
Section Abstract Introduction Methods Results Discussion Conflict Of Interest Acknowledgment References
Clinical Research
The influence of water intake on waiting time prior to uroflowmetry: a prospective, randomized, double-blind trial
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v26i3.1628 Med J Indones. 2017;26:212–7
Received: October 27, 2016
Accepted: June 21, 2017
Author affiliation:
Department of Urology, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Corresponding author:
Ponco Birowo
E-mail: ponco.birowo@gmail.com
Background
In uroflowmetry examination, patients are usually instructed to intake a large volume of water and wait until the bladder is full. The association between the volume of water intake and the waiting time before uroflowmetry is unknown. The aim of this study is to investigate the relationship between the volume of water intake and the waiting time prior to uroflowmetry.
Methods
This trial was designed as a randomized, researchers, caregivers and patients blinded, superiority trial with three parallel groups and primary endpoint of waiting time prior to the uroflowmetry study based on the volume of patients’ water intake. Randomization was performed by block randomization with a 1:1:1 allocation. Patients scheduled for uroflowmetry at the Urology Clinic of Cipto Mangunkusumo Hospital were enrolled from March 2013 until December 2013. The eligibility criteria were male patients with ages above 50 years and body mass index 18.5–24.9 kg/m2.
Results
A total of 83 patients was randomly assigned into 3 study groups: 300 ml (28 patients), 400 ml (28 patients), and 500 ml (27 patients). All patients were included in final analysis. Mean waiting time were 85.1±59.8 min, 107.2±70.4 min, and 66±28.4 min for patients intake 300, 400, and 500 ml of water respectively (p=0.07). The final bladder volumes for three groups were statistically different (262.4±130.8 ml, 289.4±126.2 ml, 359.2±137 ml; p=0.02).
Conclusion
The volume water intake of 300–500 ml did not affect waiting time before uroflowmetry. Increasing water intake at least 500 ml added the final bladder volume and shorter the waiting time.
Keywords
drinking, urinary bladder, uroflowmetry, waiting time
Lower urinary tract symptoms (LUTS) is a collection of complaints consist of three groups: storage, voiding, and post micturition symptoms.1 The prevalence of LUTS in elderly male population is approximately 20–30%, and nocturia is common in 30 to 59-year-old men.2,3 In 2008, 45.2% of world population experienced one symptom of LUTS. It is expected that the prevalence will rise to 63.6% in 2018.4
Therefore, before the uroflowmetry study, patients should fill their bladder. The influence of water intake on waiting time before uroflowmetry study is unknown. There are no consensus guidelines on safe preparation or imaging modalities for pre-procedural fluid hydration.9 Patients are usually asked to drink plenty of water to achieve a full bladder and wait until they have a desire to urinate.7 The disadvantage of this method is some patients feel uncomfortable with a full bladder, and some other patients have their bladder not fully filled for uroflowmetry study. By knowing the amount of fluid intake, it will reduce excessive fluid intake and facilitate hospital to calculate unit cost of uroflowmetry. Another advantage of knowing time required before uroflowmetry study is that patients, doctors, and nurses can predict how long patients should come, so that patients and doctors do not have to wait too long. In this study, we investigated the influence of water intake on waiting time prior to uroflowmetry.
METHODS
This trial was designed as a randomized, researchers, caregivers and patients blinded, superiority trial with three parallel groups and primary endpoint of waiting time prior to the uroflowmetry study based on the volume of patients’ water intake. Randomization was performed by block randomization with a 1:1:1 allocation. The trial was completed, and there was not any change in protocol design. The trial received ethical committee, and informed consent was obtained from each patient (47/H2.F1/ ETIK/2013). The trial was conducted at the Urology Clinic of Cipto Mangunkusumo Hospital, Jakarta, from March 2013 until December 2013.
The eligibility criteria were male patients who will have uroflowmetry examination with ages above 50 years and body mass index (BMI) 18.5– 24.9 kg/m2. The exclusion criteria were subjects have history of hematuria, urinary tract infection, renal insufficiency or urinary tract anomaly, hypertension, coronary heartt disease or congestive heart failure, diabetes mellitus, shock, residual urine ≥50 ml, history of operation or pelvic radiation, suprapubic mass, consumption of diuretic or anticholinergic.
The patients were asked to fill informed consent and personal data including age, occupation, education, blood pressure, height, and weight. History and physical examination were taken in relation to research status of patients. The blood level of urea, creatinine, glucose, and urinalysis were also determined. The patients were asked to measure bladder volume and urinate, and then the examiner checked the residual urine.
Patients who have met the inclusion criteria were mL randomly divided into three groups. The first group was given water about 300 ml (group A), the second group was given water about 400 mL (group B), and the third group was given water about 500 ml (group C). For the allocation of participants, a block randomization by a computer-generated list of random number was used by researchers with no clinical involvement in the trial. After the nurse had obtained patient’s consent, she contacted a staff member who was independent during the recruitment process for allocation consignment. The allocation sequence was concealed from researchers, caregivers, and patients. Each patients was given a sealed-bottle, and description amount of water given was contained in a sealed envelope. All sealed-bottles have same dimension, color, and appearance. The period of drinking was ten minutes. The patients did not allow drink or urinate until they felt first sensation of micturition. The staff member noted time and bladder volume when the subject wanted to urinate for the first time at the same day with randomization. Bladder volume was assessed by ultrasonography. The staff member who obtained outcome measurement was not informed of the group assignment. The staff who delivered the intervention did not take the outcome measurements.
The primary outcome was the relationship between the volume of water intake and the waiting time before uroflowmetry study. The secondary outcome was the relationship between the volume of water intake and the total bladder volume before uroflowmetry.
Water intake is defined by volume of water which was given by researchers to be taken by patients. The volume of water intake has been determined to 300 ml, 400 ml, and 500 ml. Waiting time is defined by the time from ingestion of water until first sensation of micturition. The time is noted in minutes.
The minimum total samples needed to have 80% power to detect a significant difference (p=0.05, two-sided) were 27 for each group. The mean and standard deviation of quantitative Figure 1. The CONSORT 2010 flow diagram about the influence of water intake on waiting time before uroflowmetry procedure. The process consists of four phases: enrollment, allocation, follow-up, and analysis data were calculated and compared using oneway analysis of variance, statistical product and service solutions (SPSS) version 15.0. P<0.05 was considered statistically significant.
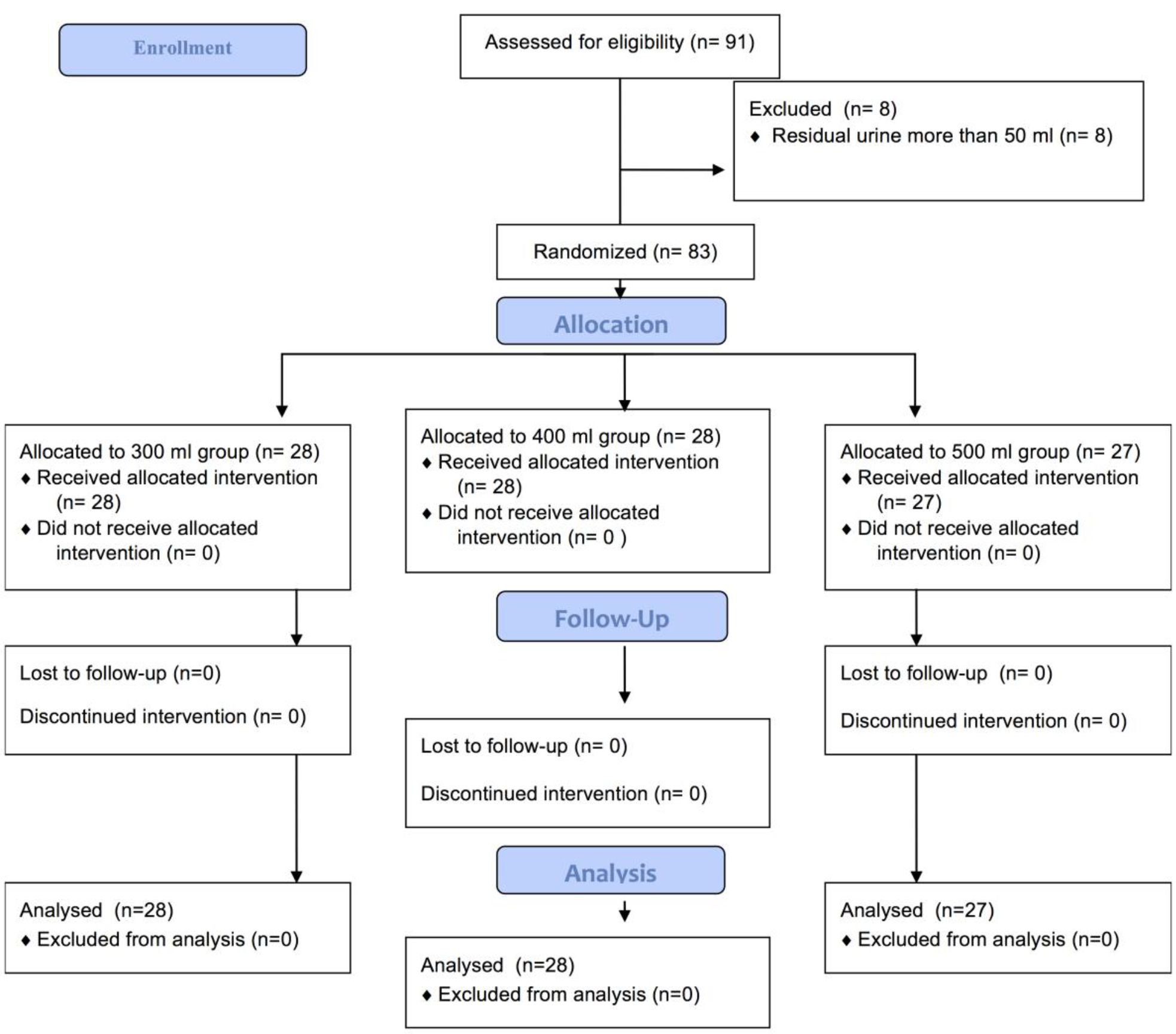
Figure 1. The CONSORT 2010 flow diagram about the influence of water intake on waiting time before uroflowmetry procedure. The process consists of four phases: enrollment, allocation, follow-up, and analysis
RESULTS
There were 91 patients who were eligible for the study. However, eight patients were excluded due to residual urine more than 50 ml. A total 83 patients were randomly assigned to 3 study groups: 300 ml (28 patients), 400 ml (28 patients), and 500 ml (27 patients). Flow diagram of the progress through the phases of a parallel randomized trial of three groups is shown in Figure 1.
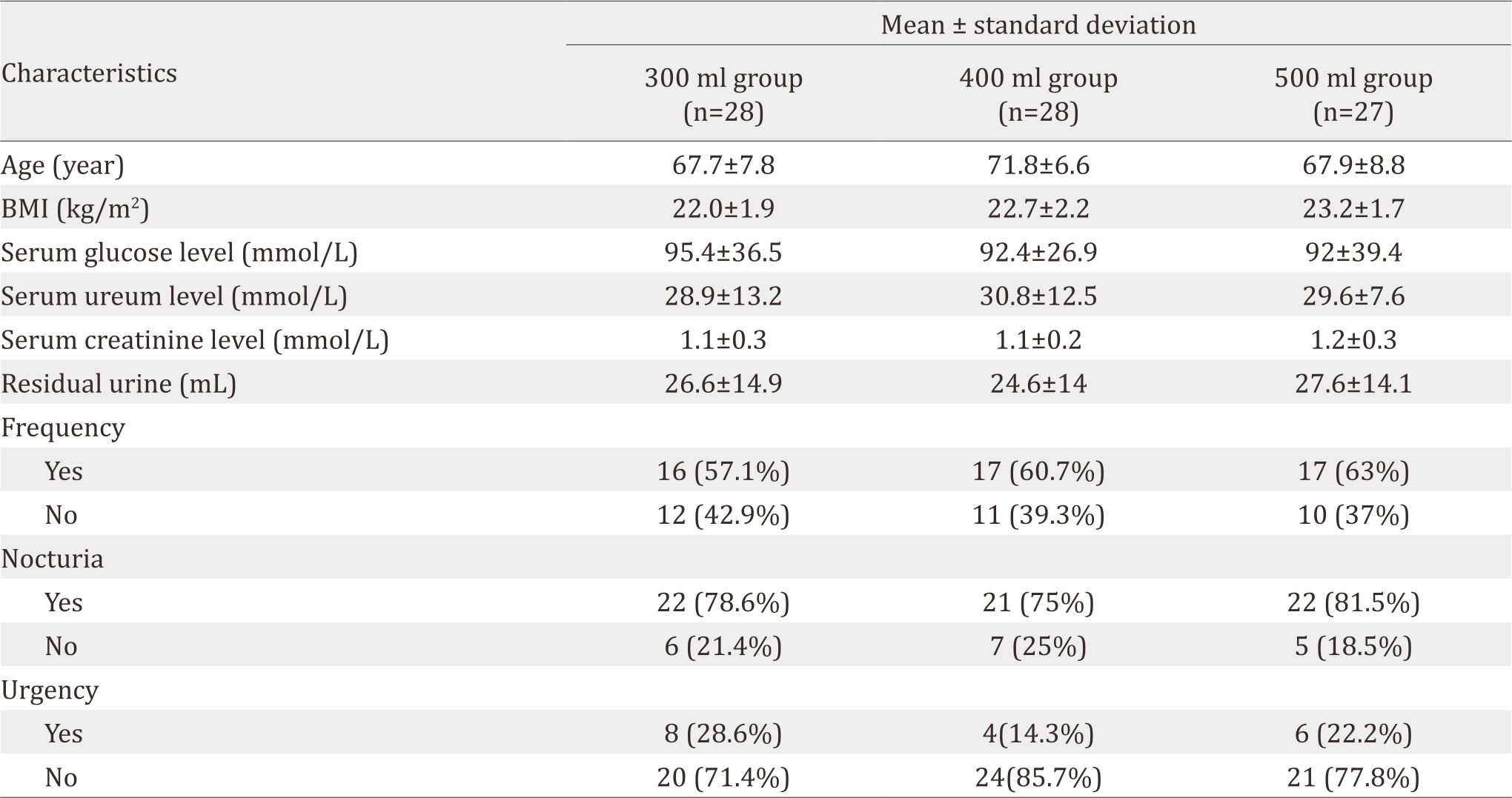
The demographic and clinical characteristics of subjects in three groups are shown in Table 1. There were not any patients complain in relation to bladder discomfort during the trial.
Table 1. Demographic and clinical characteristics of patients in each study group
The average waiting time and the total bladder volume between groups are described in Figure 2. There were no statistically significant differences in waiting time between three groups (p=0.07). The average waiting time was comparable for 300 and 400 ml groups; however the 500 ml group had the least waiting time and variation. The total bladder volumes among the 3 study groups were higher in the 500 ml group among them all. The final bladder volumes for three groups were statistically different (p=0.02).
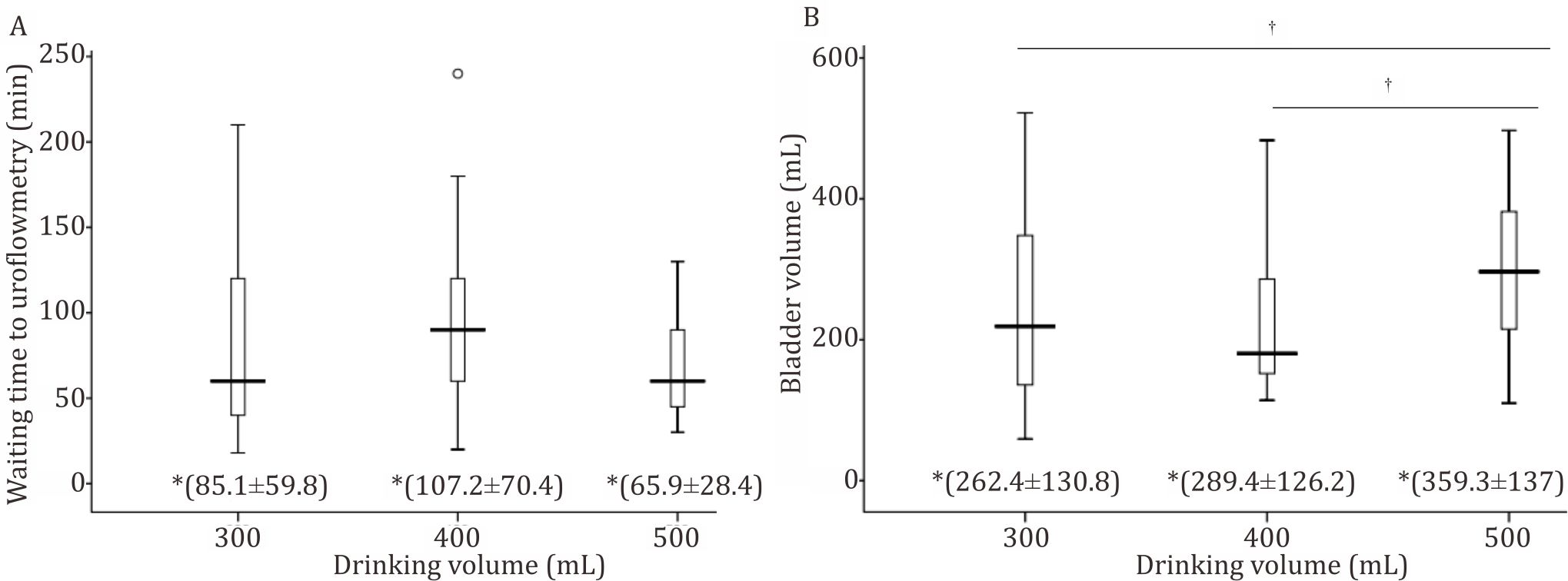
Figure 2. Average waiting time (A) and total bladder volume before uroflowmetry (B). Analysis used One Way Anova with post -hoc Bonferroni. *mean±SD; †p<0.05
DISCUSSION
Uroflowmetry is the preferred examination tools for patient with LUTS complain. This examination required voiding volume between 150 ml and 400 ml to achieve optimal result. An increase in volume water ingested increased the urine output, and we hypothesized that increasing the volume of water ingested would reduce the time needed to fill the bladder sufficiently prior to uroflowmetry.6–8
This study is the first study that investigated relationship between the water intake and the waiting time prior to uroflowmetry. The result of this study indicated that waiting time before uroflowmetry study reduced as the volume of water intake increased (300, 400, and 500 ml). However, this relationship was not significant (p=0.07). The possibility of this finding could be due to the small sample size or the insufficient volume of water intake to reduce waiting time. Jordan et al10 concluded that there was not any change in plasma renin and vasopressin after drinking 500 ml of water. Thus, the waiting time might be reduced if water intake was more than 500 ml. No previous study recommended the volume of water intake for patients undergoing urine flow studies. The lack of consensus guidelines on pre-study fluid consumption could lead to adverse event due to excessive water intake. Some reports have been published about water intoxication before flow study caused severe hyponatremia and seizure.9,11,12 In this study, water intake of 300–500 ml was safe and did not cause any complains from patients. We suggest patients should take more than 500 ml of water prior to uroflowmetry.
A study about the influence of water intake on waiting time prior gynecologic abdominal ultrasound concluded that differences in the volume of water intake (range 300–500 ml) did not affect waiting time before transabdominal ultrasound examination. The possible reason is the inadequate sample size. Another possibility is the volume of water ingested was not sufficient enough to reduce waiting time.13 The previous study is in accordance with our study. We used the same volume of water (range 300–500 ml) and did not find significant differences in waiting time. As suggested by previous study, larger sample size may be needed.
This study also showed that increasing water intake significantly added total bladder volume. The minimum water intake of 300 ml was sufficient to fill bladder of 262.4±130.8 ml. This volume of water might be enough to consume before uroflowmetry. The accuracy of residual urine measurement in men cannot be accurate as catheterization. Ultrasonography is poor for quantitative assessment of bladder volumes, particularly with volume below 48 ml. It is reported that inaccuracies from methods used in ultrasonography varied from 12.9% to 20% in adults.14 This study used ultrasonography to assess the residual urine before water intake and final bladder volume after water intake. This study used residual urine above 50 ml to exclude patients from randomization. Therefore, we can minimize the chance of ultrasonography inaccuracy in assessing the bladder.
The measurement of post-micturition residual urine that recorded before water load is different from that of recorded after increased water load diuresis. The residual urine volume after increased water load diuresis is larger than after normal bladder filling and voiding at first desire.15 In this study, we measured the bladder volume and asked the patients to urinate first. After that, the post micturition residual urine was remeasured. Thus, we can measure post-void residual urine volume that reflected everyday normal bladder filling.
This study has several limitations. There were some variables that could lead to bias including hydration status, previous activities of subject, and unpredicted blood loss. We cannot measure these factors to be considered as eligibility criteria. In history taking, we asked the patients whether they have history of hematuria, including education and occupation. We also checked urinalysis to confirm whether there was hematuria and assessed specific gravity to grossly determine hydration status of patients. The history of underlying disease could affect waiting time prior to uroflowmetry. Patients who have dominant storage complaints will have shorter waiting time. In addition to that, the intervention was implemented for male patients with LUTS, age >50 years old, and normal BMI, the results indicate that all male patients with that characteristic would not benefit from water intake 300–500 ml on waiting time before uroflowmetry study. Further studies by using larger sample sizes, more homogenous baseline characteristics, larger volume intake, and more accurate measurements methods are needed to confirm our findings. However, the characteristic patients included in this study covered most of patients who need uroflowmetry study in clinical setting. This suggests that this study result can be implemented in preparation of patients before uroflowmetry.
In conclusion, drinking volume of water of 300 to 500 ml is safe for patients who undergo uroflowmetry, and patients should drink at least 500 ml of water to increase bladder volume and reduce waiting time.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):167–78.
- Spigt M, Schayck OV, Knipschild P, Westerterp K, Beek CVD, Kerrebroeck PV, et al. Is it possible to improve elderly male bladder function by having them drink more water? A randomized trial of effects of increased fluid intake/urine output on male lower urinary tract function. Urology. 2006;68(5):1031–6.
- Platz EA, Smit E, Curhan GC, Nyberg LM, Giovannucci E. Prevalence of and racial/ethnic variation in lower urinary tract symptoms and noncancer prostate surgery in U.S. men. Urology. 2002;59:877–83.
- Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int. 2011;108(7):1132–8.
- Kelly CE, Krane RJ. Current concepts and controversies in urodynamics. Curr Urol Rep. 2000;1:217–26.
- Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol. Urodinam. 2002;21(3):261–74.
- Abrams P. Uroflowmetry. In: Abrams P. Urodynamics Third Edition. London: Springer; 2006. p. 20–38.
- Blaivas J, Chancellor MB, Weiss J, Verhaaren M. Uroflowmetry. In: Blaivas J, Chancellor MB, Weiss J, Verhaaren M. Atlas of Urodynamics Second Edition. New York: Blackwell Publishing; 2007. p. 37–45.
- Su M, Woo HH. Severe hyponatremia from water intoxication associated with preparation for a urine flow study. J Med Cases. 2012;3(2):123–5.
- Jordan J, Shannon JR, Black BK, Ali Y, Farley M, Costa F, et al. The pressor response to water drinking in human asympathetic reflex? Circulation. 2000;101(5):504–9.
- Issa MM, Pruthi RS, Vial C, McNamara DE, Terris MK. An unusual complication following uroflowmetry: water intoxication resulting in hyponatremia and seizure. Urol Int. 1997;59:129–30.
- Vishwajeet S, Aneesh S. Water intoxication leading to hyponatremia and seizures: a rare complication of uroflowmetry. Int Urol Nephrol. 2005;37:275–6.
- Titapant V, Phithakwatchara N, Chuenwattana P, Tontisirin P, Viboonchard S, Butsansee W. Influence of water intake on the waiting time prior to gynecologic transabdominal ultrasound. Int J Gynecol Obstet. 2009;105(3):233–5.
- Simfroosh N, Dadkhah F, Hosseini SY, Asgari MA, Nasseri A, Safarinejad MR. Accuracy of residual urine measurement in men: comparison between real time ultrasonography and catheterization. J Urol. 1997;158:59–61.
- Alivizatos G, Skolarikos A, Albanis S, Ferakis N, Mitropoulos D. Unreliable residual volume measurement after increased water load diuresis. Int J Urol. 2004;11:1078–81.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id