
Section Abstract Introduction Methods Results Discussion Conflict Of Interest Acknowledgment References
Clinical Research
Diagnostic accuracy of magnetic resonance imaging in detecting anterior cruciate ligament injuries
pISSN: 0853-1773 • eISSN: 2252-8083
http://dx.doi.org/10.13181/mji.v26i3.1873 Med J Indones. 2017;26:218–23
Received: February 15, 2017
Accepted: June 04, 2017
Author affiliation:
Department of Orthopedics and Spine, Ghurki Trust Teaching Hospital, Lahore, Pakistan
Corresponding author:
Ashfaq Ahmed
E-mail: ashfaqjadoon40@yahoo.com
Background
The anterior cruciate ligament (ACL) stabilizes the joint during hyperextension and prevents anterior translation over femur. The objective of this study was to determine the diagnostic accuracy of magnetic resonance imaging (MRI) in detecting ACL injury by taking arthroscopy as gold standard in patients with traumatic knee injury.
Methods
Patients fulfilling the study criteria were treated with clinical examination, MRI and then arthroscopy at the Department of Orthopedics and Spine in the Ghurki Trust Teaching Hospital, Lahore. The accuracy, sensitivity and specificity of MRI in diagnosing the anterior cruciate ligament injury were calculated based on arthroscopic findings. All the data were analyzed using SPSS 17.0 version.
Results
A total 185 patients were included. 91.1% were males and 8.9% were females with Mean age of 28.25±0.433. The accuracy of MRI in diagnosing the anterior cruciate ligament was 91.89%, with sensitivity of 93.33%, specificity of 85.71%, positive predictive value of 96.55% and the negative predictive value of 75%.
Conclusion
MRI is accurate and non-invasive modality for the assessment of ligamentous injuries. It can be used as a first line investigation to patients with suspicion of ACL injury.
Keywords
ACL, arthroscopy, knee, MRI
The anterior cruciate ligament is currently the most common ligament injury in the knee joint. The number of incidences is as many as 1 in 3,500 individuals each year.1 Sports like skiing, ice hockey, and gymnastics can also produce enough stress to disrupt knee ligaments. Automotive accidents, especially those involving motorcycles, are common causes of knee ligament disruptions. Sudden severe loading without a fall or contact, like deceleration of a running athlete can also cause ligament disruption.2–3
The anterior cruciate ligament is the major stabilizer of knee joint. It prevents the anterior tibial displacement over the femur. Selective sectioning of the anterior cruciate ligament has shown that the anteromedial band is tight in flexion, providing the primary restraint, whereas the posterolateral bulky portion of this ligament is tight in extension.4 The posterolateral bundle provides the primary resistance for hyperextension.
There are many modalities to diagnose the anterior cruciate ligament (ACL) injury, however good history and physical examination are the key steps. The patient’s history of the experience (i.e., the knee’s buckling or jumping out of place; an audible pop; the location, severity, and relative time at the onset of pain; the ability to walk after the injury occurred) is important.5 In physical examination, anterior drawer and Lanchman tests are most useful tests. The Lanchman test is most sensitive for anterior tibial displacement.4–6
Imaging and arthroscopy are two most common modalities. Magnetic resonance imaging has several advantages over arthroscopy. Magnetic resonance imaging is sensitive, non-invasive and accurate in detecting soft tissue injuries of knee.7 It is a reliable method to confirm the clinical diagnosis and may even reveal the ligament tears which may be missed by arthroscopy.8–9
Ligament tears can be accurately assessed with MRI, but distinguishing partial tears from ruptures of the ACL can be challenging. Determining the extent of a partial tear is often extremely difficult to accurately assess.7–10 However, it is a routinely prescribed test in suspecting soft tissue injuries of knee. Kostov H. et al6 reported 83% sensitivity, 88.37% specificity, 93% positive predictive value, 74.5% negative predictive value, 82.5% accuracy in detecting anterior cruciate ligament. The prevalence of ACL tear in knee injuries is 14.4%.11
Arthroscopy directly visualizes all the internal structures of the knee joint. It can be used as a diagnostic and at the same time as a therapeutic tool. The knee is the joint in which arthroscopy has its greatest diagnostic and intra articular surgical application.12 The usefulness of arthroscopic techniques in diagnosis and treatment of intra articular pathology has been well documented.10 Arthroscopy needs special instruments and expert surgeons. This makes arthroscopy more costly than magnetic resonance imaging (MRI). The main aim of this study is to determine the efficacy of MRI in detecting the anterior cruciate ligament injuries in our set up.
METHODS
This descriptive study uses a non-probability consecutive sampling at the Department of Orthopedics and Spine Centre, Ghurki Trust Teaching Hospital, Pakistan from January 1st, 2016 to December 31st, 2016. A written informed consent from every patient and approval from the Hospital Ethical Committee were obtained. 185 patients with the ages between 16–55 years of both sexes having had recent post traumatic knee injuries within two months were included in the study. While the patients having inconclusive findings on MRI, degenerative changes on X-rays or having previous history of knee surgery or managed conservatively or not in the range of above inclusion age were excluded from the study. All patients with positive anterior drawer test and positive Lachman test were subjected to MRI. However patients who had already done MRI were also included. Images of magnetic resonance were performed with 0.5 tesla (Philips Medical system) at the Radiology Institute Ghurki Trust Teaching Hospital, Lahore Medical and Dental College, Lahore. Standardized magnetic resonance imaging protocol consisted of sagittal, coronal and axial sequences in section thickness of 3–5 mm. Magnetic resonance images were reported by a consultant radiologist who then determined whether the ACL is intact or torn. Arthroscopy were performed after informed consent and demographic information like name, age and gender were recorded. All arthroscopies were performed by the same consultant orthopedic surgeons who were blinded to the radiologist’s diagnosis. He determined whether the ACL intact or torn.
Arthroscopy was done in a standardized manner using inferolateral and medial portal which include the survey of the entire joint and anatomical structure, lesions involved with the presence or absence of tear, its location, status of the articular cartilage.
Statistics
The collected data were entered initially on a pre-formed proforma and then analyzed using statistical product and service solution (SPSS) version 17. Sensitivity, specificity, positive predictive value, negative predictive value and accuracy were calculated by generating a 2×2 contingency table. Categorical variables like ACL injury on MRI and on arthroscopy and gender were summarized using frequency and percentages. Quantitative variables like age and body mass index (BMI) were presented as mean ± SD.
Data were stratified by age, gender and BMI to address effect modifiers. A post-stratification Chi-square test was applied with p≤0.05 as significant.
RESULTS
This study included 185 patients out of which 168 (91.1%) were males and 17 (8.9%) were female. The male to female ratio of 9.88:1 and the mean age was 28.25±12.25 years. The different characteristics such as right or left knee involvement, patients from different age groups, mechanism of injury and body mass index are summarized in Table 1.
Table 1. Basic demographic characteristics of patients
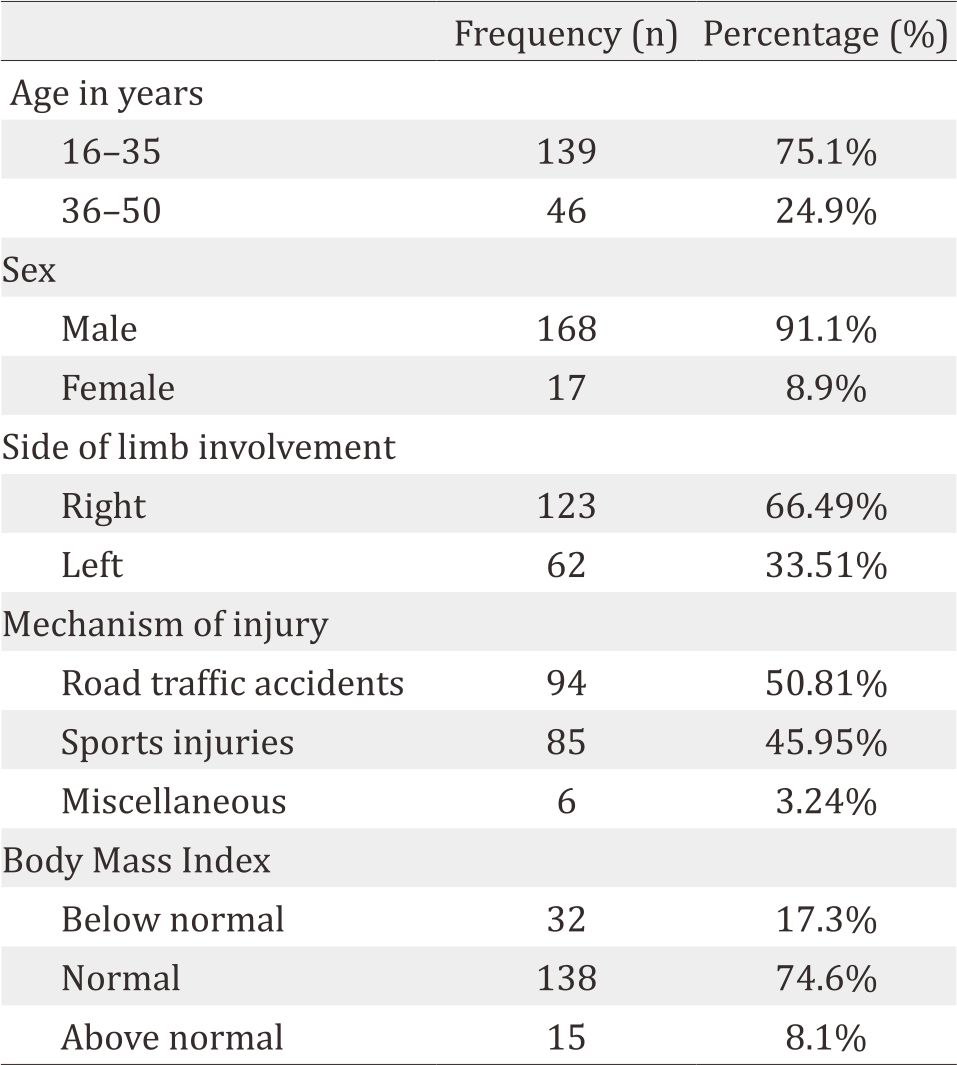
The arthroscopic findings for the ACL tear were positive for 150 (81.08%) compared to MRI findings, i.e. 145 (78.37%). The arthroscopic findings were negative for 35 (18.92 %) and on MRI it was 40 (21.62%). The results of different variables like sensitivity, specificity, positive and negative predictive value and accuracy of MRI and arthroscopy are summarized in Table 2.
Table 2. Comparison of MRI to arthroscopic findings in ACL injury detection
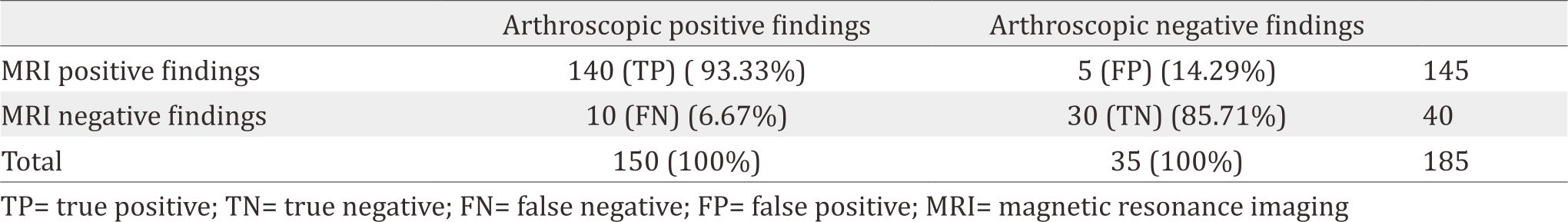
Though the gold standard of detecting anterior cruciate ligament injuries is arthroscopy, the diagnostic accuracy of MRI is also much more. The sensitivity and specificity of MRI in detecting anterior cruciate ligament injuries is 93.33% and 85.71%. Similarly MRI has high positive and negative predictive value, i.e. 96.55% and 75%. The arthroscopic and MRI pictures of two patients having sports injury and trauma to knee joints are given in Figure 1 (a, b) and Figure 2 (a, b).
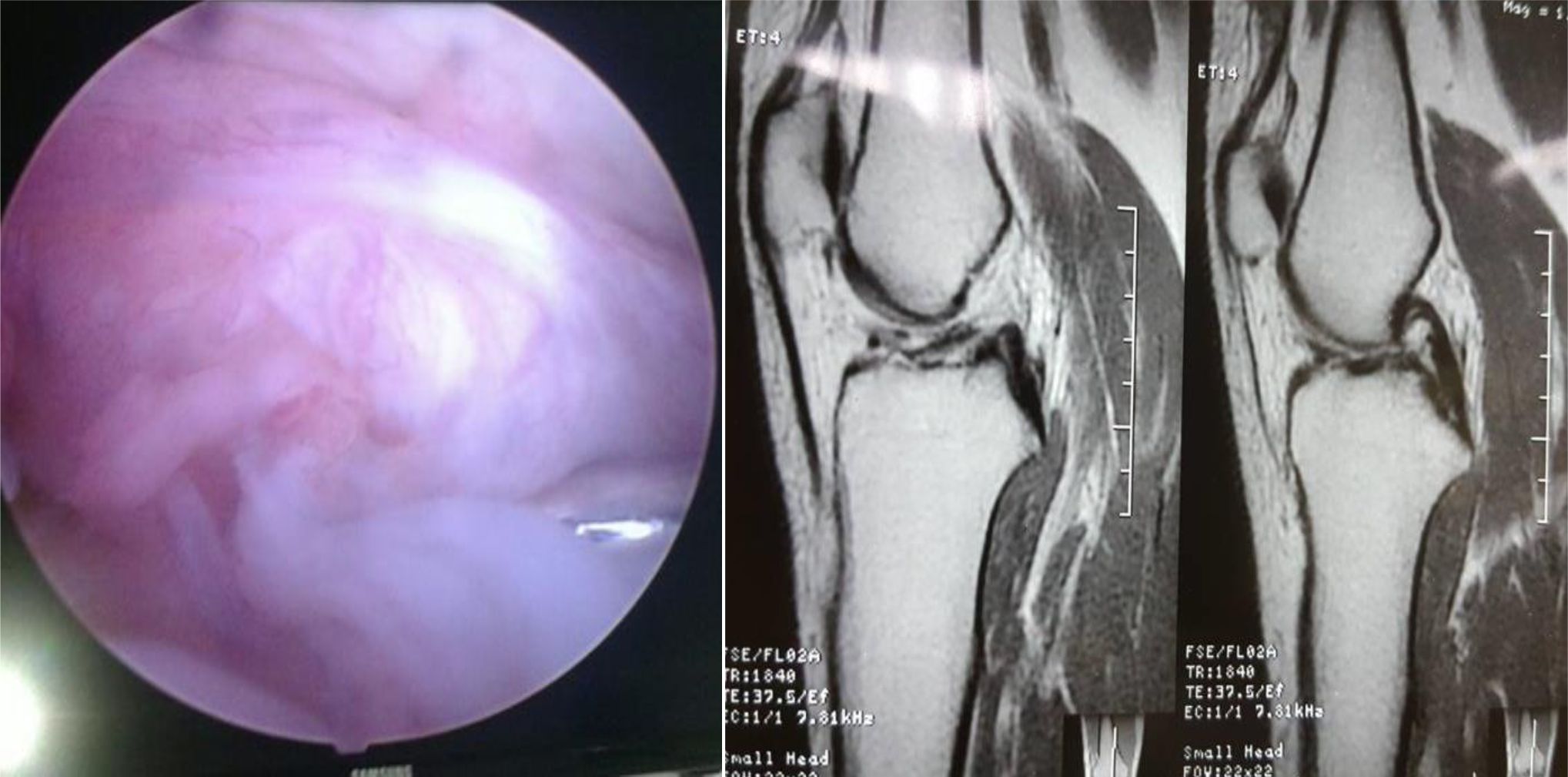
Figure 1. Arthroscopic and MRI image of 35 years-old-male having twist injury to right knee joint. Complete tear of ACL are shown in arthroscopy as well as MRI
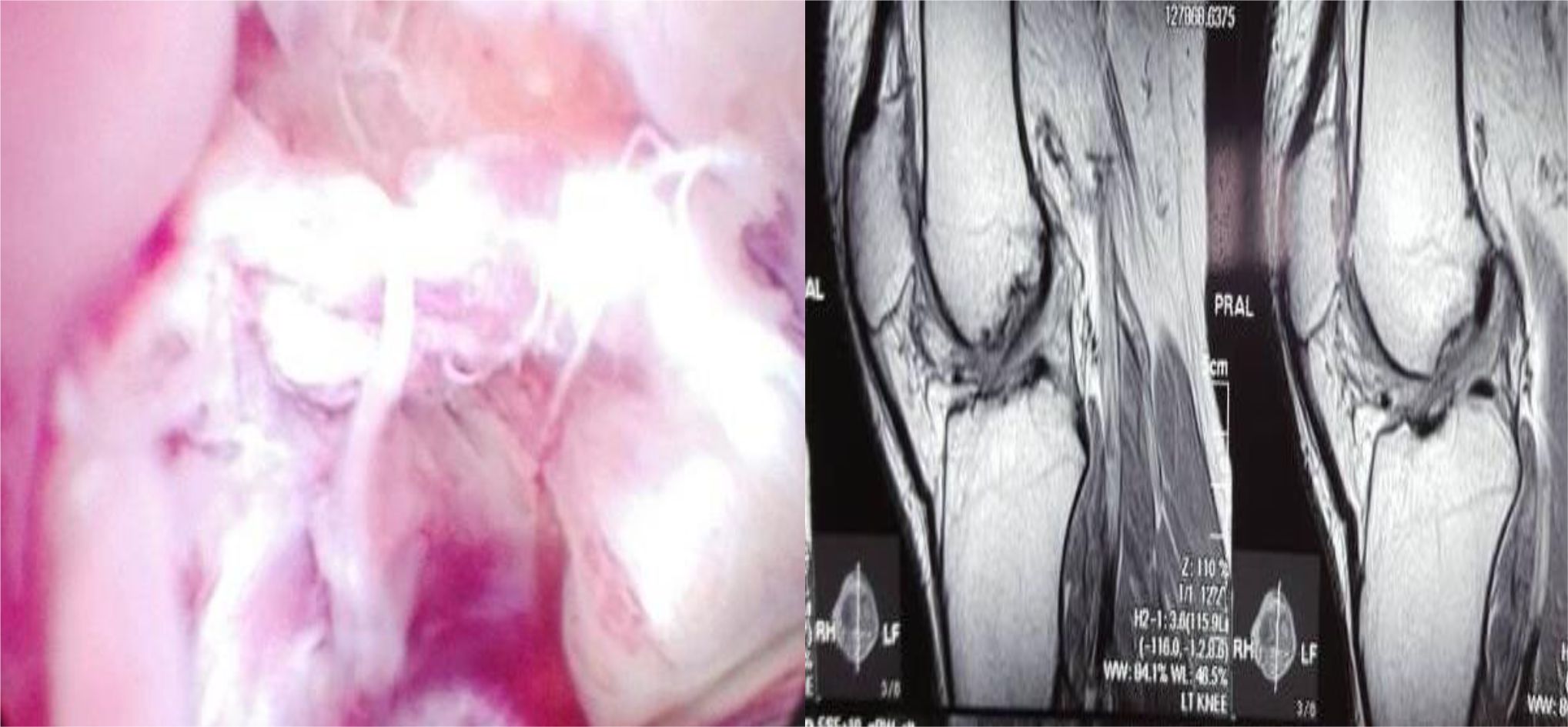
Figure 2. Arthroscopic and MRI image of 29 years-old-male had left knee injury during sports. There is complete ACL tear found on arthroscopy as well as MRI
DISCUSSION
MRI commonly uses modality to diagnose soft tissue injuries when other modalities fail to diagnose. It plays a vital role in diagnosing meniscal and ligamentous knee injuries. The knee often experiences injured joint due to its involvement in motion. It is complicated joint that includes multiple structures for support and stability. Cruciate ligaments, collateral ligaments and menisci provide stability during motion. The ACL commonly gets injured during sports and accidents. It can occur isolated or associated with menisci and other ligaments. The first diagnosis of ACL tear was made by Galin and Stark12 and the first intra articular ACL reconstruction was made by the father of ligamentoplasties i.e. Hey Groves.
The difference between acute and chronic injury as well as partial or full tear is difficult to define on clinical examination. Clinical examination has very low sensitivity and specificity. Ultrasonography is another modality for diagnosis of ACL tear. It has a high sensitivity and specificity but requires the hands of an expert.13 The advent of MRI technology in the early 1980s helped orthopedic surgeons in the treatment of knee disorders in several ways. In the early use of the technology, the improved initial diagnostic accuracy with preoperative MRI proved to be cost-effective in reducing unnecessary surgical interventions and altering treatment plans.14 The addition of oblique axial imaging to standard MR imaging improves diagnostic accuracy for detecting partial tears of the ACL as well as individual bundle tears of the ACL.15 3D MR imaging has the potential to allow surgeons to: (1) tailor an ACL reconstruction technique or graft choice based on the ACL footprint size, (2) plan for selective bundle ACL reconstruction for partial tears, and (3) preoperatively template tunnel position according to the patient’s individual anatomy.16 MRI has high accuracy for patients with complete ACL rupture. Due to the higher economic costs and increased complication risks of diagnostic arthroscopy, MRI is therefore recommended as the principal investigation following clinical examination, to diagnose ACL rupture.17 However, there are still controversies. According to Liodakis et al.18 the MRI scans are not routinely necessary as an indication for knee arthroscopy as clinical examination and plain radiograph are sufficient.
Our results showed that MRI had sensitivity and specificity of 93.33% and 85.71%. Similarly, the positive predictive value, the negative predictive value and accuracy are 96.55%, 75.0%, and 91.89%. Khan et al.19 concluded that MR had 100% sensitivity and NPV 0f 70% of diagnosing ACL tears in their study, which was higher than our findings. Clinical examination had sensitivity of 88% and NPV 75% in diagnosing ACL injuries. Gupta et al.20 found that MRI showed a sensitivity of 74.42%, specificity of 93.10%, accuracy of 84.21%, and a negative predictive value of 88.04%. These findings were almost similar to our findings. Thiga et al21 found that the sensitivity and specificity of MRI for anterior cruciate ligament rupture (whether complete or partial) was 83.3% and 90.9% respectively. Similarly, Similarly, Amr et al22 found that in comparison with knee arthroscopy, magnetic resonance imaging revealed an overall of 93.9% sensitivity and 66.6% specificity. Chiranjib et al.23 also found that the sensitivity of MRI for diagnosis of ACL was 87.5%, specificity was 66.67%, positive predictive value -87.5%, negative predictive value -66.6% and accuracy of 81.82%. Almost all of the studies discussed above yield almost similar findings with our study in that we are in favor of conducting MRI for diagnostic purposes. While arthroscopy should be restricted for therapeutic purpose, MRI is non-invasive and cost-effective compared to arthroscopy and should always be considered as an option of choice for diagnosing ACL injuries.
There are some limitations in our study. Firstly the findings were not compared with the findings from the clinical examinations. Moreover chronic injuries were excluded to reduce the bias. Therefore, further research needs to be carried out to yield different results.
In conclusion, MRI is highly accurate in the diagnosis of ACL injuries in traumatic knees. Arthroscopy should be considered when it is required as therapeutic. Diagnostic use of arthroscopy is limited in the presence of MRI. MRI is an appropriate screening tool for therapeutic arthroscopy, making diagnostic arthroscopy unnecessary in most patients.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Solomon L. Warwick D, Nayagam S. Apley’s system of orthopaedics and fractures. 9th edition. Imaging of knee. Bristol. UK;2010:553.
- Canale ST, Beaty JH. Campbell’s operative orthopaedics. 12th edition New York: Mosby; 2013:2133–6.
- Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39(12):1338–44.
- Muhle C, Ahn JM, Dieke C. Diagnoses of ACL and meniscal injuries: MR imaging of knee flexion versus extension compared to arthroscopy. Springerplus. 2013;2(1):213.
- Noyes F, Mooar P, Matthews D, Butler DL. The symptomatic anterior crucial deficient knee: Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983;65(2):154–62.
- Kostov H, Stojmenski S, Kostova E. Reliability assessment of arthroscopic findings versus MRI in ACL injuries of knee. Acta Inform Med. 2014;22(2):111–4.
- Cellar R, Sokol D, Lacko M, Štolfa Š, Gharaibeh A, Vaško G. Magnetic resonance imaging in the diagnosis of intraarticular lesions of the knee. Acta Chir Orthop Traumatol Cech. 2012;79(3):249–54.
- Sharma UK, Shrestha BK, Rijal S, Bijukachhe B, Barakoti R, Banskota B, et al. Clinical, MRI and arthoscopic correlation in internal derrangement of knee. Kathmandu Univ Med J. 2011;9(35):174–8.
- Siddiqui A, Ahmad I, Sabir AB, Ekram Ullah, Rizvi SA, RizvI SW. Clinical examination vs. MRI: evaluation of diagnostic accuracy in detecting ACL and meniscal injuries in comparison to arthroscopy. Pol Orthop Traumatol. 2013;78:59–63.
- Gupta S, Sharma R, Sachar R, Saini Y, Saini N. Comparison of clinical examination, MRI and arthroscopy in knee injuries. Internet J Orthop Surg. 2012;19(3):275–81.
- Stein V, Li L, Lo G, Guermazi A, Zhang Y, Kent Kwoh C, et al. Pattern of joint damage in persons with knee osteoarthritis and concomitant ACL tears. Rheumatol Int. 2012;32(5):1197–208.
- Leblanc M-C, Kowalczuk M, Andruszkiewicz N, Simunovic N, Farrokhyar F, Turnbull TL, et al. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2805–13.
- Palm H-G, Bergenthal G, Ehry P, Schwarz W, Schmidt R, Friemert B. Functional ultrasonography in the diagnosis of acute anterior cruciate ligament injuries: a field study. Knee. 2009;16(6):441–6.
- Milewski MD, Sanders TG, Miller MD. MRI-arthroscopy correlation: the knee. J Bone Joint Surg Am. 2011;93(18):1735–45.
- Ng AW, Griffith JF, Hung EH, Law KY, Yung PS. MRI diagnosis of ACL bundle tears: value of oblique axial imaging. Skeletal Radiol. 2013;42(2):209–17.
- Han Y, Kurzencwyg D, Hart A, Powell T, Martineau PA. Measuring the anterior cruciate ligament’s footprints by three-dimensional magnetic resonance imaging. Knee Surg Traumatol Arthrosc. 2012;20(5):986–95.
- Smith TO, Lewis M, Song F, Toms AP, Donell ST, Hing CB. The diagnostic accuracy of anterior cruciate ligament rupture using magnetic resonance imaging: a meta-analysis. Eur J Orthop Surgery Traumatol. 2012;22(4):315–26.
- Liodakis E, Hankemeier S, Jagodzinski M, Meller R, Krettek C, Brand J. The role of preoperative MRI in knee arthroscopy: a retrospective analysis of 2,000 patients. Knee Surgery Sports Traumatol Arthroscopy. 2009;17(9):1102–6.
- Khan HA, Ahad H, Sharma P, Bajaj P, Hassan N, Kamal Y. Correlation between magnetic resonance imaging and arthroscopic findings in the knee joint. Trauma Mon. 2015;20(1):e18635.
- Gupta K, Guleria M, Sandhu P, Galhotra R. Correlation of clinical, MRI and arthroscopic findings in diagnosing meniscus and ligament injuries at knee joint: A prospective study. J Orthop Allied Sci. 2013;1(1):2–6.
- Thiga L. Findings of magnetic resonance imaging of intra-articular knee pathology: Radioarthroscopic correlation. University of Nairobi, CHS, Kenya; 2008.
- Khalil AO, Resnick D, Zeid AF, Zaiton FM. The role of magnetic resonance musculoskeletal imaging in evaluation of sports injuries of the knee joint. Zagazig University Medical Journal. 2015;20(6).
- Murmu C, Tiwari P, Sircar S, Agrawal V. Accuracy of magnetic resonance imaging in diagnosis of knee injuries. Int J Orthop. 2017;3(1):85–8.
Copyright @ 2017 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id