
Section Abstract Introduction Methods Results Discussion Conflict Of Interest Acknowledgment References
Clinical Research
Association between varicocele grade and semen analysis parameter
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v26i4.1623 Med J Indones. 2017;26:270–6
Received: October 25, 2017
Accepted: December 29, 2017
Author affiliation:
1 Department of Radiology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
2 Department of Urology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
3 Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
4 Department of Community Medicine, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
Corresponding author:
Rahmad Mulyadi
E-mail: dr_rahmad_radiologi@yahoo.com
Background
Varicocele is a condition characterized by elongation, dilatation and tortuousity of spermatic vein in pampiniform plexus. Approximately 50% of infertility cases among men are caused by varicocele. The varicocele may affect the components of sperm. This study aimed to determine the association between varicocele grade based on ultrasound Doppler examination and sperm concentration, sperm motility, and sperm morphology based on semen analysis examination.
Methods
This was a descriptive, cross-sectional study which used secondary data from 85 patients that visited Department of Urology, Cipto Mangunkusumo Hospital, then underwent ultrasonography examination at Department of Radiology, Cipto Mangunkusumo Hospital and semen analysis examination at Department of Obstetrics and Gynecology, Cipto Mangunkusumo General Hospital.
Results
Varicocele grade was significantly associated with sperm morphology, concentration and motility (all p<0.05). Significant association was found between maximum condition and semen analysis component.
Conclusion
Varicocele grade may affect semen analysis component.
Keywords
semen analysis, ultrasound examination, varicocele’s grade
Varicocele is a condition characterized by elongation, dilatation and tortuosity of spermatic vein in pampiniform plexus. The incidence of varicoceles in the general population varies from 4.4–22.6%, whereas in men with primary and secondary infertility, the incidence is 21– 41% and 75–81%, respectively.1 It is the most frequent abnormal physical finding among men who undergo infertility evaluation.2 Varicocele can influence all of semen parameters such as sperm concentration, sperm motility and sperm morphology.1–3
Al Ali et al found decreased quality of semen as well as higher level of testosterone in patient with varicocele grade III. Similarly, Mori et al also reported varicocele grade II and grade III caused decrease in sperm quality and testes volume. However, there were no significant differences between both grades. The study also mentioned that Grade III varicocele adolescents were much closer to the World Health Organization (WHO) sperm motility cut off value of which is established in 1999. Despite of that, sperm quality deterioration in varicocele is progressive and expected to cross into the WHO-defined infertile range much sooner.2,4
Approximately 83% of varicocele patients were under 50 years of age, and about 75% of patients reported infertility as the chief complaint and uncomfortable sensation at scrotum as additional symptom.5 The study also found that all of the patients had varicocele in the left side and 62.5% of patients presented oligozoospermia. There was no linear association between varicocele grades and sperm concentration, whereas testes atrophy had direct correlation with varicocele grades. In additional, 38.5% of varicocele patients had one child or more, but 61.5% of patients had no child.2,4,5
Up to nowadays, studies regarding association between varicocele grade and disturbance of semen analysis component are still scarce, especially in Indonesia. Referring to the latest WHO sperm analysis guideline established in 2010, it is confirmed that sperm analysis cut off has been updated. Therefore, this study may provide new paradigm and different analysis. This study aimed to determine the association of varicocele grade with sperm concentration, motility and morphology.
METHODS
This was a cross-sectional study conducted at Cipto Mangunkusumo Hospital between May 2013 to February 2014 with ethical approval number 584/H2.F1/ETIK/2013. Medical records of patients aged above 16 years old who were clinically diagnosed as varicocele during October 2013 to January 2014 were evaluated. The inclusion criteria included patients who were diagnosed with varicocele by physical examination who had undergone testis ultrasonography examination as well as semen analysis. Patient who had undergone varicocelectomy, abnormal follicle-stimulation hormone (FSH) level (FSH serum level out of 1–14 IU/L), small testes volume (testes volume below 13.9–18.9 ml3 with difference between left and right testes more than 20% according to ultrasonography examination), and the long interval duration between ultrasonography (USG) and semen analysis (more than 1 month) were excluded.
In this study, varicocele was graded using USbased criteria as follows: grade 0, if the diameter of pampiniform plexus is less than 2 mm during Valsalva and non Valsalva maneuver; grade I, if the diameter of pampiniform plexus is less tahn 2 mm during non-valsalva, but 2–3 mm during valsalva maneuver; grade II, if the diameter of pompiniform plexus is 2–3 mm during both condition; and grade III, if the diameter is more than 3 mm during the Valsalva and non-valsalva meneuver.6
The analysis of sperm quality using three components: sperm concentration, motility, and morphology. Sperm concentration is reported as azoospermia, oligozoospermia, and normozoospermia. Sperm motility is sorted as azoospermia, asthenospermia, and normozoospermia. Sperm morphology is sorted as azoospermia, teratozoospermia, and normozoospermia. According to WHO laboratory manual for sperm examination (2010), the terms mentioned before are defined based on criteria as follow: azoospermia is a condition of absence of sperm in the semen. Oligozoospermia is a condition of sperm concentration less than 15 million per ml semen. Asthenozoospermia is a condition of progressively motile sperm less than 50% of total sperm. Teratozoospermia is a condition of sperm with normal morphology less than 30% of total sperm. Normozoospermia is a condition of sperm with concentration above 39 million per ml semen, progressively motile sperm is more than 50% of total sperm, and morphologically normal sperm is above 30% of total sperm.7
Varicocele grade data measurement was analyzed according to diameter of the right testis group and left testis group. But, varicocele grade may vary between left and right testis. This condition may affect result of overall analysis. So, it is necessary to add maximum condition group which is drawn from either left or right pampiniform plexus with highest number in diameter in each individual.
The numerical data were presented as means ± standard deviation. McNemar’s test was used for comparison of the scored quality of the examination. All statistical analyses were performed using statistical product and service solutions (SPSS) 11.5 for Windows.
RESULTS
A total of 85 patients were recruited in this study. The mean age of the subjects was 35±6.27 years old. The subjects mostly came from Jakarta-Bogor- Depok-Tangerang-Bekasi (83.5%). Maximum condition was taken from the highest grade between right and left varicoceles. About 67.1% of patients presented normal morphology, and 61.2% of the subjects were oligospermic. According to sperm motility, 51.8% of patients were found asthenozoospermia (Table 1).
Table 1. Subject characteristic and data distribution
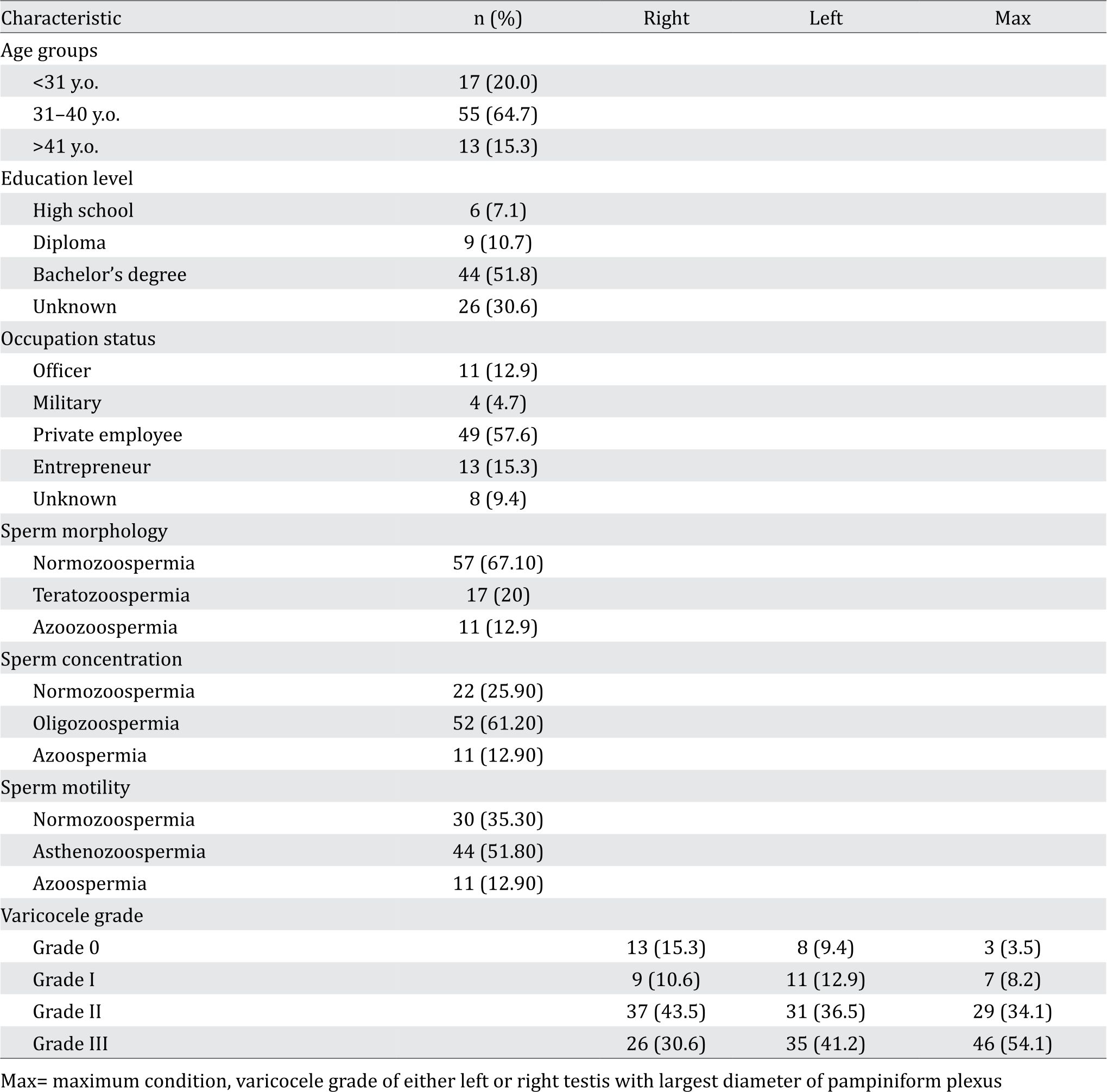
On statistical analysis, we divided varicocele grade into three groups. There were grade 0 (Figure 1. A-D), grade I (Figure 1. E-H) – grade II (Figure 2. A-D), and grade III (Figure 2. E-F). Dilatation of right, left, and maximum pampiriform plexus with sperm morphology gave p<0.001 (Table 2). Dilatation of right pampiriform with sperm concentration gave p=0.011, dilatation of left and maximum pampiriform p=0.000 (Table 3). Concerning dilatation of right pampiriform and sperm motility we obtained p=0.001, dilatation of left and maximum pampiriform p<0.001 (Table 4). We found significant association between the grade of right varicocele and morphology (p<0.05). The significant association was also found in the grade of left varicocele and the maximum condition (p<0.05).
Table 2. Grading varicocele and sperm morphology. All parameters were not statistically significant p>0.005
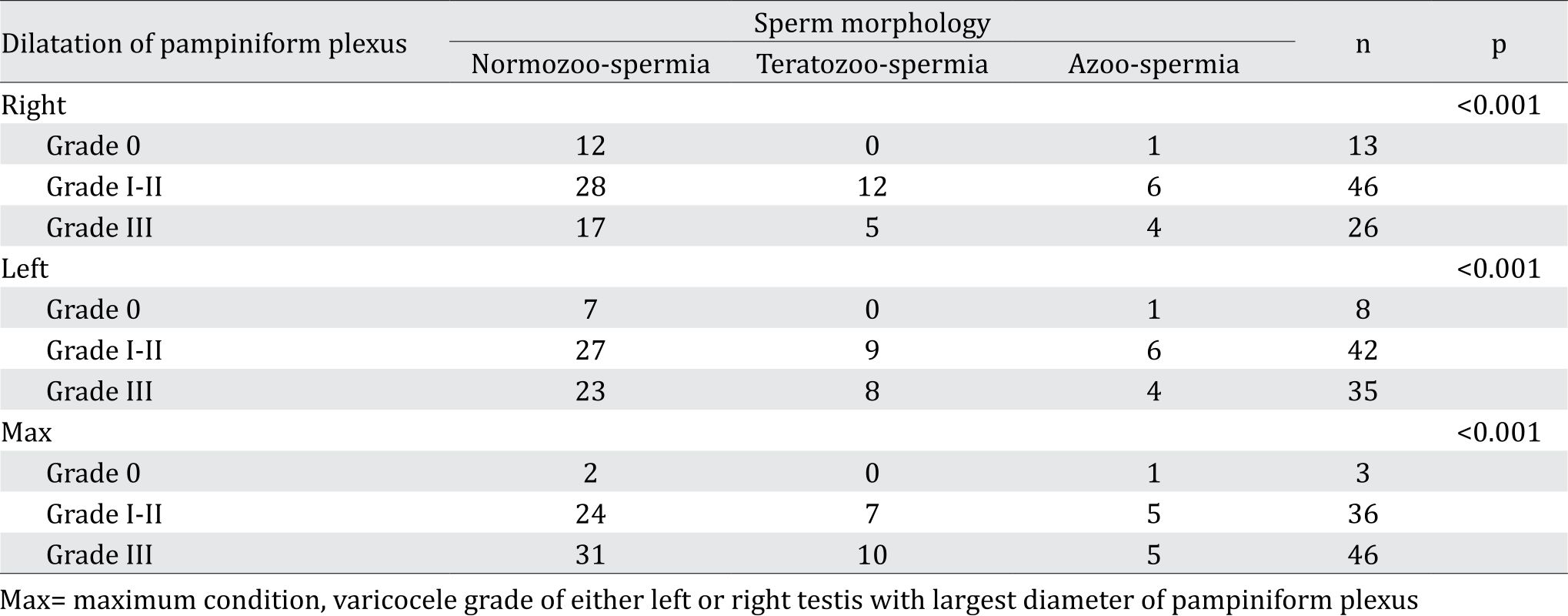
Table 3. Grading varicocele and concentration
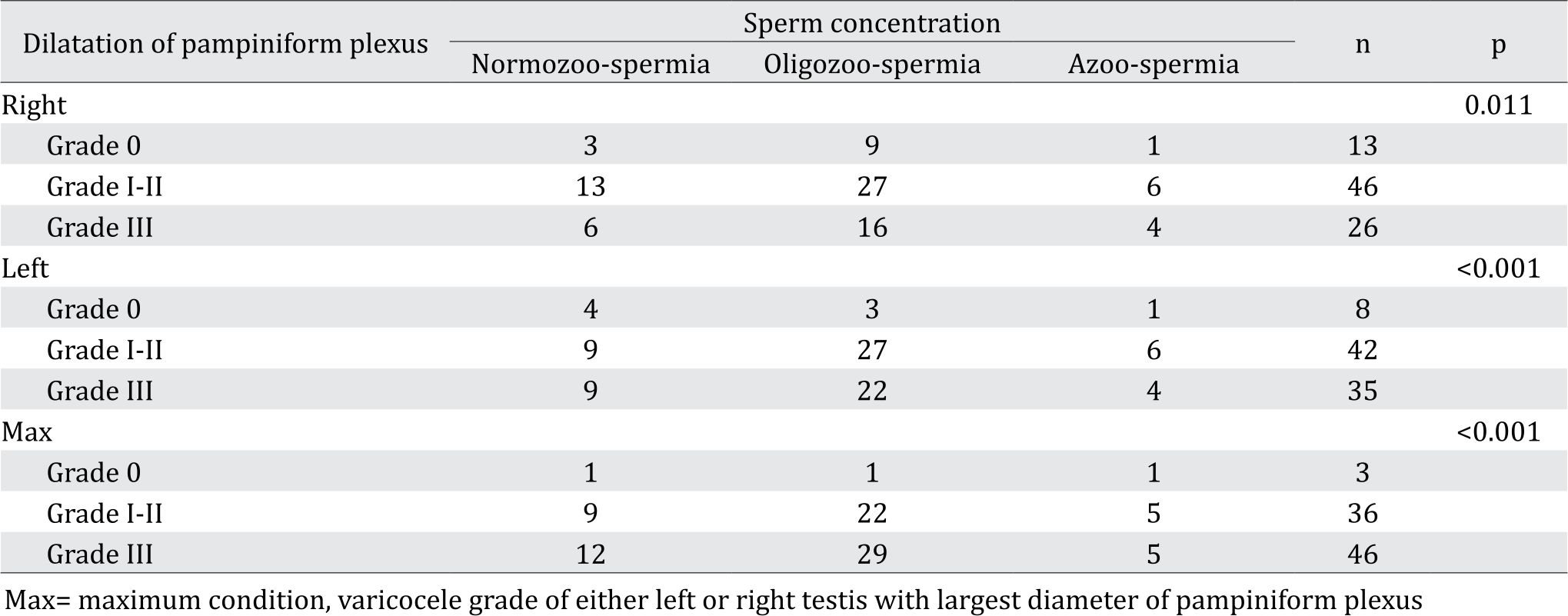
Table 4. Grading varicocele and motility
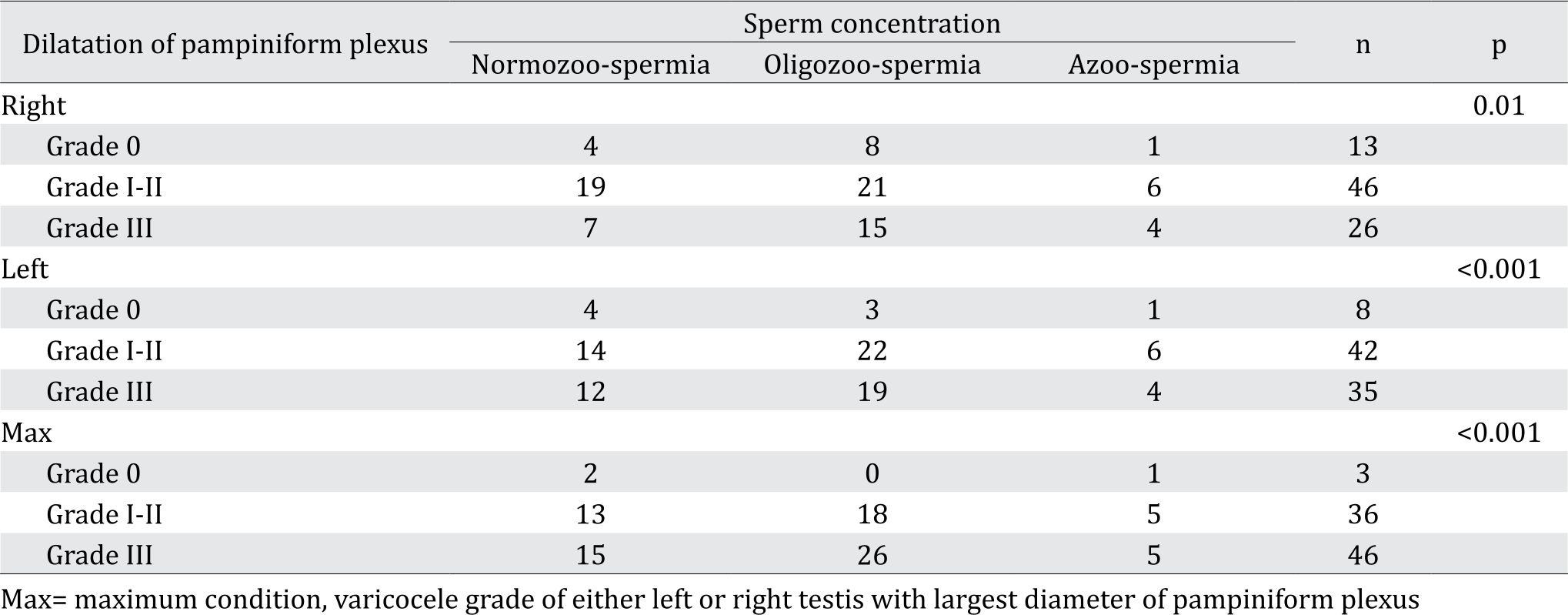
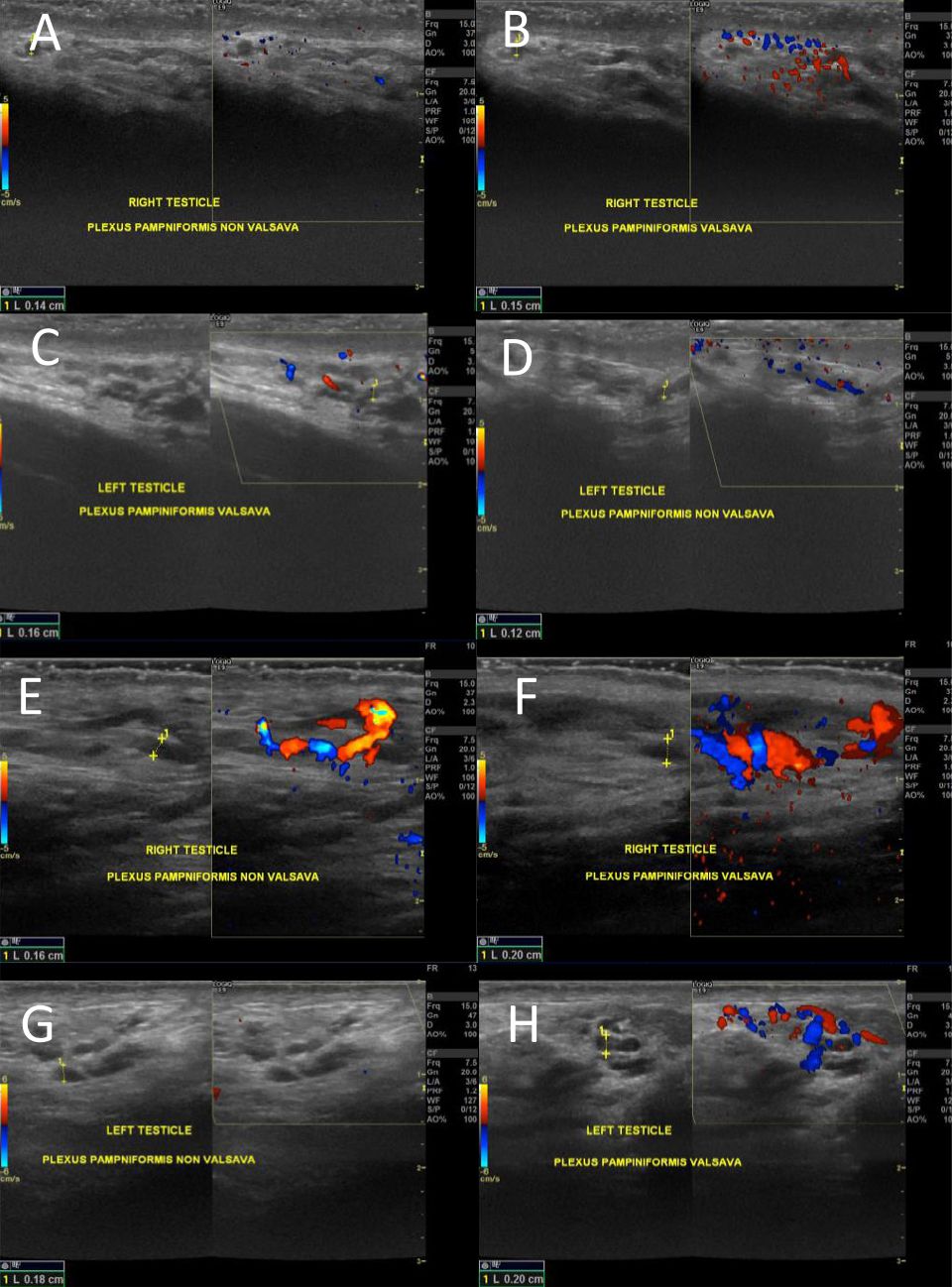
Figure 1. Doppler ultrasound of grade 0 varicocele. A is the right testicle and C is the left testicle. Both showing plexus pampiniform diameter below 2 mm in relaxed supine position. B and D showing both left and right pampiniform plexus increased in diameter below 2 mm. Doppler ultrasound of grade I varicocele. E is the right testicle and G is the left testicle. Both showing plexus pampiniform diameter below 2 mm in relaxed supine position. Both right (F) and left (H) pampiniform plexus diameter increased between 2–3 mm during Valsava maneuver
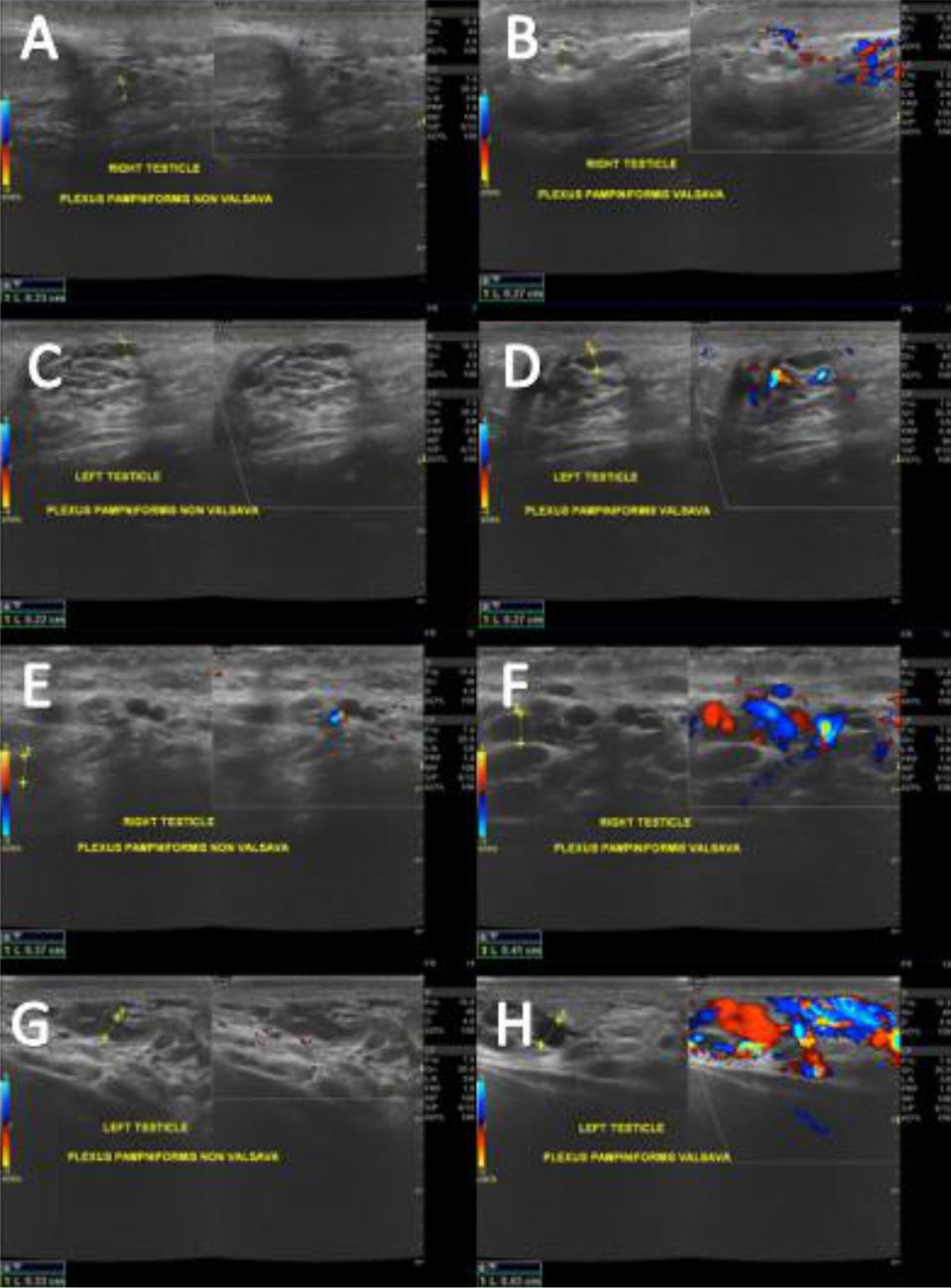
Figure 2. Doppler ultrasound of grade II varicocele. A) is the right testicle and C) is the left testicle. Both showing plexus pampiniform diameter at less than 3 mm in relaxed supine position. Both right (B) and left (D) pampiniform plexus diameter increased at the range of 2-3 mm during Valsava maneuver. Doppler ultrasound of grade III varicocele. E) is the right testicle and G) is the left testicle. Both showing plexus pampiniform diameter more than 3 mm in relaxed supine position. Both right F) and left H) pampiniform plexus diameter increased higher than 3 mm during Valsava maneuver
DISCUSSION
Varicocele is a condition of spermatic vein dilatation in the pampiniform plexus. It is reported that varicocele is associated with infertility.1 Approximately 8% of men in the reproductive age have infertility problems8 and 35% of them are caused by varicocele.4 The previous study found that patient with varicocele did not have Sertoli cell. the Sertoli cell, which function to stimulate follicle stimulating hormone (FSH) and responsible for spermatogenesis.8,9
The number of patients with left-sided varicocele is more than the population with right-sided varicocele. This is consistent with the other studies that showed that majority of primary varicoceles were present on the left side. Hasan et al10 reported that 86.3% of varicoceles were on the left side, whereas Abbas et al11 revealed that 82% of varicoceles were mainly left-sided. Other studies1,12 suggested that 78–93% of primary varicoceles were left-sided. The main cause is the anatomical location of left spermatic vein which is more vertical than the right side entering renal vein. Moreover, there is “nutcracker” phenomenon that happened due to compression of the left renal vein, which was located between abdominal aorta and superior mesenterica artery.
The term varicocele grade 0 in this study was defined when the diameter of pampiniform plexus on the Valsalva and non-Valsalva maneuver was less than 2 mm. It’s been determined that there was no dilatation of pampiniform plexus. This definition was supported by Pilatz et al6 who reported that varicocele was the dilatation of pampiniform plexus about 2.45 mm in the relax position (sensitivity 84%; specificity 81%) and about 2.95 mm on the maneuver (sensitivity 84%; specificity 84%) using Doppler ultrasonography.
According to the results of the semen analysis, the majority of sperm morphology was good. However, the sperm concentration and motility were mostly poor. This study is consistent with the semen parameters were influenced by biological, physical, occupational, and environment factor two months before semen analysis examination. Patients was instructed to abstinent for sexually intercourse during 2 until 7 days. Duration of abstinence would influence volume and sperm concentration, but not with sperm motility.8 The multiple semen analysis disturbance would increase infertility risk. Defect in the sperm morphology was the most crucial factor in the semen analysis, but the result should be interpreted in context of their clinical condition.8
This study suggested that varicocele grade is strongly associated with sperm morphology, concentration, and sperm motility. It is caused by increased hidrostatic pressure inside scrotum due to dilatation of pampiniform plexus. This condition increases the temperature, and if the temperature rises, the volume and quality of sperm will be reduced. The lower quality of sperm will impact in the fertilization then. Nevertheless, reference limits provided by WHO manual are derived from semen samples used to initiate natural conception but not the nature of the treatment. Therefore, according to Esteve et al8 it should be considered to perform additional test, such as genetic evaluation, radiology evaluation, and antibody evaluation.
Patients selected based on inclusion and exclusion criteria. However, there might be several factors that influence the results of this study, such as the past-medical history (cryptorchidism history, herniation, testis trauma, mumps, diabetes mellitus, chirrosis, hypertension, sexually transmitted diseases, tuberculosis and viral infection), surgical history (orchidopexy, herniorraphy, orchiectomy, and surgical at the organ around pelvis), history of gonadotoxic exposure, family history of fibrotic cyst, metabolic endocrine disease and infertility history in family, infertility history (contraception method, pregnancy, and age of wife), and sexual history (frequency of coitus, lubricant used, and libido). Furthermore, larger numbers of the patients is still needed for the better study.1,4,8
In conclusion, varicocele grade may affect semen analysis component. A precise medical history, physical examination, and complementary test are the key to establish early diagnosis of varicocele and to determine best strategies to treat infertility.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Will MA, Swain J, Fode M, Sonksen J, Chistman GM, Ohl D. The great debate: Varicocele treatment and impact on fertility. Fertil Steril. 2011;95(3):841–52.
- Al-Ali BM, Marszalek M, Syamloul R, Pummer K, Trummer H. Clinical parameters and semen analysis in 716 Austrian patients with varicocele. Urology. 2010;75(5):1069–73.
- Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM. Does Varicocele Repair Improve Male Infertility? An Evidence-Based Perspective From a Randomized, Controlled Trial. Eur Urol. 2011;59:455–61.
- Mori MM, Bertolla RP, Fraietta R, Ortiz V, Cedenho AP. Does varicocele grade determine extent of alteration to spermatogenesis in adolescents. Fertil Steril. 2008;90(5):1769–73.
- Yasumoto R, Kobayakawa H, Kawamura M, Iwai S, Yuuki K, Ohyama T, et al. Clinical studies of varicocele report 1: Clinical statistical analysis of varicocele. Kurenai. 1988;34:309–11.
- Pilatz A, Altinkilic B, Kohler E, Marconi M, Weidner W. Color doppler ultrasound imaging in varicoceles is the venous diameter sufficient for predicting clinical and subclinical varicocele. World J Urol. 2011;29(5):645–50.
- WHO Laboratory Manual for the Examination and Processing of Human Semen. Fifth edition. 2010.
- Esteves SC, Miyaoka R, Agarwal A. An update on the clinical assessment of the infertile male. Clinics (Sao Paulo). 2011;66(4):691–700.
- Roth M, Amory J, Page ST. Treatment of male infertility secondary to morbid obesity. Nat Clin Pract Endocrinol Metab. 2008;4(7):415–9.
- Hasan R, Dian A, Hanif M, Yusuf A, Hassan H. Comparison of the efficacy of laparoscopic versus open high ligation of varicoceles. Ann Pak Inst Med Sci. 2013;9(2):68–73.
- Abbas MW, Kamal M, Murtaza G. Varicocele; comparison of complications in open surgery versus laparoscopic surgical management of varicocele among adolescents at a tertiary care hospital. Professional Med J. 2017;24(8):1099–104.
- Kantartzi PD, Goulis ChD, Goulis GD, Papadimas I. Male infertility and varicocele myths and reality. Hippokratia. 2007;11(3):99–104.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id