
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Systematic Review
Does the establishment of universal health coverage drive the foundation of postgraduate education for primary care physicians?
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v26i2.1857 Med J Indones. 2017;26:141–51
Received: February 09, 2017
Accepted: May 31, 2017
Author affiliation:
1 Department of Community Medicine, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia
2 Department of Public Health, Faculty of Medicine Universitas Padjajaran, Bandung, Indonesia
3 Department of Family and Community Medicine, University of the Philippines, Manila, Philippines
Corresponding author:
Indah S. Widyahening
E-mail: indah_widyahening@ui.ac.id
Background
Studying the formation of postgraduate training in primary care within countries which has attained Universal Health Coverage (UHC) is important to support the development of similar training in low-and middle-income countries aiming to achieve UHC by 2030. This review aims to describe the state of postgraduate training for primary care physicians in UHC-attaining countries.
Methods
A literature review of published literature and official documents from the websites of regional and global health/primary care organizations or societies such as World Health Organization (WHO), World Organization of Family Doctors (WONCA), European Forum for Primary Care, European Union of General Practitioners (GP)/Family Physicians (FP), European Academy of Teachers in GP/ Family Medicine (FM), as well as the websites of GP/FP organizations in each of the respective countries. The list of UHC attained countries were identified through WHO and International Labor Organization databases.
Results
A total number of 72 UHC-attained countries were identified. Postgraduate education for primary care physicians exists in 62 countries (86%). Explicit statements that establish primary care postgraduate training were corresponded with the policy on UHC is found in 11 countries (18%). The naming of the program varies, general practice and family medicine were the commonest. In 33 countries (53%), physicians are required to undertake training to practice in primary level. The program duration ranged from 2–6 years with 3 years for the majority.
Conclusion
Although UHC is not the principal driving force for the establishment of postgraduate training for primary care physicians in many countries, most UHCattaining countries make substantial endeavor to ensure its formation as a part of their health care reform to improve national health.
Keywords
family medicine, general practice, primary care physician, universal health coverage, postgraduate training
Since the 1978 Alma Ata declaration of “Health for All” by countries attending the International Conference on Primary Health Care jointly organized by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), most nations acknowledged that health provision is a fundamental human right and that primary health care is the key to ensure the fulfillment of adequate health.1 However, although people are generally healthier, wealthier and live longer today than 39 years ago, health inequity persisted in many countries. The failure to achieve “health for all” has propelled a campaign for Primary Health Care Reforms which comprised universal health coverage (UHC) reforms, service delivery reforms, public policy reforms, and leadership reforms.2
In September 2015, the United Nations General Assembly launched the Sustainable Development Goals (SDGs) which included the third goal “to ensure healthy lives and promote well-being for all at all ages” that should be achieved in 2030.3 It is believed that development of systems capable of delivering health rely on the existence of health financing mechanisms that offer universal access to health. One of the targets to accomplish the goal is “the attainment of universal health coverage which includes financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all”.4
According to WHO, universal coverage is defined as “access to key promotive, preventive, curative, and rehabilitative health interventions for all at an affordable cost, thereby achieving equity in access.” The principle of financial-risk protection ensures that the cost of care does not put people at risk of financial catastrophe. A related objective of health-financing policy is equity in financing: households contribute to the cost of health care on the basis of ability to pay.5
Reform in service delivery in order to support the affordable cost and equity in access incorporates the availability of health care providers competent in delivering a person-centered, continuing, comprehensive and integrated health service; it is responsible for a defined population and able to coordinate support from hospitals, specialized services and civil society organizations.2 Therefore, the establishment of special training program for primary care physicians (general practitioner or family physician) is considered integral to primary health care (PHC) reforms in some countries.6
Even though this discipline is well established and mainstreamed in most developed nations, it is still relatively new in low and middle‑income countries. Studying the formation of postgraduate training in primary care within countries which have attained UHC is important to support the development of such education in low-and middle-income countries aiming to achieve UHC by 2030. In this review, we aim to describe the existence of the postgraduate training for primary care physicians in countries which have attained UHC.
METHODS
This study is a review of academic literature and official documents, both nationally and internationally. Review also includes secondary data collection from publicly available data and reports by major international organizations such as International Labor Organization (ILO) and WHO.
Identification of countries which have attained universal health coverage
A report by Stuckler et al5 identified 58 countries which have achieved UHC based on the following criteria.1 Healthcare legislation explicitly states that the entire population is covered under a specific health plan, including availability of package of services with identifiable year (and such legislative articles can be identified online);2 More than 90% of the residents of those country must have access to skilled attendance at birth and health care insurance (i.e. social health insurance, state coverage, private health insurance, and employer-based insurance), which serve as broader proxy indicators for access to care, using the latest data available and based on the ILO threshold.
To identify additional countries which meet the Stuckler criteria of attaining UHC, the list is updated using the ILO databases on social health protection coverage,7 supplemented with the data about access to skilled attendance at birth from the WHO Global Health Observatory data repository.8 Fourteen countries were added, thereby increasing to 72 countries included in this report.
The literature review methods
To identify the existence of postgraduate training for primary care physicians in the 72 UHC-attaining countries, online literature search was conducted using medical databases such as Medline and Google Scholar in February 2017. The keywords “postgraduate training” AND (“primary care” OR “general practice” OR “family medicine”) both as medical subject headings (MeSH) terms and freetexts, were utilized to identify reviews, surveys and country specific reports with regards to the establishment of postgraduate training on primary care/general practice/family medicine in those countries. A hand search was also conducted on the websites of regional and global health/primary care organizations or societies such as WHO, WONCA, European Forum for Primary Care, European Union of GP/FP, European Academy of Teachers in GP/FM, etc, as well as on the websites of GP/FP organizations in each respective country.
To explore the connection between establishment of primary care physician postgraduate education with UHC, another literature search was conducted using the terms “universal health coverage” OR “universal coverage” AND the name of each of the countries in the list. We concluded the relationship between the establishment of primary care specialist in one country and UHC policy if we found any statement specifying that primary care physician postgraduate education was started or endorsed as part of the UHC implementation policy in the respective countries.
RESULTS
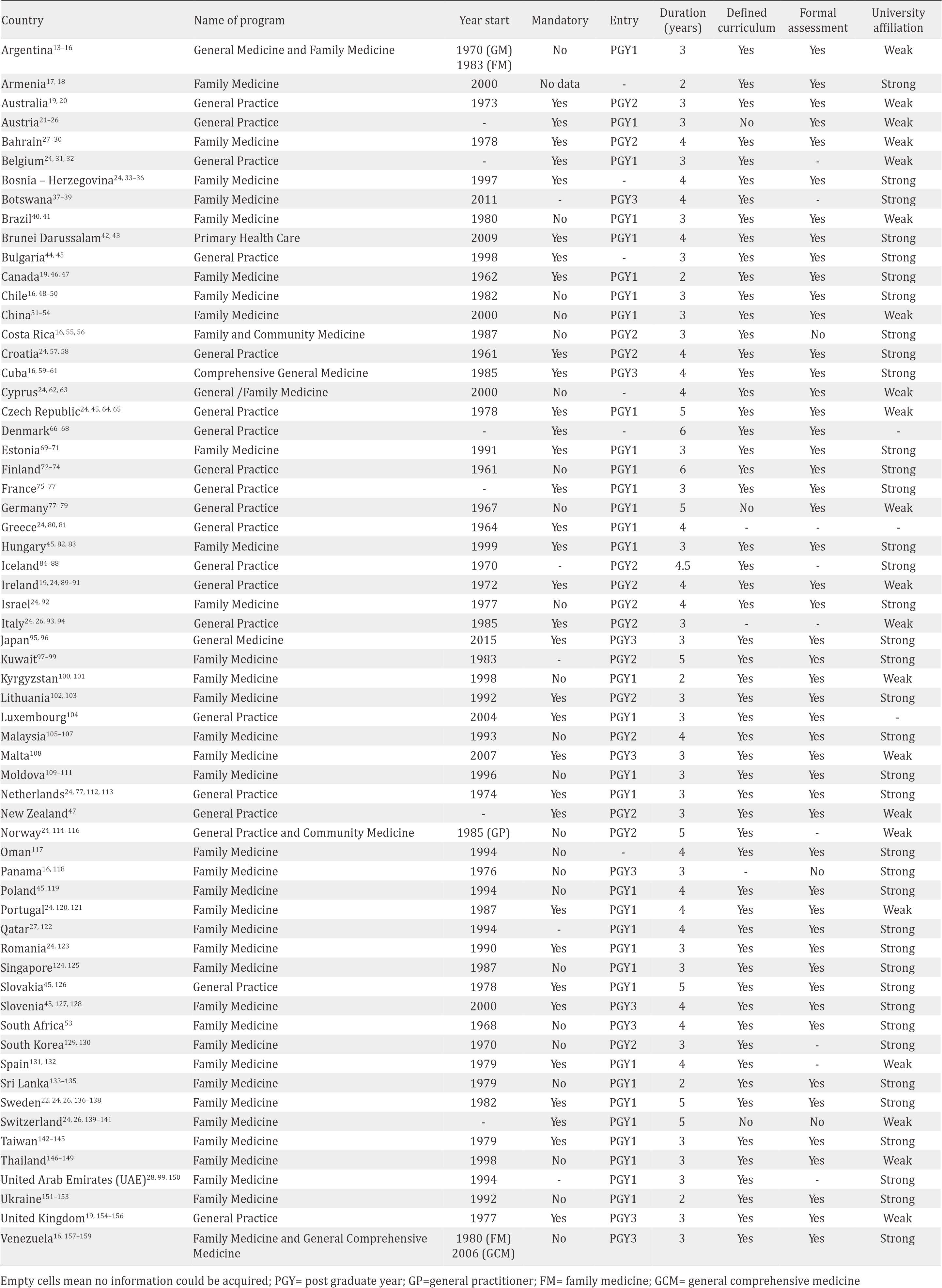
Postgraduate education for primary care physicians exists in 62 of 72 countries (86%) which attained UHC as shown in Table 1 although in Austria and Brunei Darussalam it is not recognized as specialist degree. The existence of the education could not be determined in Andorra, Antigua, and Mauritius. Only in 11 of 62 countries (18%) showed explicit statement that the establishment of primary care postgraduate education corresponded with the policy on UHC. Statements that education is established or reinforced as part of health care reforms through primary health care movement was found in several countries such as Brazil, China and South Africa. Other statement found was the recognition of the need for professional development of generalist physicians as a distinct medical discipline with its own training which can be identified in pioneering countries for the development of general practice/family medicine, such Canada, United Kingdom, Australia, and the Netherlands. Becoming members of regional organization requiring countries to adhere to standard in health care including training of primary care physicians was also influential in the establishment of training on primary care physicians as observed in the east of Europe and Arab gulf countries.
Table 1. Availability of primary care physician post-graduate education in the countries which attained universal health coverage

Table 2 displayed the features of the primary care physician postgraduate education in the 62 countries. The name of the program varies; general practice and family medicine were mostly described. In Argentina, Norway, and Venezuela, two postgraduate programs with different name exists. In Czech Republic, there are two separate groups of GPs, who never work in combined practices: GPs for adults and practitioners for children and adolescents, each with their own training program. The mandatory status of the program for those who wants to practice in primary health care could be ascertained in 33 of 62 (53%) countries. The duration of the program ranges from 2–6 years, in which three years is the most common.
Table 2. Characteristics of the primary care physician post-graduate education in countries which attained universal health coverage
DISCUSSION
Postgraduate education for primary care physicians exists in 86% countries which attained UHC. The link between the establishments of postgraduate education and the UHC implementation policy is explicitly stated in only 18% of the countries.
In many industrialized countries like Canada, United Kingdom, Australia, or the Netherlands, the postgraduate education for primary care physicians have been established since the 1960s or 1970s. It was fostered as a response to the declining general practice due to the rapid development of medical specialization in the first half of the twentieth century. The age of specialization resulted in the fragmentation of medical care which led to deterioration of doctorpatient relationship. A new kind of generalist with special training and qualifications armed with a defined set of skills is needed.9 The Alma- Ata declaration in 1978 which emphasized the importance of PHC to achieve “Health for All”1 further expanded the development of special training of primary care physicians in the wider part of the world since successful PHC systems usually involve a primary care doctor with postgraduate training in family medicine or general practice.2
Evidences from various studies on the effectiveness of strong PHC showed that with PHC specialist physicians holding the central role, there is an improvement of various health outcomes and with better use of health cost. A systematic review by Engström et al10 reported that an increase in the number of, or ratio of primary health care specialist physicians compared to total number of doctors, was significantly associated with lower mortality rates, neonatal death rate, rate of low birth weight; increased life expectancy and decreased total mortality and stroke. The same review also revealed that higher proportions of primary care physicians were associated with lower payments for both in-hospital and outof- hospital care while a greater supply of family doctors was significantly associated with lower reimbursements for outpatient care.
The reason why in some countries in this study, the establishment of postgraduate training for primary care physicians is linked to the effort in attaining the UHC could be found in a review by Kruk et al11 This review described how primary care strengthening contributed to increased access to services as well as equity in access and outcomes. Primary care emerged as foundation for health systems strengthening in the developing world, by improving cost efficiency and responsiveness. Similar observation has also been emphasized by Barbara Starfield.12
Our study is the first attempt to find link between the establishment of training for primary care physicians with universal health coverage. However, we acknowledged limitations of our study. The main source of limitation is that it relied heavily on the published literature which in some countries are very limited and outdated. Our decision to only including literature in English also limited information from the non-English speaking countries.
In conclusion, although UHC is not the principal driver of the establishment of postgraduate primary care physician education in many countries, most UHC-attaining countries made substantial endeavor to ensure the formation of those trainings as part of their health care reform to improve the national health.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
The authors appreciate the valuable inputs from Hadyana Sukandar and Dwi Agustian during the literature review process and the development of report.
REFERENCES
- World Health Organization. Alma-Ata 1978 Primary Health Care. Geneva: World Health Organization, 1978.
- World Health Organization. Primary health care now more than ever. Geneva: World Health Organization, 2008.
- GBD 2015 SDG Collaborators. Measuring the healthrelated Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1813–50.
- Garrett L, Chowdhury AMR, Pablos-Méndez A. All for universal health coverage. Lancet. 2009;374(9697):1294–9.
- Stuckler D, Feigl AB, Basu S, McKee M. The political economy of universal health coverage. Global symposium on health systems research; Montreux, Switzerland. Geneva: World Health Organization; 2010. p. 11–3.
- Williams RL, Henley E, Prueksaritanond S, Aramrattana A. Family Practice in Thailand: Will It Work? J Am Board Fam Med. 2002;15(1):73–6.
- www.ilo.org [Internet]. International Labour Organization. ILOSTAT. Geneva: International Labour Organization; 2016. [update 2017; cited 2017 Feb]. Available from: http://www.ilo.org/ilostat/faces/wcnav_ defaultSelection?_adf.ctrl-state=131zmqr4t4_91&_ afrLoop=28105723263739&_afrWindowMode=0&_ afrWindowId=131zmqr4t4_117#!.
- World Health Organization. Global Health Observatory Data Repository. 2012. [update 2016; cited February 2017]. Available from: http://apps.who.int/gho/data/ view.main.1610?lang=en.
- McWhinney IR, Freeman T. Textbook of Family Medicine. 3rd ed. Oxford: Oxford University Press; 2009. p. 460.
- Engström S, Foldevi M, Borgquist L. Is general practice effective? A systematic literature review. Scand J Prim Health Care. 2001;19(2):131–44.
- Kruk ME, Porignon D, Rockers PC, Van LW. The contribution of primary care to health and health systems in low- and middle-income countries: A critical review of major primary care initiatives. Soc Sci Med. 2010;70(6):904–11.
- Starfield B. Primary care: an increasingly important contributor to effectiveness, equity, and efficiency of health services. SESPAS report 2012. Gac Sanit. 2012;26(Suppl 1):20–6.
- Haq C, Ventres W, Hunt V, Mull D, Thompson R, Rivo M, et al. Where there is no family doctor: The development of Family Medicine around the world. Acad Med. 1995;70(5):370–80.
- Lopez E, Blanco M, editors. Starting family medicine in Argentina. Presentation at WONCA World Conference. 2004 October 13–17; Orlando, USA.
- Pan American Health Organization. Health in the Americas. Washington DC: World Health Organization, 2012.[updated 2012; cited 2017 Feb]. Available from: http://www.paho.org/salud-en-las-americas-2012/ index.php?option=com_content&view=article&id=18& Itemid=129&lang=en.
- Spann SJ. Primary Care and General Practice in Latin America. In: Jones R, Britten N, Culpepper L, Gass D, Grol R, Mant D, et al., editors. Oxford Textbook of Primary Medical Care. Oxford: Oxford University Press;2005. p. 62–4.
- Hovhannisyan SG, Tragakes E, Lessof S, Aslanan H, Mkrtchyan A. Health care system in transition: Armenia. Copenhagen: European Observatory on Health Care Systems, 2001. p. 41–7.
- Ohanyan M, Danielyan A, Hopaiyan K, Mash B. Making strides towards Family Medicine in Armenia. Br J Gen Pract. 2015;65(635):308–9.
- Hays RB, Morgan S. Australian and overseas models of general practice training. Med J Aust. 2011;194(11):63.
- Trumble SC. The evolution of general practice training in Australia. Med J Aust. 2011;194(11):59–62.
- Hofmarcher MM. Health Systems Review: Austria. Copenhagen: World Health Organization, 2013. p. 151–64.
- Masseria C, Irwin R, Thomson S, Gemmill M, Mossialos E. Primary care in Europe. Policy brief. The London School of Economics and Political Science. 2009. Sponsored by the European Commission.
- Redaèlli M, Wilm S, Simic D, Sprenger M. Austria. Kringos DS, Boerma WGW, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: European Observatory on Health Systems and Policies; 2015. p. 1–9.
- Sammut MR, Lindh M, Rindlisbacher B, On behalf of Euract-the European Academy of Teachers in General Practice. Funding of vocational training programmes for general practice/family medicine in Europe. Eur J Gen Pract. 2008;14(2):83–8.
- Spiegel W, Pichlhöfer O, Haoula D, Schneider B, Maier M. Specialty selection and relative job satisfaction of family physicians and medical specialists in Austria. Croat Med J. 2008;49:375–83.
- The New Leeuwenhorst Group [Internet]. A commentary on the present state of learning and teaching general practice in Europe. [update 1985; cited 2017 Feb]. Available from: http://euract.woncaeurope. org/sites/euractdev/files/documents/archive/ publications/commentary-present-state-learning-andteaching- general-practice-europe-new-leeuwenhorstgroup- 1985.pdf
- Abyad A. Family Medicine in the Middle East: Reflections on the Experiences of Several Countries. J Am Board Fam Pract. 1996;9(4):289–97.
- Abyad A, Al-Baho AK, Unluoglu I, Tarawneh M, Al Hilfy TKY. Development of Family Medicine in the Middle East. Fam Med. 2007;39(10):736–41.
- Al-Al-Tahoo L. Health System Profile: Bahrain. Cairo: World Health Organization - Eastern Mediterranian Region, 2007. p. 51–4.
- Alnasir FAL. Family Medicine in the Arab world. Is it a luxury? Lecture presented at Health Congress 2011, December 14–6; Kurdistan, Iraq.
- Cartier T, Ryssaert L, Bourgueil Y. Belgium. In: Kringos DS, Boerma WGW, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe - Case studies. Copenhagen: European Observatory on Health Systems and Policies; 2015. p. 9–18.
- Gerkens S, Merkur S. Health System Review: Belgium. Health systems in transition. 2010;12(5):1–266.
- Jatić Z, Račić M. Family medicine education in Bosnia and Herzegovina. EURACT Messenger. 2015(4):1–2.
- Masic I, Skopljak A, Jatic Z. Comparative review of Education Programs of Family Medicine (FM) in Bosnia and Herzegovina and Several Transition Countries. Mater Sociomed. 2014;26(6):411–8.
- Račić M. Family Medicine Development in Bosnia and Herzegovina. J Fam Med. 2015;2(4):1031.
- Švab I, Pavliè DR, Radić S, Vainiomäki P. General practice east of Eden: an overview of general practice in Eastern Europe. Croat Med J. 2004;45:537–42.
- Mbuka DO, Tshitenge S, Setlhare V, Tsima B, Adewale G, Parsons L. New family medicine residency training programme: Residents’ perspectives from the University of Botswana. Aft J Prim Health Care Fam Med. 2016;8(1):1–8.
- Ogundipe RM, Mash R. Development of Family Medicine training in Botswana: Views of key stakeholders in Ngamiland. Afr J Prm Health Care Fam Med. 2015;7(1):1–9.
- University of Botswana Faculty of Medicine. Master in Medicine programme. Gaborone, Botswana: University of Botswana; [cited 2017; cited 2017 Jan]; Available from: http://www.ub.bw/programdet/pid/187//master-inmedicine/.
- Haq C, Gusso G, Anderson MIP. Strengthening Primary Health Care with Family and Community Medicine in Brazil. Rev Bras Med Fam e Com. 2006;2(7):196–202.
- Rodnick JE, Blasco P. Brazil: Family medicine in Brazilestablishing the specialty. Fam Med. 2005;37(9):668.
- Starkey C, Matthews B. A modular family medicine training program at the master’s-degree level and taught at a distance. Acad Med. 2001;76(5):569–9.
- Anonim. Specialty training and career structure for family medicine in Brunei Darussalam [power point presentation]. Available from: http://docslide.net/ documents/specialty-training-and-career-structurefor- family-medicine-in-brunei-darussalam.html.
- Kringos D, Salchev P. Bulgaria. In: Kringos DS, Boerma WGW, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe - Case studies. Copenhagen: European Observatory on Health Systems and Policies; 2015. p. 19–29.
- Krztoń-Królewiecka A, Švab I, Oleszczyk M, Seifert B, Smithson WH, Windak A. The development of academic family medicine in central and eastern Europe since 1990. BMC Family Practice. 2013;14(37):1–10.
- Hennen BKE. Academic family medicine in Canada. Can Med Assoc J. 1993;148(9):1559–63.
- Pullon S. Training for family medicine in Canada and general practice in New Zealand: how do we compare? J Prm Health Care. 2011;3(1):82–5.
- Bossert TJ, Leisewitz T. Innovation and Change in the Chilean Health System. N Engl J Med. 2016;374(1):1–5.
- Organisation for Economic Co-operation and Development. Health Systems Characteristics Survey 2012 and 2016. Organisation for Economic Co-operation and Development (OECD), 2016.p.4. [update 2017; cited Feb 2017]. Available from: stats.oecd.org/fileview2. aspx?IDFile=f1d6c79f-6f31-4435-8147-172cba38f3ad
- Wonca News [Internet]. From the President: The theme is team - Primary Health Care in Chile. [update 2017; cited 2017 Feb]. Available from: http://www.wonca. net/News/FromthePresidentThethemeisteam-
- PrimaryHealthCareinChile.aspx. 51. Chen T, Du Y, Sohal A, Underwood M. Essay - Family medicine education and training in China: past, present and future. Br J Gen Pract 2007;57(541):674–6.
- Dai H, Fang L, Malouin RA, Huang L, Yokosawa KE, Liu G. Family Medicine Training in China. Fam Med. 2013;45(5):341–4.
- Mash R, Almeida M, Wong WC, Kumar R, von Pressentin KB. The roles and training of primary care doctors: China, India, Brazil and South Africa. Human Resources for Health. 2015;13:1–9.
- Wang J, Kushner K, Frey III JJ, Du XP, Qian N. Primary Care Reform in the Peoples’ Republic of China: Implications for Training Family Physicians for the World’s Largest Country. Fam Med. 2007;39(9):639–43.
- Kidd M. From the President: Family Medicine in Costa Rica. WONCA News. 2016;42(4):2–4.
- Scyner A. Family and community medicine in Costa Rica: where professionalization meets development. Montreal: McGill University; 1997.
- Katiæ M, Jureša V, Oreškoviæ S. Family Medicine in Croatia: Past, Present, and Forthcoming Challenges. Croat Med J. 2004;45(5):543–9.
- Keglević MV. Family Medicine/General Practice in Croatia: some facts [power point presentation].
- Cardelle AJ. The preeminence of primary care within Cuban predoctoral medical education. International Journal of Health Services. 1994;24(3):421–9.
- Demers R, Kemble S, Orris M, Orris P. Family Practice in Cuba; evolution into the 1990s. Family Practice. 1993;10:164–8.
- Keck CW, Reed GA. The Curious Case of Cuba. American Journal of Public Health. 2012;102(8):e13–22.
- Samoutis G, Tedeschi P. Cyprus. In: Kringos DS, Boerma WGW, Hutchinson A, Saltman RB, editors. European Observatory on Health Systems and Policies. Copenhagen: World Health Organization; 2015. p. 31–40.
- University of Nicosia Medical School. Postgraduate Diploma and Masters in Family Medicine. In: University of Nicosia Medical School, editor. Nicosia, Cyprus: University of Nicosia Medical School; 2016. p. 1–8.
- Vychytil P, Marx D. The reform of specialist training for general practice in the Czech Republic. Cent Eur J Public Health. 2009;17(3):146–51.
- Windak A, Oleszczyk M, Seifert B. Czech Republic. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015. p. 41–8.
- Forde I, Nader C, Socha-Dietrich K, Oderkirk J, Colombo F. Primary Care Review of Denmark. Paris: Organisation for Economic Co-operation and Development, 2016. p. 6–16.
- Hasvold T. Denmark. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015. p. 49–56.
- Pedersen KM, Andersen JS, Søndergaard J. General Practice and Primary Health Care in Denmark. J Am Board Fam Med. 2012;25:S34–8.
- Maaroos H-I, Lember M. Specialist training of family physicians in non-UEMO countries: An Estonian experience. European Journal of General Practice. 2007;13(4):246–7.
- Põlluste K, Lember M. Estonia. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015. p. 57–66.
- Polluste K, Lember M. Primary health care in Estonia. Family Medicine & Primary Care Review 2016;18(1):74– 7.
- Sumanen M, Aine T, Halila H, Heikkilä T, Hyppölä H, Kujala S, et al. Where have all the GPs gone – where will they go? Study of Finnish GPs. BMC Family Practice. 2012;13(121).
- Vuorenkoski L. Finland: Health System Review. Copenhagen: World Health Organization, 2008. p. 85– 121.
- Winell K, Dedeu T. Finland. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015. p. 67–75.
- Cartier T, Bourgueil Y. France. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015. p. 77–87.
- Horder J. Training for general practice at Bobigny, Paris. Journal of the Royal College of General Practitioners. 1975;25:197–9.
- Miani C, Hinrichs S, Pitchforth E, Bienkowska-Gibbs T, Disbeschl S, Roland M, et al. Best Practice: Medical training from an international perspective. Santa Monica, California: RAND Corporation, 2015;5(1):2.
- Knabe H. The training of the general practitioner in the German Democratic Republic. J Roy Coll Gen Pract. 1969;18:374–6.
- Simic D, Wilm S, Redaèlli M. Germany. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015. p. 89–98.
- Economou C. Greece: Health system review. Copenhagen: World Health Organization, 2010 Contract No: 7.
- Mariolis A, Mihas C, Alevizos A, Gizlis V, Mariolis T, Marayiannis K, et al. General Practice as a career choice among undergraduate medical students in Greece. BMC Med Educ. 2007;7(15):1–8.
- Rurik I. Postgraduate education, vocational training in the Family Medicine in Hungary. Stary Smokovec. 2012.
- Wilm S, Vajer P, Rurik I. Hungary. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015.
- Bardardottir E. News from the Nordic Colleges of General Practitioners. Scandinavian Journal of Primary Health Care. 2006;24(3):129–30.
- Halldorsson M. Health Care Systems in Transition: Iceland. Copenhagen: WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies, 2003.
- Hutchinson A. Iceland. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015.
- Jónsdóttir SH. General Practice in Iceland at the turn of the millennium. Rome: European Union of General Practitioners, 2000.
- Solberg IB, Tómasson K, Aasland O, Tyssen R. The impact of economic factors on migration considerations among Icelandic specialist doctors: a cross-sectional study. BMC Health Services Research. 2013;13(524):1–7.
- Hutchinson A. Ireland. In: Kringos DS, Boerma WG, Hutchinson A, Saltma RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015.
- Irish College of General Practice. A career in General Practice. In: Irish College of General Practice, editor.: Irish College of General Practice; 2006.
- McDaid D, Wiley M, Maresso A, Mossialos E. Ireland: Health System Review. Copenhagen: World Health Organization on behalf of the European Observatory on Health Systems and Policies, 2009.
- Tandeter H. Family Medicine in Israel: A national overview and examples from Ben-Gurion University in the Negev. Archivos en Medicina Familiar. 2007;9(1):65–70.
- Tedeschi P. Italy. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe - Case studies. Copenhagen: European Observatory on Health Systems and Policies; 2015. p. 133–43.
- Cegolon L, Heymann W. International primary care snapshot: academic primary care in Italy. British Journal of General Practice. 2016. p. 34.
- Takamura A. The present circumstance of primary care in Japan. Quality in Primary Care. 2015;23(5):262–6.
- Takamura A. The new era of postgraduate certified general practice training in Japan. Education for Primary Care. 2016. p. 1–4.
- Al-Baho AK, Serour M. Development of Family Practice Specialty Training Program over a 20-year period (1983–2002) in Kuwait. Bulletin of the Kuwait Institute for Medical Specialization. 2003;2:59–63.
- Almussalam S, Serour M, Alwagayan A, Alzayed K, Buhamra A, Alnajjar A, et al. Family Medicine Residency Program Trainers’ & Residents’ Guide to the curriculum: Kuwait Institute for Medical Specialization Faculty of Primary Healthcare; 2014.
- Osman H, Romani M, Hlais S. Family Medicine in Arab Countries. Fam Med. 2011;43(1):37–42.
- Fonken P, Brouhard K, Chubakov T, Djuzenova B, Pirnazarova G, Burns D, et al. Family Medicine in Kyrgyzstan: The First Nine Years 1996–2005. Bishkek, Kyrgyzstan: USAID, 2005. p .11–26.
- Hardison C, Fonken P, Chew T, Smith B. The Emergence of Family Medicine in Kyrgyzstan. Fam Med. 2007;39(9):627–33.
- Jurgutis A, Jukneviciute V. Primary Care in Lithuania. Utrecht, the Netherlands: European Forum for Primary Care; [update 2013; cited 2017 Feb]; Available from: http://www.euprimarycare.org/column/primary-carelithuania.
- Kasiulevičius V, Lember M. Lithuania. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 155–61.
- Kringos D, Aubart M, Leners J, Stein R. Luxembourg. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 163–70.
- Ng CJ, Teng CL, Abdullah A, Wong CH, Hanafi NS, Phoa SSY, et al. The status of Family Medicine training programs in the Asia Pacific. Fam Med. 2016;48(3):194–202.
- Academy of Family Physicians of Malaysia. Graduate Certificate in Family Medicine. Kuala Lumpur: Academy of Family Physicians of Malaysia; [update 2016 ; cited 2017 Feb]; Available from: https://www.afpm.org.my/ programmegcfm.
- University of Malaya. Master of Family Medicine (MFamMed). Kuala Lumpur: University of Malaya; [update 2016; cited 2017 Feb]; Available from: https:// www.um.edu.my/academics/master/medicine/ master-of-family-medicine.
- Camilleri AF, Sammut D. A Curriculum for Specialist Training in Family Medicine for Malta: Malta College of Family Doctors; 2009. p. 7–11.
- Galbur O. Concerning the comparative analysis of the classification and lists of the medical specialities in the EU and Republic of Moldova with concrete suggestions of improvement and fittings to the European Standards. Chisinau, Moldova: 2010.
- Atun R, Berdaga V, Turcan L, Stefanetz S, Cibotaru E, Ibragimov A. Review of Experience of Family Medicine in Europe and Central Asia: Moldova Case Study. World Bank, 2005 Contract No: 32354-ECA.
- Zarbailov N, Carelli F. Family medicine development in the Republic of Moldova - Trends in European education of Family Physicians. The Synapse. 2017. [updated 2017; cited 2017 Feb]. Available from: http:// www.thesynapse.eu/corporate/associates/jamesco/ item/321-family-medicine-development-in-therepublic- of-moldova-trends-in-european-education-offamily- physicians.
- Kroneman M, Boerma W, van den Berg M, Groenewegen P, de Jong J, van Ginneken E. The Netherlands: health system review. Health Systems in Transition. 2016;18(2):1–239.
- Kringos D, Paap JvR, Boerma W. The Netherlands. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 181–92.
- Westin S, Östensen AI. General Practice Recognized as a Speciality in Norway. Scandinavian Journal of Primary Health Care. 1987;5(1):60–1.
- Hasvold T, Christensen B. Norway. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 193–200.
- Rørtveit G. Primary Care in Norway. Utrecht, the Netherlands: European Forum for Primary Care; 2017 [update 2017; cited 2017 Feb]; Available from: http:// www.euprimarycare.org/column/primary-care-norway.
- Al-Shafaee M. Family Medicine Practice in Oman, Present and future. Squ Med J. 2009;9(2):116–8.
- Knox L, Ceitlin J, Hahn RG. Slow Progress: Predoctoral education in Family Medicine in four Latin American countries. Fam Med. 2003;35(8):591–5.
- Sagan A, Panteli D, Borkowski W, Dmowski M, Domański F, Czyżewski M, et al. Poland: Health system review. Health Systems in Transition. 2011;13(8):1–193.
- Kumar R, Barata AN, Floss M. Primary care education: medical student and young doctors’ perspective from Brazil, India and Portugal. Education for Primary Care. 2016;27(5):345–8.
- Fonseca C, Dedeu T, Pisco L, Gouveia A. Portugal. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 211–22.
- Verjee MA, Abdulmalik MA, Fetters MD. Family medicine’s rapid establishment and early leadership role in Qatar’s health care system. Journal of Healthcare Leadership. 2013;5:47–52.
- Pavlič DR, Miftode R, Balan A, Pall ZF. Romania. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 223–32.
- Thomas SL. Family Medicine Specialty in Singapore. J Family Med Prim Care. 2013;2(2):135–40.
- Goh LG, Ong CP. Education and training in family medicine: progress and a proposed national vision for 2030. Singapore Med J. 2014;55(3):117–23.
- Windak A, Oleszczyk M, Jurgova E. Slovakia. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 233–42.
- Pavlič DR, Švab I, Pribaković RB. Slovenia. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in a changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 243–52.
- Bulc M, Švab I, Pavlič DR, Kolšek M. Specialist training of Slovene family physicians. European Journal of General Practice. 2006;12(3):128–32.
- Chun CB, Kim SY, Lee JY, Lee SY. Health System Review: Republic of Korea. Health System in Transition. 2009;11(7):1–184.
- Paek YJ, Shin HC, Kim CH, Choi YS, Lee H, Cho AK, et al. Curriculum and Training Difficulties of Family Medicine Residency Programs in Korea. Korean J Fam Med. 2007;28(5):367–74.
- Dedeu T, Bolibar B, Gené J, Pareja C, Violan C. Building primary care in a changing Europe - Case studies. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Copenhagen, Denmark. European Observatory on Health Systems and Policies2015. p. 253–64.
- Gofin J, Foz G. Training and application of Communityoriented Primary Care (COPC) through Family Medicine in Catalonia, Spain. Fam Med. 2008;40(3):196–202.
- de Silva A, Ranasinghe T, Abeykoon P. Universal health coverage and the health Sustainable Development Goal: achievements and challenges for Sri Lanka. WHO South- East Asia J Public Health 2016;5(2):82–8.
- Ramanayake R. Historical Evolution and Present Status of Family Medicine in Sri Lanka. Journal of Family Medicine and Primary Care. 2013;2(2):131–4.
- World Health Organization - Regional Office for South East Asia. Regional Consultation on Strengthening the Role of Family/Community Physicians in Primary Health Care. New Delhi: World Health Organization, 2012. p. 11–3.
- Anell A, Glenngård AH, Merkur S. Sweden: Health system review. Copenhagen: World Health Organization, 2012 Contract No: 5.
- Björkelund C, Maun A. Primary Care\\ in Sweden. Utrecht: European Forum for Primary Care; 2017 [updated 2017; cited 2017 Feb]. Available from: http:// www.euprimarycare.org/column/primary-care-sweden.
- Hasvold T. Sweden. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in changing Europe. Copenhagen: World Health Organization; 2015. p. 265–74.
- Buddeberg-Fischer B, Stamm M, Marty F. Family Medicine in Switzerland: Training Experiences in Medical School and Residency. Fam Med. 2007;39(9):651–5.
- Cartier T, Senn N, Cornuz J, Bourgueil Y. Switzerland. In: Kringos D, Boerma W, Hutchinson A, Saltman R, editors. Building primary care in changing Europe - Case studies. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2015. p. 275–84.
- Clarke O, Lindh EM, Sammut MR, Price R, Svavardottir AE, O’Shea B, et al. Training, status and migration of General Practitioners/Family Physicians within Europe. The Journal of the Malta College of Family Doctors. 2013;2(2):24–30.
- Chen S-C, Yen C-H, Chen C-C, Wu W-Y, Chou M-C, Bell W, et al. Outpatient teaching in family medicine residency training programs in Taiwan. Asia Pacific Family Medicine. 2004;4:1–5.
- Lee M. Education and training of family medicine in Taiwan. Journal of Capital Medical University. 2013;34(2):218–23.
- Lee M. Integrated care and training in family practice in the 21st century: Taiwan as an example. Family Medicine and Community Health. 2016;4(1):57–9.
- Yen E. Family practice instructional development models in Taiwan, review and prospective. Kaohsiung J Med Sci. 1996;12(11):641–5.
- Jaturapatporn D, Dellow A. Does Family Medicine training in Thailand affect patient satisfaction with primary care doctors? BMC Family Practice. 2007;8(14):1–6.
- William R, Henley E, Prueksaritanond S, Aramrattana A. Family Practice in Thailand: Will it Work? JABFP. 2002;15(2):73–6.
- Wiwanitkit V. Family medicine in Thailand: System, training, and obstacles. Medical Journal of Dr DY Patil University. 2016;9(1):1–6.
- World Health Organization - Regional Office for South East Asia. Family Medicine - Report of a Regional Scientific Working Group Meeting on Core Curriculum. New Delhi: World Health Organization - Regional Office for South East Asia, 2003. p. 9–16.
- Ibrahim H, Nair SC, Shaban S, El-Zubeir M. Reducing the Physician Workforce Crisis: Career Choice and Graduate Medical Education Reform in an Emerging Arab Country. Education for Health. 2016;29(2):82–8.
- Gibbs T, Khimion L, Lysenko G. Family medicine in Ukraine: changing theory into practice and completing the circle. British Journal of General Practice. 2008:654–6.
- Kolesnyk P, Švab I. Development of family medicine in Ukraine. European Journal of General Practice. 2013;19:261–5.
- Korzh O. Primary Care in Ukraine. Utrecht: European Forum for Primary Care; [Update: 2 February 2017]; Available from: http://www.euprimarycare.org/ column/primary-care-ukraine.
- Chouinard J. Mandatory training for general practice in the United Kingdom. Can Med Assoc J. 1978;119(8):861.
- NHS Choices. The NHS in England. London: National Health Service; [ update 2016; cited 2017 Feb]; Available from: http://www.nhs.uk/NHSEngland/thenhs/about/ Pages/overview.aspx.
- Wilson A. United Kingdom. In: Kringos DS, Boerma WG, Hutchinson A, Saltman RB, editors. Building primary care in a changing Europe. Copenhagen: World Health Organization; 2015.
- María A. Mejía OMQ, María C. D’Avila and Carmen C. Silva. Current situation of family medicine in Venezuela. Aten Primaria. 2007;39(9):495–6.
- Romero N, Gruber F, Rincon M, Thompson R. Teaching family and community dimensions of clinical family medicine in Venezuela. Fam Med. 1994;26(2):89–92.
- Thompson R, Gruber F, Marcano G. Family medicine training in Venezuela. Fam Med. 1992;24(3):188–90.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id