Based on the 8th Indonesian Renal Registry, the number of end-stage renal cases (ESRD) in Indonesia has been increasing annually. In 2015, there were 21,050 new cases of renal dysfunction of which 89% were categorized as end-stage renal disease (ESRD).1 Furthermore, a surge in non-communicable diseases, such as diabetes and hypertension, caused a rapid increase of ESRD incidence.2 The presence of this disease could trigger many issues, especially in socioeconomy aspect. The majority of ESRD cases opted for hemodialysis as their treatment. In the past, the cost of hemodialysis was cheaper than kidney transplantation. In the early years of kidney transplant in Indonesia, one complete procedure cost approximately US$ 15,000, but as years passed, this trend changed.3 The overall cumulative cost of kidney transplant becomes lower than that of hemodialysis.3 The high incidence and long-term treatment of hemodialysis for ERSD patients contribute to the national health burden. Furthermore, Heathcare and Social Security Agency (Badan Penyelenggara Jaminan Sosial Kesehatan/BPJS Kesehatan) reported that the cost of renal disease treatment is the second highest health expenses.4 To cover the cost of two times a week of dialysis, it needs 500 healthy insured people. To further explain about the cost of hemodialysis in Indonesia, data from 2006 showed that the cost of hemodialysis varies from US$ 4,900 to US$ 6,500 depending on the facility.5 This is considered expensive considering the average Indonesian earns US$ 1280 per year (one year’s dialysis is equal to 5 years of the average Indonesian wage), thus it needs an alternative option to overcome this condition. Two other alternatives that are considered as renal replacement therapy are continuous ambulatory peritoneal dialysis (CAPD) and kidney transplantation. CAPD is considered as an alternative as it provides many advantages compared to hemodialysis, such as liberal dietary intake of protein, potassium, sodium, and fluids, elimination of need for anticoagulation, increased patient mobility and lower costs, but it has high incidence complications like peritonitis, catheter malfunction up to 70%, and high hematocrit levels in many patients.6 On the other hand, according to emerging evidences, kidney transplantation is considered as the most desired and cost-effective modality for patients with ESRD.7 According to the National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQI), early kidney transplant in ESRD patient has the best result on costs and medical outcomes.7 Laupacis et al8 also showed that kidney transplantation had better advantages compared to hemodialysis in terms of cost and survival rate.
The first recorded clinical kidney transplantation was conducted on March 13th, 1902 by Erich Ullmann in ‘Wiener klinische Wochenschrist’. He performed kidney transplantation to a dog by transplanting one of the dog’s kidney on another dog’s neck vessel. The first renal transplantation from human to human was successfully conducted in 1933 by Yuri Voronoy in Ukraine,9 using 6 hours anoxic cadaver kidneys to be re-implanted into medial thigh of a 26-year-old woman with acute mercury intoxication, but the result was poor due to ABO incompatibility and hyperacute rejection. Afterwards, the discovery of immunosuppressive medication and the better understanding regarding cross matching between recipient and donor greatly increased the survival of kidney transplantation in humans. Until December 23rd, 1954, Dr. John Murray, who eventually won the Nobel Prize in Medicine for his achievement, performed the first successful kidney transplant in Brigham and Women’s Hospital Boston to a 23-year-old patient with ESRD. The donor was his identical twin brother.8,10 As it progressed, more minimal invasive procedures were found, such as laparascopic donor nephrectomy, laparoscopic kidney transplantation, and robotic kidney transplantation. The introduction of these techniques increased the number of transplantation conducted around the world.11 In Indonesia, BPJS Kesehatan recently endorsed kidney transplantation as an alternative treatment option for ESRD patients.
This review identifies the milestones in the development of kidney transplantation in Indonesia and elucidate factors that affect its growth. This identification may be used to further strengthen and develop Indonesia’s kidney transplantation program. Therefore, we divide the era of kidney transplantation into several periods.
The birth of a new ESRD treatment (1977–1980)
The first kidney transplantation procedure in Indonesia was conducted on November 11th, 1977 in Cipto Mangunkusumo Hospital and supervised by a Japanese urologist named Professor Ota from Tokyo Women Medical College. This was the beginning of a historical hallmark in Indonesia. In 1977, renal transplantations were mainly conducted in two hospitals, Cipto Mangunkusumo Hospital (RSCM) and PGI Cikini Hospital, with the number of transplantations was still less than 5 per year. The number of surgeons who was capable to do kidney transplantation surgery was less than 10 surgeons.12 In order to boost up the number of surgeons capable to perform kidney transplantation surgery, these experts continued to share their knowledge to other colleagues, especially outside of Jakarta. As a result of these events, later in 1985, Kariadi Hospital and Telogorejo Hospital Semarang successfully conducted several transplantation surgeries. Thus, after this breakthrough, the number of kidney transplantation was increasing every year although it was still less than 20 per year.
At this period, the organ donor shortage, the expensive cost, and the public opinion still emerged as the main barriers.13 Furthermore, consensus regarding kidney transplantations in the main religions has not established yet.
Expectant growth (1981–1984)
In 1981, the government issued new laws regarding surgery in deceased bodies and transplantation of human tissues (Peraturan Pemerintah/ Government Regulation No. 18/1981). It was the first national law that became the basis of kidney transplantation law in Indonesia.14 This law was supported by an International Consensus made by the Transplantation Society which has been updated from time to time. This law and consensus provided the first guideline for the distribution and the use of organs from cadavers and living unrelated donors. Thus, it encouraged the increase of kidney transplantation numbers in this era.
The first downfall (1984–1987)
In this period, the first major downfall in numbers of kidney transplantation occured. This was seen as an expected downfall, considering that in these years, kidney transplantation was still a relatively new procedure, and economically, Indonesia was still unstable.12,15 Several factors were believed to contribute for the declining of kidney transplant. The first issue was that in the 1983, the value of Rupiah begin to drop, from Rp. 702 to Rp. 970 per 1 US$, (a devaluation up to 38%). At first, this issues didn’t have any impact on the number of kidney transplant. In 1985-1986, Indonesian Government devaluated the value of Rupiah even further, from Rp.1,134 to Rp. 1,664 per 1 US$, a devaluation of 47%. In 1986, Indonesia was affected by the global economic crisis due to the drop in global oil prices (on January 1986, the price of oil per barrel was 25 US$, but six months later dropped to 10 US$ per barrel), which affected Indonesia’s revenue.15 This economic problem was believed to have a correlation with the number of transplantation in Indonesia (especially at 1985–1986). As the economy condition in Indonesia crumbled, people could not afford kidney transplant surgery.
The stable period (1988–1995)
In this period, centers for kidney transplantation grew in several cities, including Bandung, Semarang, Yogyakarta, Surabaya, and Medan. The number of kidney transplantation doubled compared to the previous period. However, the growth in the number of cases of kidney transplantation was relatively slow.
Various regulations encouraged the economic growth and promoted the growth of health programs. The examples of these programs were an earlier form of national health insurance and well-balanced distribution of health services around Indonesia through primary health care centers. Organ transplantation law was also renewed in the form of Undang Undang No 23 Tahun 1992 (Law No. 23/1992).16 This law stated that organ transplantation could only be conducted for humanitarian purposes, and any commercializations of organ transplantation were prohibited. Moreover, in 1995, a consensus was made between religious leaders and health experts including nephrologists and urologists. It was named Kesepakatan Kemayoran (Kemayoran Agreement).17This consensus, that were formulated at the 2nd PERNEFRI (Perhimpunan Nefrologi Indonesia/ Indonesian Society of Nephrology) and YAGINA (Yayasan Ginjal Nasional/National Kidney Foundation) symposium, concluded that kidney transplantation was one the best treatments for ESRD and stated that the use of cadaveric donor was permitted from the perspective of religion (all five official religions in Indonesia), perspective of health experts, and culture aspects.
The unstable period (1996–2005)
The year 1996–1999 was the peak of global economy crisis which increased health cost and led millions of people into poverty in Indonesia. As a result, many Indonesians were unable to afford health care facilities including kidney transplantation. Furthermore, the government mainly focused to provide primary health care and used most of its resources for this sector. As a result, the budget allocated for kidney transplantation was small because chronic kidney disease (CKD) was not categorized as a main health care problem. Kidney transplantation also was not the primary treatment for ESRD patients during this time. However, there were many Indonesian ESRD patients who went abroad for kidney transplantation.18 Other aspects that were suspected to have an effect in declining the number of kidney transplantations in Indonesia (especially in 2004–2005), were the changes in the political climate in Indonesia, the 2004 Election. This year’s election was the hallmark of Indonesian democracy and reformation. Therefore, many policies in Indonesia (including health policy) were changed, such as the implementation of keluarga miskin policy (GAKIN)/Policy for Poor Families, and also these changes affected the economic stability in Indonesia back then.15 Also in this period, one of the worst natural tragedies in Indonesia, the Aceh tsunami unfolded, further affected the economic stability in Indonesia. Figure 1 shows that the unstable number of kidney transplants mainly happens in PGI Cikini Hospital. In 2004, Markum17 tried to deduce several factors that affected the number of organ transplant donor. These factors were the availability of living donors, the reluctance of using cadaveric organ donors, the donor availability problem, and the pre- and post-operative cost. Moreover, the issue of organ donor compensation was still an ethical dilemma between medical practitioners. The demand for transplantable organs became a burden not only in Indonesia, but also in most of ASEAN countries.19 Singapore, Malaysia, and the Philippines encountered shortage of organ donor. Each country tried to resolve this issue through various methods. Singapore gave birth to the “Human Organ Transplant Act” which allowed medical staff to give compensation to the donor in the form of medical saving accounts. Malaysia and the Philippines expanded the living-related donor definition by including emotional related relationship. A close friend or marital partner could be included as the source of organ donor. Furthermore, to overcome this problem, ASEAN countries tried to adapt the Scandinavian transplant program. This program allowed Scandinavian countries to work together to fill the demand organ transplant by exchanging their donor pool.
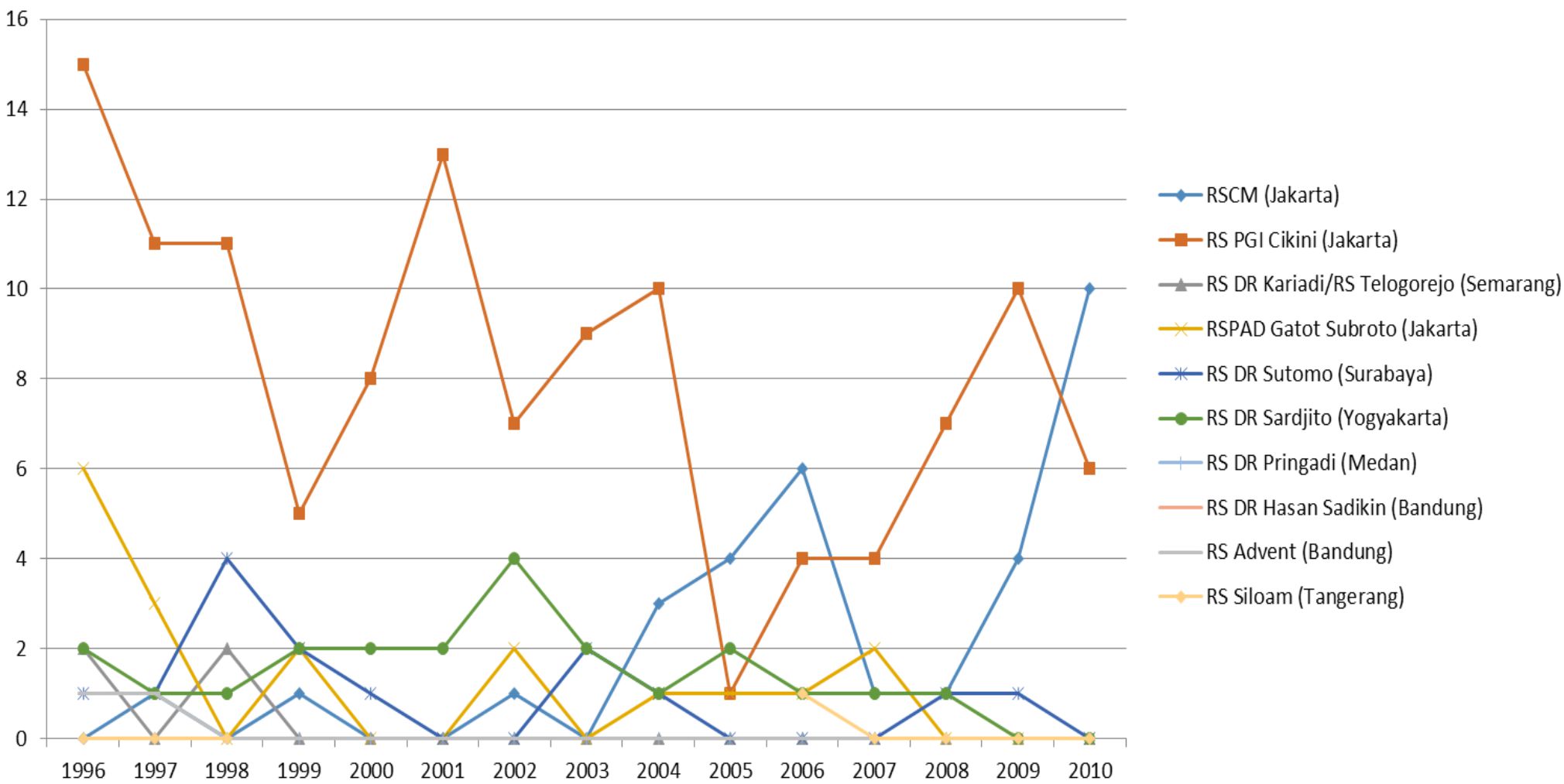
Figure 1. The unstable and rebirth of kidney transplant era. This figure shows that the unstable condition mainly happens in PGI Cikini Hospital, and the rebirth mainly happens in Cipto Mangunkusumo Hospital, and it keeps on going until present time
The rebirth of kidney transplantation in indonesia (2006–2010)
In the early 2000s, increasing demands of kidney transplantation were not balanced by the number of organ donors.17 As a result of this problem, illegal donor retrieval, such as organ trafficking, began to arise.20, 21
During 2006, there was global concern regarding organ donor commercialization in several countries. Organ trafficking was on the rise worldwide with numerous unfortunate stories of brokers, physicians, and hospitals engaged in illegal trade were featured in high-profile media.20 The example of this problem was the case of Falun Gong Followers’ organ harvesting in China, which Amnesty International reportedly said that 99% of organs in China came from executed prisoners.20 Other reported case is India’s black market organ scandal that was based in Gurgaon, a business center close to the capital New Delhi.21 This black market organ transplant ring had been harvesting poor Indian laborers, sometimes against their wishes, then sold to foreigners desperate for transplants. Doctors usually paid as little as $ 1,000 for kidneys and sold them as much as $ 37,500. As the consequences, World Health Organization (WHO) conducted an international investigation regarding organ donor, and the World Health Assembly issued a resolution for all WHO member states to prohibit transplant tourism.20 This ultimately ended up with organ transplantation tourism being banned around the world, as stated in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism.20,22,23 This condition reduced the number of countries that provided organ donor for transplantation tourism and forced end-stage renal disease patients to look for available donors in their own countries. This issue caused the demand of domestic renal transplantation increased in Indonesia and in many other countries. The rapid growth of information technology bridged the supply and demand of organ transplantation, and after a short slump, it helped in increasing the number of kidney transplantations in Indonesia.
In 2008, the Indonesian Health Ministry passed a new regulation regarding inform consent. This law mandated hospitals to obtain inform consent to conduct any medical procedures. The aim of this regulation was to protect health care personnel from any lawsuit. Following this regulation, the government issued a new law related with organ transplantation (UU No.36 Tahun 2009).24 It specifically regulated the use of transplantation as the option for end-stage disease patients. This regulation allowed organ transplantation only for medical purposes and without any commercial motivation. Moreover, government health insurance was improved in 2005 when a new regulation (UU No. 40 Tahun 2004 about National Social Security System)25 was created. These changes were made to ensure that poor people will get sufficient health care services.
All of these regulations and laws affected the number of kidney transplantation in Indonesia. Figure 2 shows that the number of kidney transplantation started to increase progressively in these years, especially in Cipto Mangunkusumo Hospital. It indicates that the rebirth mainly happened in Cipto Mangunkusumo Hospital although the number of transplants were still relatively low compared to the present time. In 2005–2010, kidney transplant was still considered as special surgery, which was still conducted only on Saturday (especially in our Cipto Mangunkusumo Hospital), required expensive logistics, and there were no clear standard operating procedure (SOP) back then. Following this trend, several hospitals, Dr. Saiful Anwar Hospital Malang, Dr. Moewardi Hospital Solo, and Dr. M. Djamil hospital Padang also successfully conducted their first kidney transplantation. These marked the distribution of transplantation skills and knowledge among medical services in Indonesia.
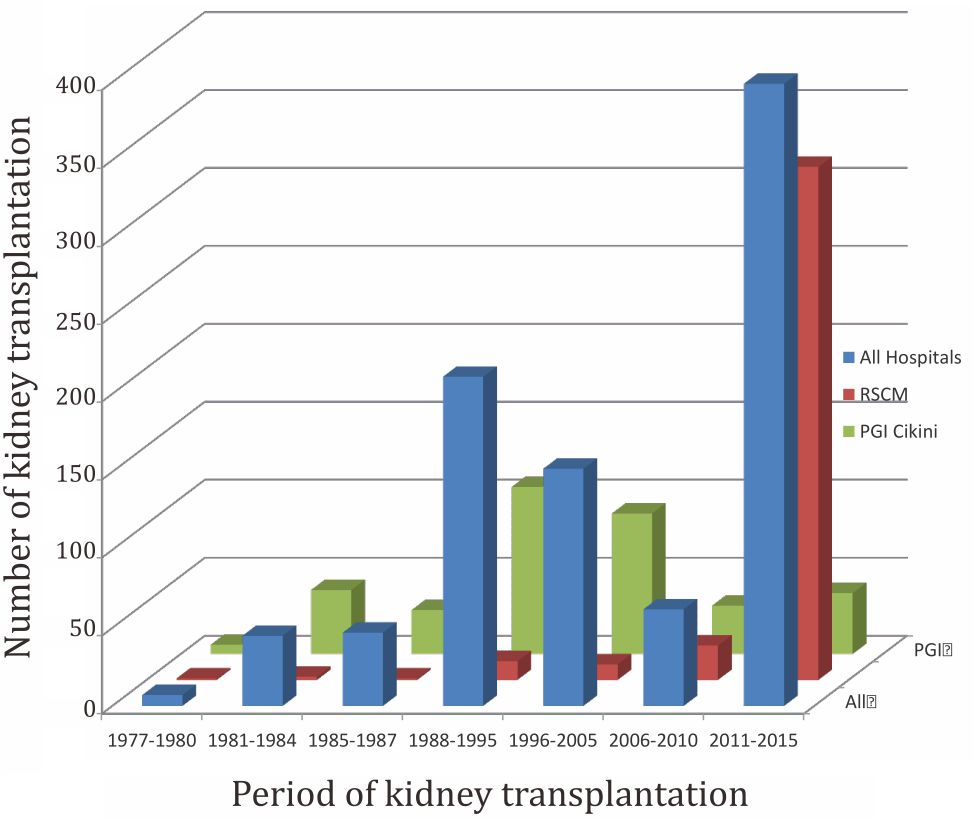
Figure 2. The growth of kidney transplantation. This figure explains the number of kidney transplants in each designated era of kidney transplant in Indonesia
The explosive growth (2011–2015)
The year 2011–2012 was an important breakthrough of kidney transplant in Indonesia. The numbers of kidney transplantation in Cipto Mangunkusumo Hospital was rising high in this period (Figure 2). The important aspect in this period was the application of a minimal invasive technique, laparoscopic living donor nephrectomy (LLDN). In November 2011, the first LLDN was successfully conducted in Cipto Mangunkusumo Hospital, and this technique was widely introduced to the media in a Press Conference entitled “RSCM Mampu Melakukan Teknik Transplantasi Ginjal Berstandar Internasional di Gedung RSCM Kencana” that was held on Thursday, 12 January 2012. This technique has surely become one of the most important milestones in Indonesia. It can be observed that after this LLDN technique was introduced to the public through media, the number of kidney transplants were increasing dramatically. Meta-analysis study from 2008 by Nanidis et al26 concluded that LLDN has less postoperative pain, less post-operational morbidity, and most importantly shorter recovery time and shorter time to get back to work post operation.
Another milestone of kidney transplantation in Indonesia that happened in this period was the pediatric kidney transplantation. In March 2013, Cipto Mangunkusumo Hospital successfully conducted the first renal transplantation in a pediatric case. It was commonly known that the renal transplantation surgery in children was harder compared to adult patients. Various issues were needed to be considered when transplantation was conducted in children. The issues were the requirement of chronic immunosuppression, the immune responsiveness, the sexual and emotional transition, the dosage changes, and the risk of post-transplant viral infections and lymphoproliferative disorders (PTLDs).27 Until now, RSCM has performed 4 cases of pediatric kidney transplantations.
Drastic changes also happened in 2014, where in this year, the government through Ministry of Health appointed 11 government hospitals to do (or restart in several centers) kidney transplantation services. Following this appointment, Cipto Mangunkusumo Hospital established kidney transplantation specialized team consisted of urologist, nephrologist, cardiologist, pulmonologist, anesthesiologist, clinical pathologist clinical and anatomical pathologists, radiologist, pediatrician, forensics, and nutritionist. This team was created to manage the high number of organ transplantation demands and provide comprehensive service to patient with ESRD. Until now, RSCM has supervised a kidney transplantation program at other government hospitals in Aceh, Medan, Padang, Palembang, Solo, Malang and Denpasar. Furthermore, the Ministry of Health Republic of Indonesia has established a National Transplantation Committee as an oversight committee for hospitals that deliver kidney transplantation surgery/program (Peraturan Menteri Kesehatan Republik Indonesia Nomor 38 Tahun 2016).28 This regulation also states that the permitted donor is not only related donor, but also unrelated donor.
Other aspects that affected the number of transplantation were the revision of the reimbursement for kidney transplantation (Peraturan Menteri Kesehatan Republik Indonesia Nomor 52 Tahun 2016) by BPJS.29 This revision was made due to the high long term cost of hemodialysis. After the realization of this issue, BPJS endorsed kidney transplantation surgery and CAPD as the recommended treatment for ESRDs.
Further development in Indonesia’s kidney tranplantation (2016–later)
To further develop kidney transplantation, a national kidney transplantation program is needed. Irlianti et al5 described that transplant procurement management (TPM) can be used as one of the solutions. TPM is defined as a system that provides every service required for living or deceased donors and manages the procurement and distribution of available organs through available transplantation institutions. By using this type of management, the available donor will be prioritized to severely needing patients. Indonesia is behind in terms of organ donor management. Until now, there are no specific organizations that facilitate people who want to donor their organ or to help end-stage renal failure patients to find a suitable donor within Indonesia. The management of organ transplantation is conducted mainly by the hospitals that are performing kidney transplantations. As a comparison, the Philippines already established an independent organization called the National Kidney and Transplant Institute (NKTI) with its primary role to manage the national kidney donor-recipient program since 1981. This organization ensures the source of donor is legal and not based on commercial purposes. As a result, the number of deceased and living donor increased significantly in the Philippines and until February 2013, they have performed 5,000 kidney transplantations.30
Markum et al17 summarized that there are several strategies to overcome kidney transplantation stagnancy issues in Indonesia. First strategy is by modifying the donor criteria, such as enlarging the age range for donor or allowing donor with comorbidities (marginal or sub-optimal donor). However, long-term survival rate of this technique is still a controversy. Secondly, the government needs to create operational standards for laws that regulate the use of cadaveric donor for organ transplantation. This law will be used as the legal standing to use a dead body for source of organ donor. The permission to use cadaver as organ donor is still a cultural controversy Indonesia.3 A new law that was decreed in 2016 re-emphasized the use of cadaveric donors28 (Indonesia adopts the opt in concept of donation). To enhance the progress of kidney transplantation, the government has formed a National Transplant Committee (Komite Transplantasi Nasional)28 to oversight committee and to control the legal, ethical, clinical and cultural aspects of all segments of organ transplantation.
Further development strategy that could be used in Indonesia to increase the number of kidney transplantation surgery is the use of advanced technology, such as robotic-assisted surgery. Recent study showed the beneficial effects of robotic assisted kidney transplantation.31 As a further statement, the use of minimally invasive technique was proven adequate to increase the number of kidney transplantation, as seen in Cipto Mangunkusumo Hospital. After usage of LLDN, the number of kidney transplantation hugely increased.
Another development plan in Cipto Mangunkusumo Hospital is to establish the Uro- Nephrology and Kidney Transplantation Center. Developing this new center is in response to a tremendous growth in kidney transplantation. The presence of this center can further enhance the development of donation and recipient matching technique, establishment of a national kidney transplantation clinical pathway, and long-term follow up for the donor and recipient. Furthermore, this center will act as a kidney transplantation education and training center.
However, it must be remembered that the absence of an ethical transplant procurement management system is still hindering the progression of kidney transplantation in Indonesia, even in Asia
In conclusion, kidney transplantation program in Indonesia has re-gained popularity in recent years. Government support and health insurance coverage are examples of the reasons of this improvement. However, there is still a long process to increase the quantity and quality of kidney transplantation program, i.e. expanding kidney transplantation center, organ procurement program, improved donor and recipient cross-matching technology, development of minimal invasive technique in kidney transplantation surgery, improved immunosuppression, and increased pediatric kidney transplantation.
Conflicts of Interest
Agus Rizal A.H. Hamid is the editor-in-chief of this journal, but this article is also peer reviewed.
Acknowledgment
We would like to acknowledge PGI Cikini Hospital kidney transplantation staffs: dr. David Manuputty, SpB-SpU(K); dr. Tunggul D. Situmorang, SpPDKGH; dr. Sutjahjo Endardjo, SpPA, MSc; dr. Juniara Sidabutar, SpPD; Prof.dr. Wiguno Prodjosudjadi, PhD, SpPD-KGH; dr. Marihot Tambunan, SpPDKGH for helping the data collection.
REFERENCES
- Report of Indonesian Renal Registry. Indonesia: Perhimpunan Nefrologi Indonesia (PERNEFRI); 2015. 45 p. Report No.: 8. Indonesian.
- Ojo A. Addressing the global burden of chronic kidney disease through clinical and translational research. Trans Am Clin Climatol Assoc. 2014;125:229–46.
- Bennett PN, Hany A. Barriers to kidney transplants in Indonesia: a literature review. Int Nurs Rev. 2009 Mar; 6(1):41–9.
- Badan Penyelenggara Jaminan Sosial Kesehatan. Agar BPJS Kesehatan Tidak Layu Sebelum Berkembang [Internet]. Indonesia: INFOBPJS Kesehatan Edisi XVII; 2015 [cited 2016 October]; [about 3 screens]. Available from: https://bpjs-kesehatan.go.id/bpjs/dmdocuments/ e 6 e 2 6 8 a 2 1 3 6 8 f b 4 9 c a 2 1 b 2 c 4 2 1 1 a 6 9 0 e . p d f . Indonesian.
- Irlianti PI. Manajemen pengadaan organ untuk transplantasi. Fakultas Kedokteran Universitas Indonesia. 2014. Indonesian.
- Kavalakkat JP, Kumar S, Kekre NS. Continuous ambulatory peritoneal dialysis catheter placement: Is omentectomy necessary? Urol Ann. 2010;2(3):107–109.
- Abecassis M, Bartlett ST, Gaston RS. Kidney transplantation as primary therapy for end-stage renal disease: A National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQI) Conference. Clin J Am Soc Nephrol. 2008 Mar;3(2):4.
- Laupacis A, Keown P, Pus N, Krueger H, Ferguson B, Wong C, Muirhead N. A study of the quality of life and costutility of renal transplantation. Kidney International. 1996 Jun;50(1):235–42.
- Matevossian E, Kern H, Huser N, Doll D, Snopok Y, Nahrig J, et al. Historical Perspective surgeon yurii voronoy (1895-1961): a pioneer in the history of clinical transplantation: in memoram at the 75th anniversary of the first human kidney tranplantation. Transplant International. Dec 2009;22(12):1132–9.
- Sifferlin A. How the first successful kidney transplant happened [Internet]. New York: TIME; 2014 [cited 2017 April]. Available from: http://time.com/3644215/ history-kidney-transplant/
- Kuo PC, Johnson LB. Laparoscopic donor nephrectomy increases the supply of living donor kidneys: a centerspecific microeconomic analysis. Transplantation. May 2000;69(10):2211–3.
- Rahardjo D, Hardjowijoto S, Tigor A. Sejarah 40 tahun IAUI. Jakarta: Balai Penerbit IAUI; 2013.Indonesian.
- Indonesia Invesments [Internet]. Indonesia; 2015. Sejarah Indonesia: Politik dan Ekonomi di Bawah Soekarno; 2015 Jan 31 [cited Mar 2017]; [about 4 screens]. Available from: http://www.indonesia-investments.com/id/budaya/ kolom-budaya/sejarah-indonesia-politik-dan-ekonomidi- bawah-sukarno/item5271. Indonesian.
- Peraturan Pemerintah Nomor 18 Tahun 1981 tentang bedah mayat klinis dan bedah mayat anatomis serta transplantasi alat dan atau jaringan tubuh manusia. [cited: Mar 2017]. Available from: http://www.idionline. org/wp-content/uploads/2010/03/PP-No.-18-Tahun- 81-ttg-Bedah-Mayat-Klinis-Dan-Bedah-Mayat-Anatomis- Serta-Transplantasi-Alat-Dan-A.pdf. Indonesian.
- Sherlock S. Crisis in Indonesia: Economy, Society, and Politics [Internet]. Parliament of Australia [cited Apr 2017]. Available from: http://www.aph.gov.au/About_ Parliament/ Parliamentary_Departments/Parliamentary_ Library/Publications_Archive/CIB/CIB9798/98cib13
- Undang-Undang Nomor 23 Tahun 1992 Tentang Kesehatan. [cited: Mar 2017]. Available from: http:// www.hukumonline.com/pusatdata/detail/412/ node/20/undangundang-nomor-23-tahun-1992. Indonesian.
- Markum HMS. Renal transplantation problem in Indonesia. Acta Medica. Jul-Sep 2004; 36(3):184–6.
- Prodjosudjadi W. Incidence, prevalence, treatment, and cost of end-stage renal disease in Indonesia. Ethn Dis. 2006 Spring;16(2): S2–14–6.
- Jingwei AH, Yu-Hung AL, Ching L. Living Organ Transplantation Policy Transition in Asia: towards Adaptive Policy Changes. Global Health Governance. 2010;3(2):1–14.
- Jafar TH. Organ Trafficking: Global Solutions for a Global Problem. American Journal of Kidney Diseases. Dec 2009;54(6):1145–57.
- Robinson S. India’s black market organ scandal [Internet]. New York: TIME; Feb 1 2008 [cited 2017 April]. Available from: content.time.com/time/world/ article/ 0,8599,1709006,00.html
- Li J. Taiwan shuts down organ transplant tourism [Internet]. New York: The Epoch Times; Jun 21 2015 [Cited 2016 October 16]. Available from: http://www. theepochtimes.com/n3/1399326-taiwan-shuts-downorgan- transplant-tourism/
- Matas D. Organ sourcing in China: The official version [Internet]. New York: The Epoch Times; Apr 25 2015 [Cited 2016 October 19]. Available from: http://www. theepochtimes.com/n3/1332895-organ-sourcing-inchina- the-official-version/full/
- Undang-Undang Republik Indonesia Nomor 36 Tahun 2009 Tentang Kesehatan Available from: http://www. depkes.go.id/resources/download/general/ UU%20 Nomor%2036%20Tahun2%20009%20tentang%20 Kesehatan.pdf. Indonesian.
- Undang-Undang Republik Indonesia Nomor 40 Tahun 2004 Tentang Sistem Jaminan Sosial Nasional. Available from: http://www.jkn.kemkes.go.id/attachment/ unduhan/UU%20No.%2040%20Tahun%202004%20 tentang%20SJSN.pdf. Indonesian.
- . Nanidis TG. Laparoscopic Versus Open Live Donor Nephrectomy in Renal Transplantation: A Meta- Analysis. Ann Surg. 2008;247:58–70.
- Gulati A. Sarwal M.M. Pediatric renal transplantation: an overview and update. Curr Opin Pediatr. 2010 Apr; 22(2):189–96.
- Peraturan Menteri Kesehatan Republik Indonesia Nomor 38 Tahun 2016 Tentang Penyelenggaraan Transplantasi Organ. [cited: Mar 2017] Available from: http://hukor.depkes.go.id/uploads/produk_hukum/ PMK_No._38_ttg_Penyelenggaraan_Transplantasi_ Organ_.pdf. Indonesian.
- Peraturan Menteri Kesehatan Republik Indonesia Nomor 52 Tahun 2016 Tentang Standar Tarif Pelayanan Kesehatan Dalam Penyelenggaraan Program Jaminan Kesehatan. [Cited: Mar 2017] Available from: http:// djsn.go.id/storage/app/uploads/public/58d/487/ cdd/58d487cdd4630003169427.pdf. Indonesian.
- Parayno A.C. Kidney Transplantation in The Philipines: Celebrating more than 30 years of Best Practices [Lecture]. Lecture presented on 26 August 2016; Universitas Indonesia.
- Modi P, Pal B, Modi J, Kumar S, Sood A, Menon M. Robotic assisted kidney transplantation. Indian J Urol. 2014 Jul- Sep;30(3):287–92.
