the questionnaire had been pretested to 30 individuals whose characteristics were similar to the study population in order to verify the clarity of the language used and the questionnaire’s structure. Wording revision had been done accordingly. A Cronbach’s alpha of 0.71 means that the reliability of the questionnaire is acceptable.
Data was processed using the Statistical Package for the Social Sciences (SPSS) version 15 for Windows. Descriptive statistics of respondents’ demographic profile, antibiotic use, and knowledge about antibiotics used 95% confidence interval. A bivariate analysis was performed to determine the association between respondents’ demographics and self-medication with antibiotics. Any associations with p<0.05 were considered statistically significant, and the variables were included in the subsequent logistic regression analyzing the association between respondents’ knowledge score with self-medication practices. Results of the logistic regression analysis are presented as adjusted odd ratios (OR), each with 95% confidence interval.
RESULTS
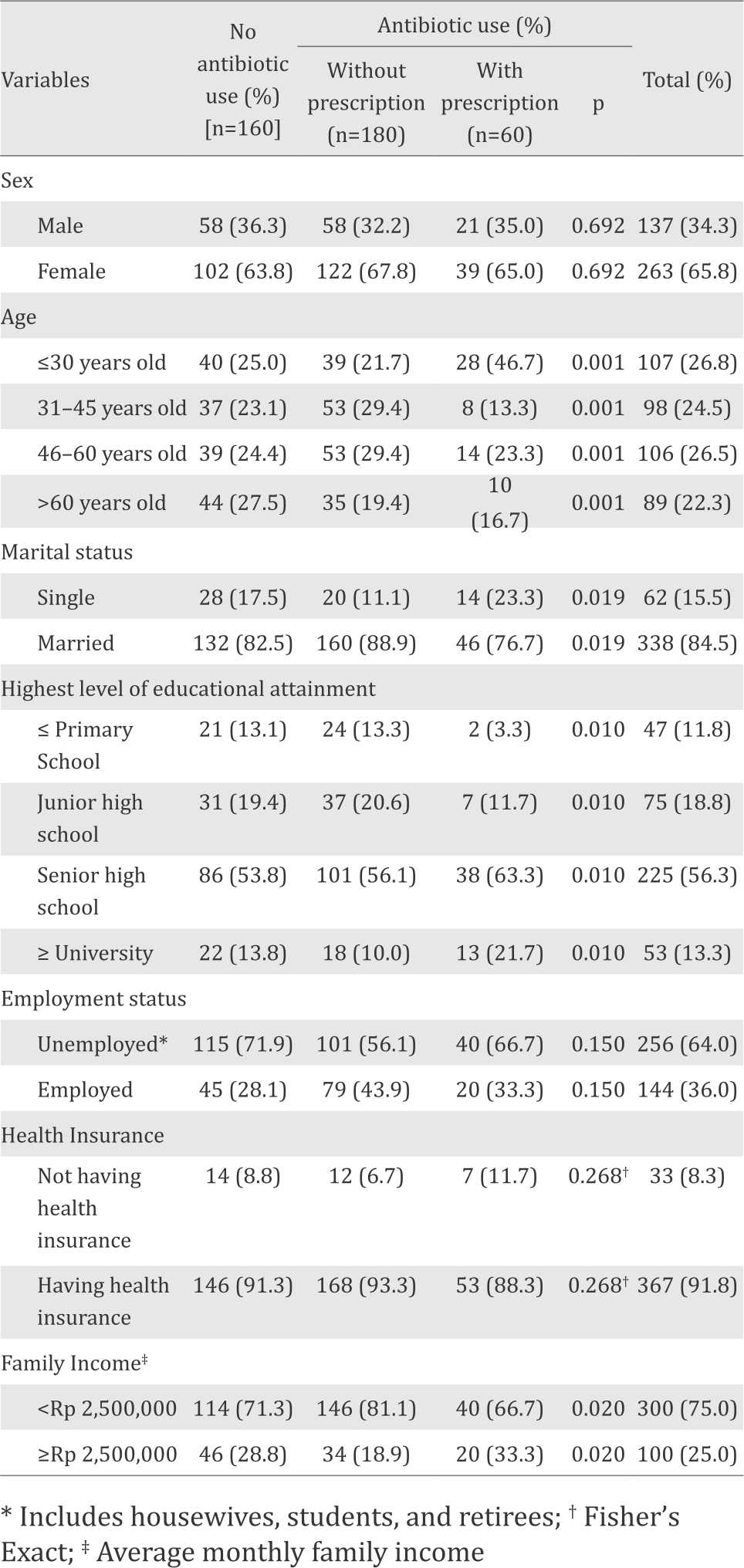
A total of 400 individuals were studied. The median age of respondents was 45.0 (18–49) years old. The majority of respondents were female (65.8%) and senior high school graduates (56.3%). The respondents’ demographics are presented in Table 1.
Table 1. Respondent’s demographics
In this study, almost half (45%) of the respondents had self-medicated with antibiotics within six months prior to the interview. Wounds or skin diseases (32.2%), acute respiratory infections (18.3%), and fever (11.7%) were the main reasons to take antibiotics without any prescriptions. (Table 2).
Table 2. Characteristics of self-medication
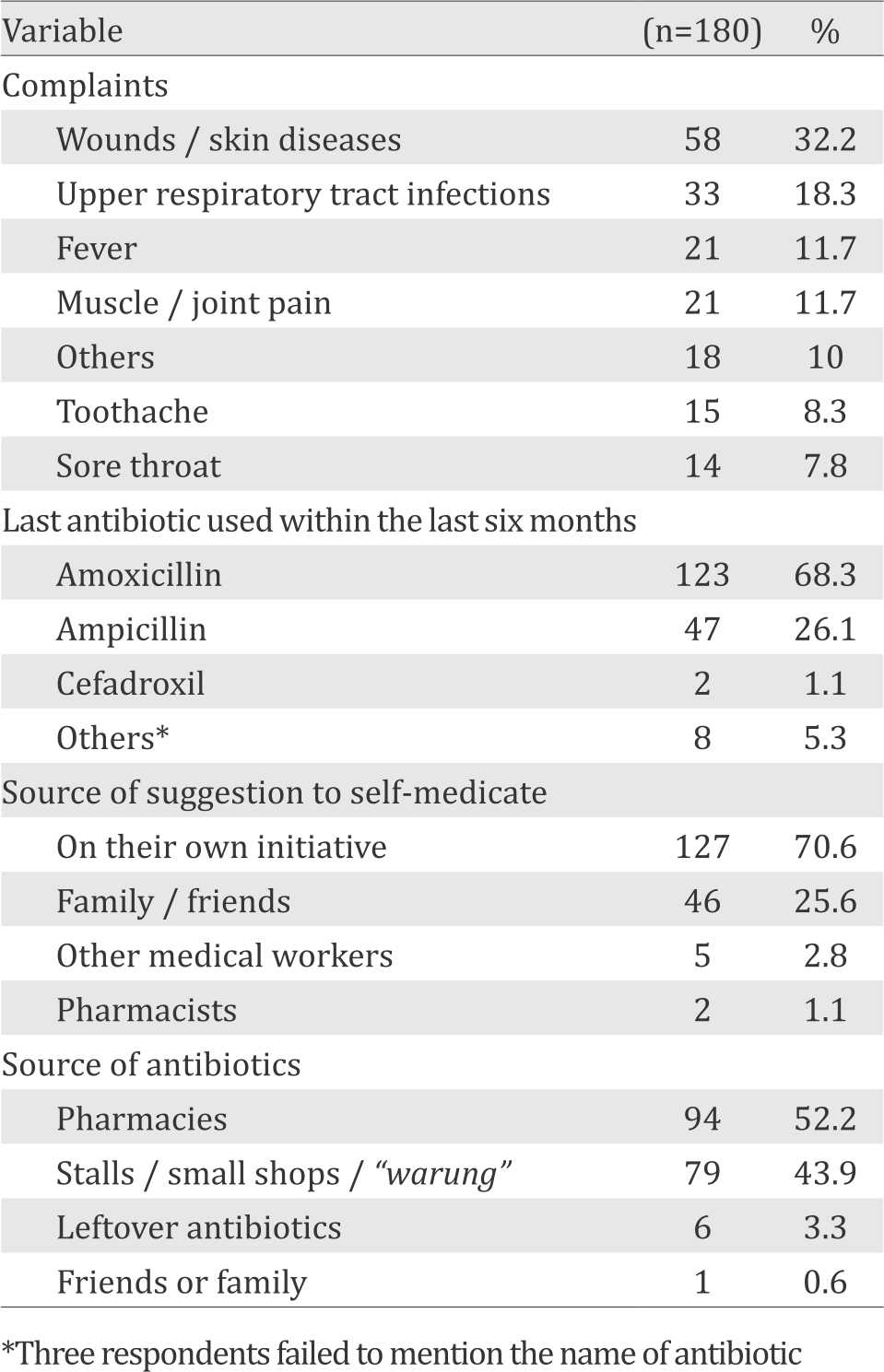
More than half of respondents who selfmedicated (n=100; 55.6%) stated that doing so was more practical than seeking a doctor for a treatment. Slightly more than one-fourth (26.7%) of respondents said that they were too busy to see a doctor, whereas another 14.4% had used the same antibiotic as the one medically prescribed for similar complaint in the past. On the other hand, six (3.3%) respondents self-medicated because they did not have enough money to pay for the doctor visit.
Most respondents (70.6%) self-medicated on their own initiative and purchased antibiotic in pharmacies (52.2%). When asked about their opinions regarding safety of self-medication, 122 (67.8%) respondents considered the practice was safe, 41 (22.8%) thought it was dangerous, and 17 (9.4%) could not answer the question.
The mean value of knowledge score in this study was 7.14±2.49. The majority of respondents (67.5%) had moderate level of knowledge, whereas respondents with high and low level of knowledge comprised 18.0% and 14.5% of the sample, respectively.
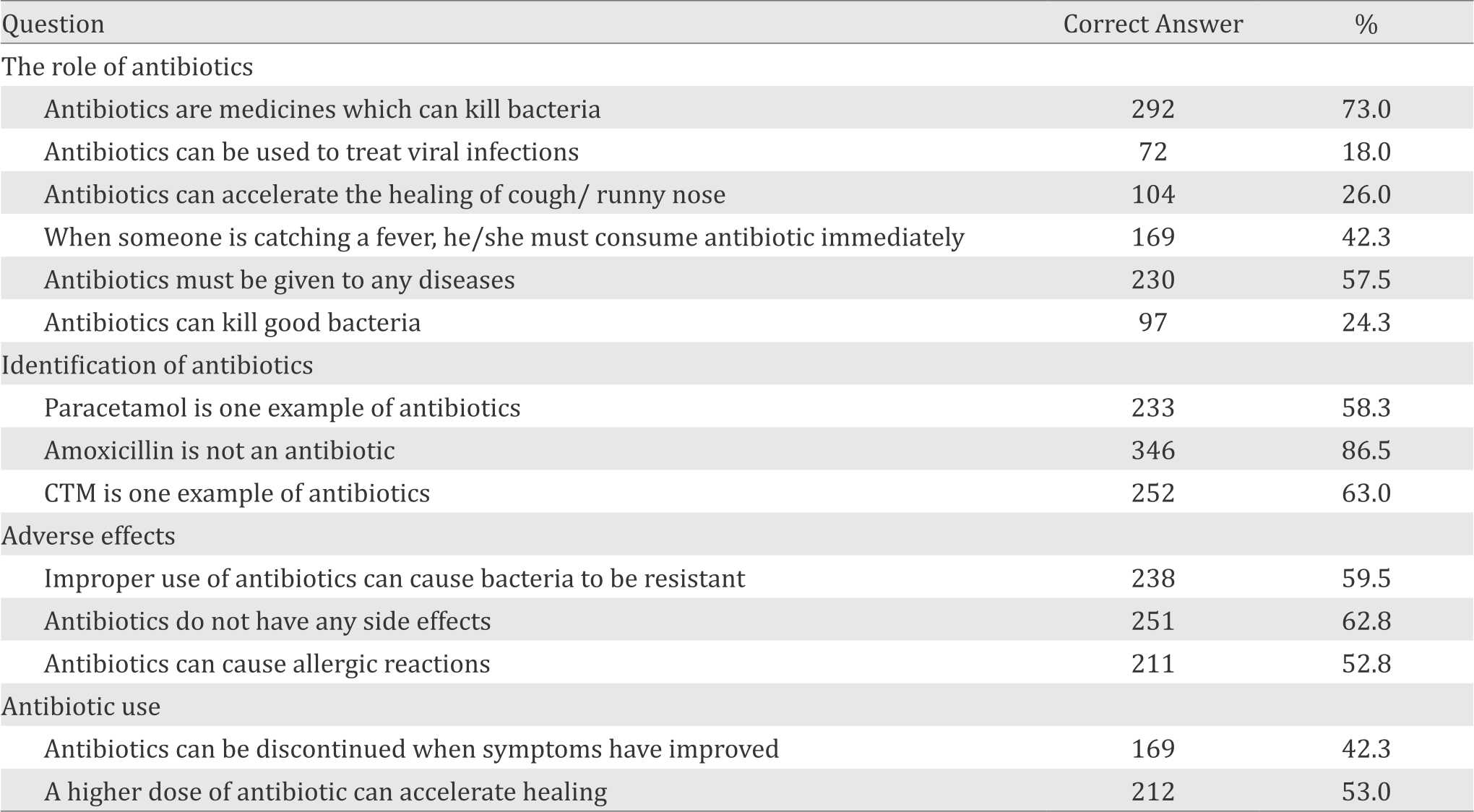
Table 3 displays respondents’ knowledge about antibiotics. A large number of respondents (73.0%) knew that antibiotics target bacteria, but only less than one-fifth (18.0%) of respondents knew that antibiotics do not play any role in viral infections. Meanwhile, there were a lot of patients (74.0%) in our study who thought that antibiotics could accelerate the healing of cough or runny nose. Although 59.5% of respondents knew that improper use of antibiotics could lead to resistance, only 24.3% of respondents knew that antibiotic use could kill good bacteria.
Table 3. Respondents’ knowledge about antibiotics
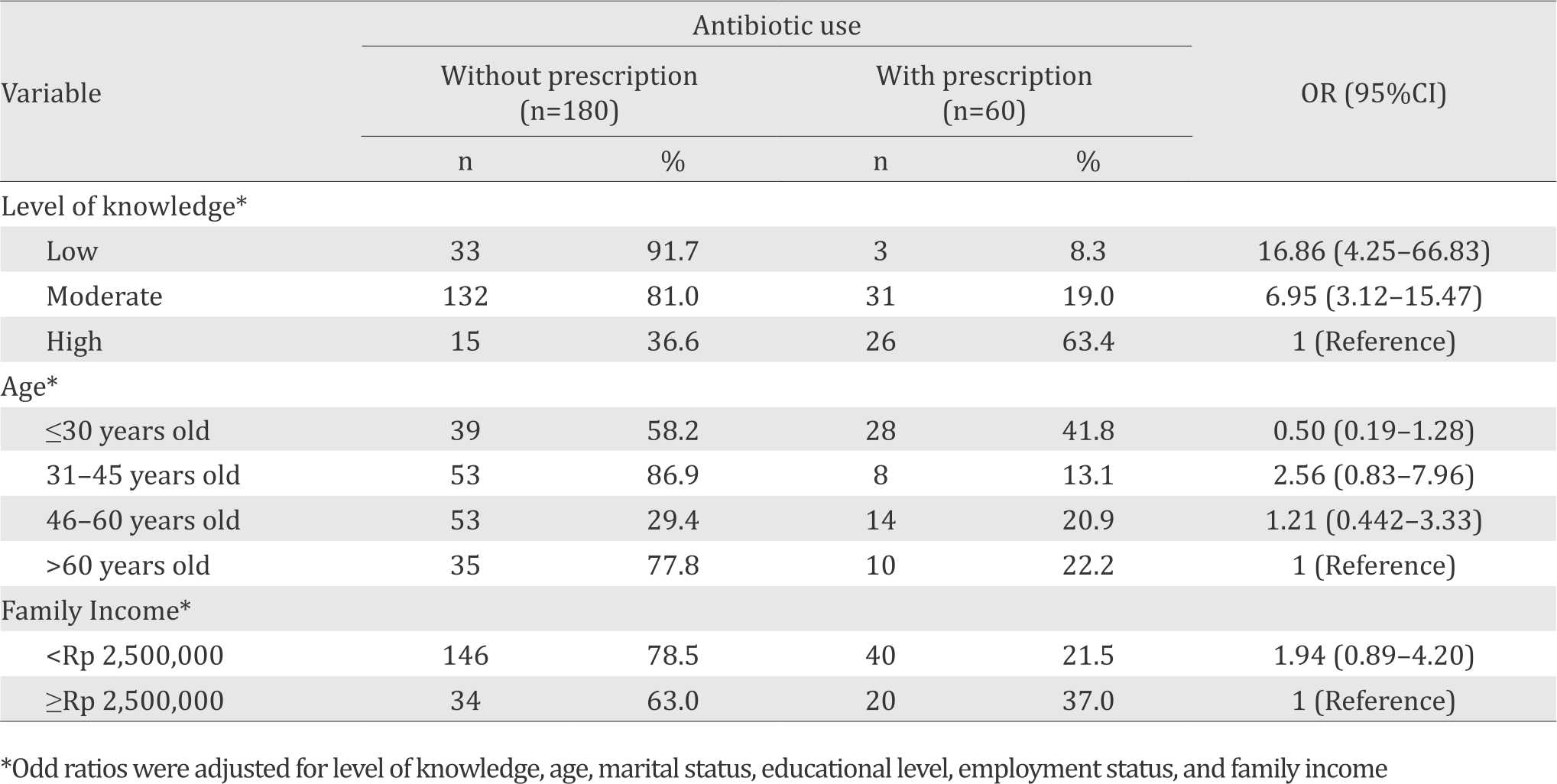
Respondents’ age, marital status, highest level of educational attainment, family income, and knowledge about antibiotics were all significantly associated (each has a p<0.05) with self-medication practices (Table 1). All of them were then included in the multivariate analysis where knowledge was an independent variable, and the rest were confounders. After having adjusted for age, marital status, education, employment status, and family income, the final logistic regression model came up with a significant association between knowledge about antibiotics and selfmedication practices. Respondents with lower level of knowledge have higher probabilities to self-medicate with antibiotics than those with higher level (OR= 16.86; 95% CI= 4.25–66.83) (Table 4).
Table 4. Associations between knowledge and self-medication
DISCUSSION
The prevalence of self-medication within six months prior to the interview in Wanea was 45.0%. This result is greater than the prevalence in Kuwait, Abu Dhabi, and Greece which were 27.5%, 44.0%, and 44.6%, respectively.5,16,17 It is strikingly higher than the finding of another study in Putrajaya and Penang, Malaysia, Indonesia’s neighboring country, which came up with 4.5% and 7.6%, respectively.4,15 When compared to previous studies in Semarang-Surabaya (17.0%) and Yogyakarta (7.3%), all of which located in Java island, the result of our study still shows a remarkably higher number.10,11
In this study, wounds and skin diseases were two main reasons for respondents to take antibiotics without a prescription. This finding is different from other studies that showed acute respiratory infection as the major cause of self-medication with antibiotics.4,5,10
Although the majority (67.8%) of respondents who self-medicated were female, we cannot yet conclude whether women tend to self-medicate rather than men because during our study, the Wanea community health center was mostly visited by women (65.8%). However, we should acknowledge that women could play an important role in preventing self-medication with antibiotics, especially in children. A study in Peru that aimed to determine factors affecting caregivers’ decisions about antibiotic use in children showed that 15.9% of children had received antibiotics without a prescription.18 In China, 62.0% of parents had selfmedicated their children with antibiotics.19 As a mother, a woman does not only act as the caregiver in her family, but also the central decision maker regarding her family’s health.
The level of knowledge about the role of antibiotics in viral infections is lower when compared to other studies conducted in Yogyakarta (29.0%), Kuwait (29.8%), South Korea (30.6%), and Sweden (73.2%).5,6,10,20 It is shown by the relatively high number of respondents who did not know that antibiotics have no role in viral infections, despite the fact that a lot of them had known that the target of antibiotics is bacteria. Moreover, many still thought that antibiotics could speed up the healing of cough or runny nose and that antibiotics should be given to all diseases. Those data display respondents’ lack of knowledge about the role of antibiotics in the treatment of infectious diseases in general.
The level of knowledge regarding appropriate use of antibiotics was also low. More than half (57.7%) of respondents said antibiotics should be discontinued when symptoms had improved. There were 40.5% of respondents who were not aware that inappropriate use of antibiotics could cause resistance.
Better knowledge about antibiotics is expected to improve practice towards antibiotic use as it helps people to better understand the role of antibiotics and the negative effects of its misuse. To change behavior, people need to know the consequences of their behavior. Lack of public knowledge about antibiotics may cause a high number of self-medicating people.5 The results of this study has proven a significant association between the level of knowledge and selfmedication with antibiotics. Respondents with poorer knowledge have higher probabilities to self-medicate with antibiotics, and vice versa. Therefore, to prevent self-medication with antibiotics and change this unhealthy habit, it is necessary to develop multifaceted educational programs to improve public knowledge about antibiotics and to raise public awareness of antibiotic resistance.
“Antibiotics: Handle with Care” was a campaign launched by WHO on the first World Antibiotic Awareness Week in 2015. The theme of the campaign reflects the overarching message to the community that antibiotics are a precious resource and should be preserved. They should be used to treat bacterial infections, only when prescribed by a certified health professional. Antibiotics should never be shared or saved for the future. Furthermore, health professionals also have a role in preventing and controlling the spread of antibiotic resistance, such as by ensuring prudent use of antibiotics as well as educating patients about antibiotic resistance, the dangers of its misuse, and the importance of preventing infections.12
As shown by Table 4, although not significantly associated, self-medication practices were more prevalent in those whose family income were less than Rp 2.500.000 (OR=1.94; 95% CI=0.89–4.20). Although inability to pay for health service may be an underlying factor, it may not be the only cause. It was shown from the data that 45.8% of respondents who covered by health insurance turned out to purchase antibiotics without a prescription. This indicates that apart from financial barriers, self-medication may also be caused by other factors, such as poor quality care, poor access to public health services, and misconception about the use of antibiotics.8–10
Self-medication practices are also made possible by the easy access to buy antibiotics without a prescription. Although in Indonesia antibiotics are classified as prescription only medicines and, therefore, cannot be sold as over the counter (OTC) drugs, in this study, more than half of respondents (52.2%) bought antibiotics without a prescription at pharmacies. Many other respondents (43.9%) could even get antibiotics without a prescription from stalls (small shops or “warung”). These disturbing situations have also happened elsewhere in Indonesia. In Yogyakarta and Surabaya, 63.4% and 90.0% of respondents, respectively, could easily buy antibiotics from pharmacies without prescriptions.3,10
The ease of obtaining antibiotics at pharmacies without a prescription, consumers’ demands, and weak government control over the sale of antibiotics have opened people’s access to antibiotics so freely that it has been a commonplace to find them in stalls along with snacks and beverages. The government needs to tighten supervision over antibiotic sale and selling antibiotics without prescriptions must be strictly prohibited. Furthermore, to prevent and control the spread of antibiotic resistance, policymakers must strengthen policies, programs, and the implementation of infection prevention and control measures. Appropriate use of antibiotics must also be well regulated and promoted.
We understand that recall bias was inevitable and might affect the result of this study. We have tried to minimize this bias by using a shorter time limit, which was 6 months, to define self-medication, while other studies commonly used 1 year interval. Another limitation would be measurement bias since the questionnaire used in this study might not be completely accurate in measuring the level of knowledge about antibiotics. Moreover, the language used to form the questions might not have been fully understood by respondents and led to inaccurate answers. To prevent this from happening, we had pretested the questionnaire and chose the questionnaire-structured interview over the self-answered questionnare technique so that we could directly see the respondents in person and make sure if they understood the questions.
In conclusion, there are associations between self-medication with antibiotics and age, family income, and the level of knowledge. Poorer knowledge about antibiotics may increase the probability to self-medicate with antibiotics, and vice versa. Thus, a better understanding of antibiotics and antibiotic resistance is required. Physicians, especially those working in primary care, have an important role to improve people’s awareness of antibiotic resistance and to promote prudent use of antibiotics.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
The authors would like to thank Oktavin Y Umboh, MD as the chief of Teling Atas Community Health Center; Anton Rumambi, MD; Debby Mintjelungan, MD; Andrea Putra Ramoh, MD; Ira Posangi, MD; Ricci Steven, MD; Guadelupe Maria Melisa, MD; Lisawati Sutrisno, MD; Gratia Kawatu, MD; Daniela Angeline, MD; and all staff of Teling Atas Community Health Center for their supports to this study. We also thank all of our respondents for their cooperation in this study.
REFERENCES
- World Health Organization. Antimicrobial resistance: global report on surveillance. Geneva, Switzerland: World Health Organization; 2014. p. 232.
- Setiati S, Alwi I, Sudoyo AW, Simadibrata M, Setiyohadi B, Syam AF, editors. Buku Ajar Ilmu Penyakit Dalam. 6th ed. Jakarta: Interna Publishing; 2014. P. 700–710.
- Puspitasari HP, Faturrohmah A, Hermansyah A. Do Indonesian community pharmacy workers respond to antibiotics requests appropriately? Trop Med Int Health. 2011;16(7):840–6.
- Lim KK, Teh CC. A cross sectional study of public knowledge and attitude towards antibiotics in Putrajaya, Malaysia. South Med Rev. 2012;5(2):26–33.
- Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS One. 2015;10(2):e0117910.
- Kim SS, Moon S, Kim EJ. Public knowledge and attitudes regarding antibiotic use in South Korea. J Korean Acad Nurs. 2011;41(6):742-9.
- Duerink DO, Lestari ES, Hadi U, Nagelkerke NJ, Severin JA, Verbrugh HA, et al. Determinants of carriage of resistant Escherichia coli in the Indonesian population inside and outside hospitals. J Antimicrob Chemother. 2007;60(2):377–84.
- Belkina T, Al Warafi A, Hussein Eltom E, Tadjieva N, Kubena A, Vicek J. Antibiotic use and knowledge in the community of Yemen, Saudi Arabia, and Uzbekistan. J Infect Dev Ctries. 2014;8(4):424–9.
- Ramay BM, Lambour P, Cerón A. Comparing antibiotic self-medication in two socio-economic groups in Guatemala City: a descriptive cross-sectional study. BMC Pharmacol Toxicol. 2015;16:11.
- Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Res Notes. 2011;4:491.
- Hadi U, Duerink DO, Lestari ES, Nagelkerke NJ, Werter S, Keuter M, et al. Survey of antibiotic use of individuals visiting public healthcare facilities in Indonesia. Int J Infect Dis. 2008;12(6):622–9.
- www.who.int [Internet]. Antibiotic resistance. [update 10/16; cited 2016 Dec 2016]. Available from: http:// www.who.int/mediacentre/factsheets/antibioticresistance/ en/
- Muras M, Krajewski J, Nocun M, Godycki-Cwirko M. A survey of patient behaviours and beliefs regarding antibiotic self-medication for respiratory tract infections in Poland. Arch Med Sci. 2013;9(5):854–7.
- Widayati A, Suryawati S, de Crespigny C, Hiller JE. Knowledge and beliefs about antibiotics among people in Yogyakarta City Indonesia: a cross sectional population-based survey. Antimicrob Resist Infect Control. 2012;1(1):38.15.
- Ling Oh A, Hassali MA, Al-Haddad MS, Syed Sulaiman SA, Shafie AA, Awaisu A. Public knowledge and attitudes towards antibiotic usage: a cross-sectional study among the general public in the state of Penang, Malaysia. J Infect Dev Ctries. 2011;5(5):338–47.
- Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Selfmedication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries. 2009;3(7):491–7.
- Skliros E, Merkouris P, Papazafiropoulou A, Gikas A, Matzouranis G, Papafragos C, et al. Self-medication with antibiotics in rural population in Greece: a crosssectional multicenter study. BMC Fam Pract. 2010;11:58.
- Ecker L, Ochoa TJ, Vargas M, Del Valle LJ, Ruiz J. Factors Affecting caregivers’ use of antibiotics available without a prescription in Peru. Pediatrics. 2013;131(6):e1771–9.
- Yu M, Zhao G, Stålsby Lundborg C, Zhu Y, Zhao Q, Xu B. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: a crosssectional study. BMC Infect Dis. 2014;14:112.
- André M, Vernby A, Berg J, Lundborg CS. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother. 2010;65(6):1292–6.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id