Morbidity and mortality are still problems, especially in developing countries. These include not only infectious diseases, but also noninfectious or degenerative as well as re-emerging diseases. Various efforts have been made, such as improving access to health care, community empowerment and setting the millenium development goals and sustainable development goals, however these efforts are still not adequate. Additional strategies have been proposed and improved, such as standardization, accreditation, health policy reform, universal coverage reform, and strengthening health resources.1
Modern medical services need teamwork, which implies that it also requires individuals with leadership competency.2 Doctors who work at primary healthcare become the forefront in all efforts to ensure sustainable health management. In managing health problems, doctors must cooperate with various individuals, both medical and nonmedical, as well as patients and their families.3,4 In their role as care coordinators, doctors must experience the stages of planning, organization, implementation, and evaluation. All of these elements comprise part of an overall healthcare service system at a healthcare service facility or organization that calls for a clinical leadership competency and are expected to bring positive effects on the quality of the services provided.5
Healthcare system and primary care
The healthcare system consists of three levels. The first is the macro level, which is at the government/legislative level and consists of health policy and health investment policy, health finance system, standardization, continuing education, and intersector coordination. The second is the meso level, which is at the health facility level and consists of health service/patient’s flow, health provider expert, evidence-based and prevention-based medicine, information systems, and connection with community resources. The third is the micro level, which consists of patient empowerment and doctor-patient relationship. All levels of healthcare system will need leadership capacity, and this article will focus more on the micro level.5,6 There are also needs in primary care as written in Primary Health Care Now More Than Ever by World Health Organization (WHO).1 Primary health care needs to establish personcentered care, comprehensive and integrated responses as well as continuity of care, closer to people, responsible for a well identified population, organizing networks and primary care team as a hub of coordination.1,7–8
Care coordinator
One of a doctor’s roles in patient’s health management is to be a care coordinator.3 McDonald9 defines a care coordinator as an individual who is responsible for conducting activities related to patient’s health management which involves two or more participants (including the patients), in an organization, in order to improve the patient’s quality of life and the quality of health services.10 The definition emphasizes the need for doctors to establish cooperation with various individuals, including patients, families, and other healthcare providers in managing diseases. This principle is in line with democracy-based health development, which is performed in the spirit of partnership and inter-sector collaboration.11
The terms coordinator itself contains leadership elements. Leadership is an action, not position.12 Being a doctor means doing an action, not having a position. Why? Because it is the duty and functions of a doctor to motivate, engage, collaborate, and influence individuals’ as well as their behavior to live healthy. Therefore, it is in accordance with WHO five stars doctor as a community leader because naturally a doctor is a leader for the community and does something for the community, regardless their structural position.13,14
Some clinicians consider leadership skills as necessary only for those doctors in a formal management role, not as practitioners.15 In primary care case management, coordination is needed between doctor and patient / family, nurses, other health providers, or other activities unit, to solve the patient’s health problems. Therefore, primary care physicians should at least have the capability of interpersonal communication, inter-professional, teamwork, and clinical administration. These abilities are reflection of the clinical leadership competencies, with doctors as the center of health care services provider to patients and leading multidisciplinary healthcare teams.15,16
Coherence between transformational leadership and doctor-patient interaction
Tead17 defines leadership as a combination of various person’s behaviors to encourage others and be able to complete entrusted tasks. Bass and Avalio18 define transformational leadership as the leader’s efforts to transform the needs of followers to one level higher. Through transformational leadership, followers can achieve performance exceeding their leader’s expectations. This theory is based on the idea that innovative, inspirational, and proactive leaders have the ability to motivate others and to pursue high standards and long-term goals.12 The transformational leader realizes that empowerment, communication, strong values, and mutual respect are the most important things to improve quality. In medicine, the transformational leadership type is more suitable because doctor-patient relationship is a dynamic, trust, and voluntary relationship. There is also internal motivation from patients and doctors to communicate with each other, and doctors should also have charisma, inspire, as well as be proactive in serving patients.19
The values of transformational leadership and value-based diagnostics are central to the clinical leadership development program. Clinical leadership is the leadership from physicians and by physicians, to initiate and implement changes, aimed to reach patient management target. The role of physicians in clinical leadership is to determine the direction, management of resources, and motivation while maintaining the clinical role. Therefore, clinical leadership is integrated into daily medical practice and become part of the clinical role because they are directly involved in health care to patients.19,16 National Health System United Kingdom20 divides the clinical leadership competence framework into five dimensions: Demonstrating personal qualities, working with others, managing services, improving services, and setting direction. By applying these five dimensions, it is hoped that a practicing physician, especially a primary care physician, is able to have self-directed development, build networks, make plan and manage resources, innovate, as well as contribute to the improvement of healthcare service based on evidence.20
The essential role of a doctor is to create a healthy and productive people. In order to achieve this goal, the doctor needs to work together with various people who share the same vision and mission, give positive influence to each other, and be willing to motivate each other. Such image is in accordance with the ideal practices of transformational leadership among doctors at all levels, from the micro level to the macro level. All efforts to create a healthy society must be supported by policies and facilities, which can assist doctors in fulfilling their duties.
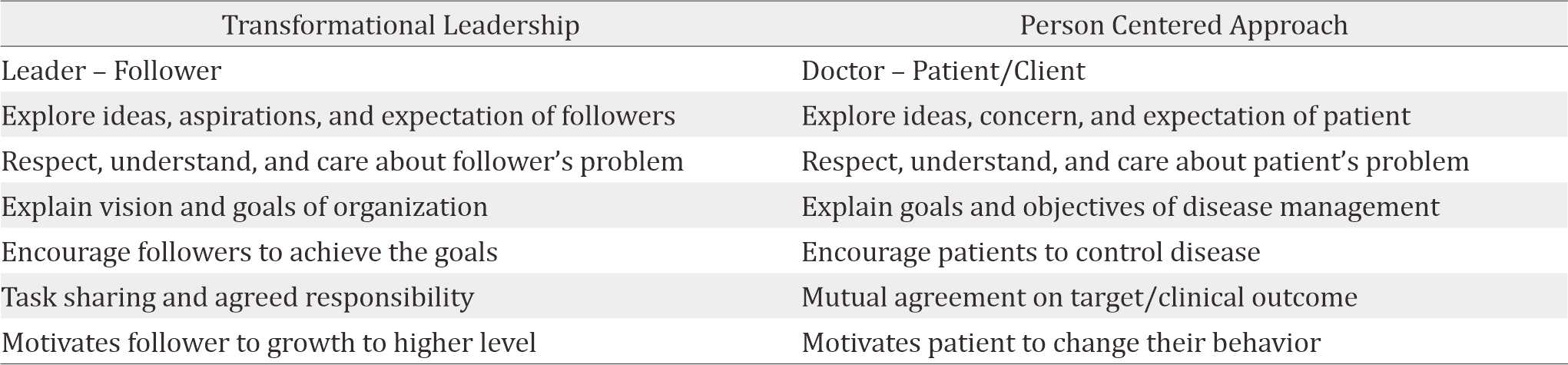
There is a term in family medicine called a patientcentered approach. There is a relationship between a leader and his followers in leadership that is similar to the relationship between a physician and his patient. One characteristic of transformational leadership is the ability to explore ideas, concerns, and expectations of followers. It is identical to a patient-centered approach, where the doctors need to explore the ideas, concerns, and expectations of patients. Both leaders and doctors should respect, understand and care about their followers or patients’ problems. The transformational leader explains the vision and goals of the organization and encourage followers to achieve organizational goals together by sharing tasks and agreed responsibilities. On the other side, doctors are also expected to explain the goals and objectives of treatment and to encourage patients to control the disease together with mutually agreed target/clinical outcome. A transformational leader motivates followers to reach a higher level. It is identical to the task of motivating patients to change their behavior to become healthier. Such is the resemblance between transformational leadership and a patient-centered approach (Table 1).16,19,21
Table 1. Transformational leadership and patient centered approach
A doctor as the leader and implementation in doctor-patient relationship
In fulfilling the duties, a leader must take several aspects in the management process for the purpose of designing the activities, which need to be performed in order to achieve the team’s common goals. A doctor can also apply the same management process when designing the treatment and intervention, which need to be performed to achieve the targets, related to the patient’s health management. The process starts from planning up to creating a professional network, as described in Figure 1.
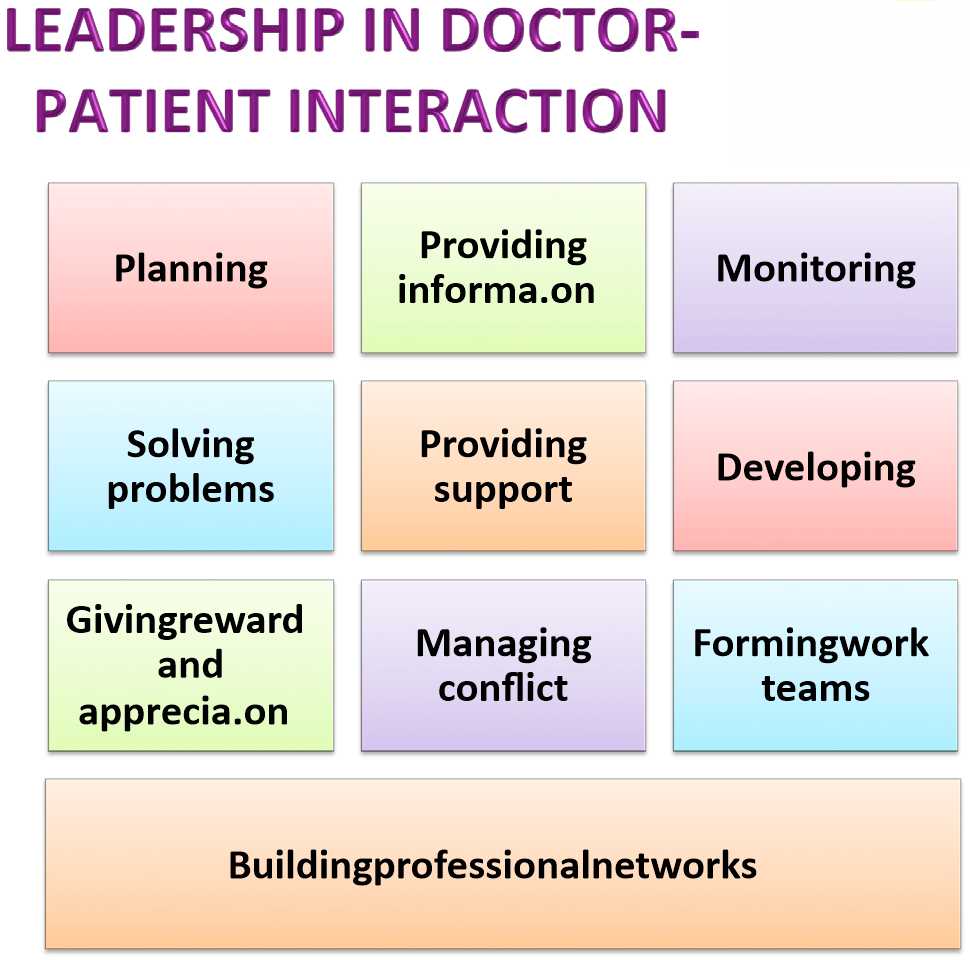
Figure 1. Leadership in Doctor – Patient Relationship
Planning
Planning is defined as a systematic activity to identify and specify the goals of a project, the set of actions that need to be taken to achieve the goals, the steps that need to be taken, the methods of implementation, and the human resources that need to be employed to perform the actions to achieve the goals. Planning must be performed in an integral, holistic, and meticulous manner; must ensure a unity of understanding, attitude, and course of action; and must be followed up by concrete actions. Planning covers a number of specific activities consisting of identifying the types of activity, determining the priority scale, preparing time and cost estimates, appointing the individuals in charge of each activity, distributing jobs, and stating the procedures for evaluation.22
In daily practice, the doctor would normally design a disease management plan according to the anamnesis, physical examination, and supporting examinations by applying a systematic process of thinking and careful establishment of a diagnosis. This principle must be adopted so that the doctor and the patient can perform the planned activities more effectively to achieve their common goals of solving the patient’s health problems. The entire planning process must be documented by medical information system, accessible to all individuals involved.
Providing information
Information gives intensification to exchanges of ideas, opinions, and thoughts related to the decisions and policies taken to solve problems. This process requires the commitment of all parties involved and comprehensive information from the leader. The process of information exchange must be performed in two directions.22 This kind of approach is expected to take place in a doctor-patient relationship. The interpersonal relationship between doctor and patient is similar to between leader and follower, which generates specific communication patterns of doctorpatient relationship. A doctor needs to devise an effective pattern of communication with the patient and other individuals involved, achieving a unity of vision and mission in their determined effort to cure the patients’ health problem.
Any plan for health management must specify the roles and duties of all individuals involved in the process including the doctor, nurses, other healthcare providers, patient, family members, and community (if required). The doctor, who leads the whole process of information exchange, selects the right model of information exchange. Communication failure often leads to misunderstandings, inflicts losses, and even leads to disastrous effects. Such consequences can and actually occur in daily medical practices in various forms, such as allegations of malpractice even in a situation where the doctor has followed applicable professional standards.
Monitoring
Monitoring is one of a leader’s duties, which involves assessment and correction to make sure that the common goals can be achieved effectively. Monitoring can be done both internally and externally. Internal monitoring consists of identifying indicators of success, examining the key success factors, raising specific questions, which are related to performance, encouraging team members to report any problems, and learning from failures. External monitoring consists of identifying customers’ needs based on situational changes, involving customers in information search, observing various events relevant to mutual goals, and learning from other people’s successes.22
In cases of daily patient’s management, a doctor needs to continuously gather relevant data and regularly evaluate the extent to which the treatments and interventions have been able to cure the patient’s health problems according to the set plan. A medical information system is required to record the data and the subsequent intervention plans by taking into account the patient’s current development. The results can be used for improving the quality of both short-term and long-term healthcare services.
Solving problems
A good leadership involves the ability to make various decisions, solve problems, take actions, employ various resources, and produce and adopt policies as solutions for certain problems. In order to achieve the goal, the leader and the followers must sit together and make decisions, which serve the interests of the organization, as well as the needs of the subordinates. Before a decision is made, both parties must consider all possible risks and identify the best solution whose performance will be part of the leader’s responsibility.22
The same analogy also applies to the doctor’s duty to cure the patient’s health problem. Before making any clinical decisions about the patient’s health problem, the doctor must consider all information, which has been gathered from many resources for the best interest of the patient. Any discussions which take place between the doctor and the patient before decision making is comparable to a counseling session in which the doctor invites the patient, along with their family when needed, to make a decision together in order to solve the problems at hand by considering the patient’s preferences.
Providing support
Providing support is one of the expected duties of a leader as the reflection of consideration, acceptance, care, and concern for the followers. It is important for a leader to treat others with politeness, to show genuine concern, to be patient and helpful, to provide support when somebody is confused and distraught, to pay attention to followers’ complaints and problems, and to identify and maximize their potentials.22
A doctor must also show the same qualities to his or her patients. When interacting with a patient, the doctor is expected to actively listen to the patient’s complaints, show empathy, give support, and work together with the patient to solve the problem while at the same time identifying the potentials or resources, which can be employed to solve the problem.
Developing
This aspect is defined as the process of enhancing an individual’s knowledge, skills and capabilities which can improve performance both at present and in the future. Development can be gained from training, coaching, mentoring, and counseling. A leader must be able to select the most suitable forms of development according to the actions that will be taken, and the achieve target. There are several factors that need to be considered in terms of development, such as the need for development, the motivation for capacity building, the method for development and the procedures for evaluation.22
In a doctor-patient relationship, the doctor has an obligation to provide education, knowledge, counsel and coaching for individual patients, their families and the larger society as a form of capacity building. Such attempts must be undertaken to empower and enable the people to address their own health problems under the doctor’s supervision and his or her medical team.
Giving rewards and appreciation
Giving rewards is defined as an action of giving praise or showing appreciation to a component of an organization that has achieved a certain level of effective performance. An acknowledgment from the leader will enhance motivation and strengthen the commitment to achieve common goals. A reward or appreciation may take concrete forms such as a raise in salary or job promotion.22
In daily interaction between a doctor and a patient, when the patient has reached a certain target (such as when the patient has been able to maintain his or her glucose level or blood pressure or when the complaints have been eased), the doctor can appreciate the patient’s commitment to follow the intervention scheme as planned before. In addition to praise, the doctor may also inform the patient about the benefits which the patient has gained or will gain from achieving a certain target. One of the greatest challenges in the medical world is to ensure long-term benefits of an intervention (such as disappearance of relapses, withdrawal of symptoms, or an absence of complications), which may not be immediately observed. As such, the patient must be continuously supported and encouraged to take the necessary measures to prevent relapses. The point is that the patients will be really motivated and feel the need to maintain their own health if they realize and know the benefits or have experienced the benefits themselves.
Managing conflicts
Conflicts may arise from the way an individual interprets, perceives, and responds to the environment. Another source of conflicts is lack of coordination among members of a team in terms of interdependence, confusion because of unstructured job descriptions, differences in task orientations, and a weak control system. A conflict may also take the form of a monotonous working environment, which will lead to excessive apathy if left unaddressed.22
Beside communication problems, another type of conflict that may arise in a doctor-patient relationship is an apathetic attitude of the patient that may arise when the problems persist and do not show any sign of improvement. This apathy might drive the patient to do things, which deviate from the agreed plan. Such conflicts may also arise when the patient is not well informed, does not know exactly what to do, or does not realize the consequences of doing things that are not supposed to be done because the doctor does not give a clear or detailed explanation. In order to avoid this type of conflict, there must be a clear distribution of duties and responsibilities between the doctor and the patient. Furthermore, the doctor must have sufficient knowledge and skills in predicting various possible scenarios, so that a more effective prevention and monitoring scheme can be prepared.
Forming work teams
This team might consist of several individuals or smaller teams, each of which possesses complementary skills and is strongly committed to achieve common goals. Each of them must also be equipped with a set of techniques, approaches, and orientations that are solidly based on scientific theories recognized and applicable in their respective fields. A leader’s duty to form a work team is also related to conflict management, because one of the ways to manage conflicts in a constructive way is by forming a solid work team.22
In order to provide high-quality medical services at a healthcare facility, a professional service team should be formed, which consists of doctors, nurses, pharmacists, nutritionists, and other healthcare providers. The team’s job is to cure patients’ health problems in an integrated way, according to the targets set for each individual patient. It is hoped that all elements within the team would support and complement each other for the best interest of the patients under the coordination of a doctor who is authorized to make clinical decisions if any clinical problems should occur. There must also be clear job distribution and procedures, which are mutually agreed and will be carried out together by all components of the team.
Building professional networks
As globalization continues to expand, the need for building networks has become more urgent. This current situation stimulates the development of an intensive communication network that “shrinks” the world. Building professional networks is associated with a variety of behaviors, which aims to enhance both the internal and external potentials of an organization. A leader must develop the awareness and sensitivity to various needs by taking into account of the available opportunities and the stakeholders interests.22 In the context of doctor-patient interaction and healthcare services, the doctor and healthcare team, who have to deal with patients personally, must be aware of and sensitive to the patients’ needs in order to build both internal and external professional networks in a healthcare facility. By establishing professional networks, the otherwise inaccessible important external information can be made more accessible to all parties involved in order to ensure information accuracy and appropriate interventions. Establishing cooperation with a specialist or building networks among healthcare facilities, are other ways to build professional networks for the benefit of the patients.
Care coordination model
Case management in primary care requires medical staff team as care coordinator who work and discuss case/health service issue, clarify each other task, contributes each other, and improve team building. Besides working among health professionals and patients, care coordinator also works closely with families and specialists for the benefit of patients. Case management assessment in a holistic (bio-psycho-socio-cultural approach), comprehensive (preventive oriented), integrated, and continuum are reported to head of health facility in a periodic meetings to identify issues that need to be changed/ updated/clarified according to the needs of patients. As a form of social responsibility or expanding services, the care coordinator team can provide guidance to specific communities as well as identifying the resources that are useful to patients. This model will enhance creativity, closeness, satisfaction, commitment, concern for others, involved in determining the direction of the healthcare, and enhance self-leadership. It requires the support of meso-level management, information systems, and strengthening the leadership capacity of primary care physicians (Figure 2).
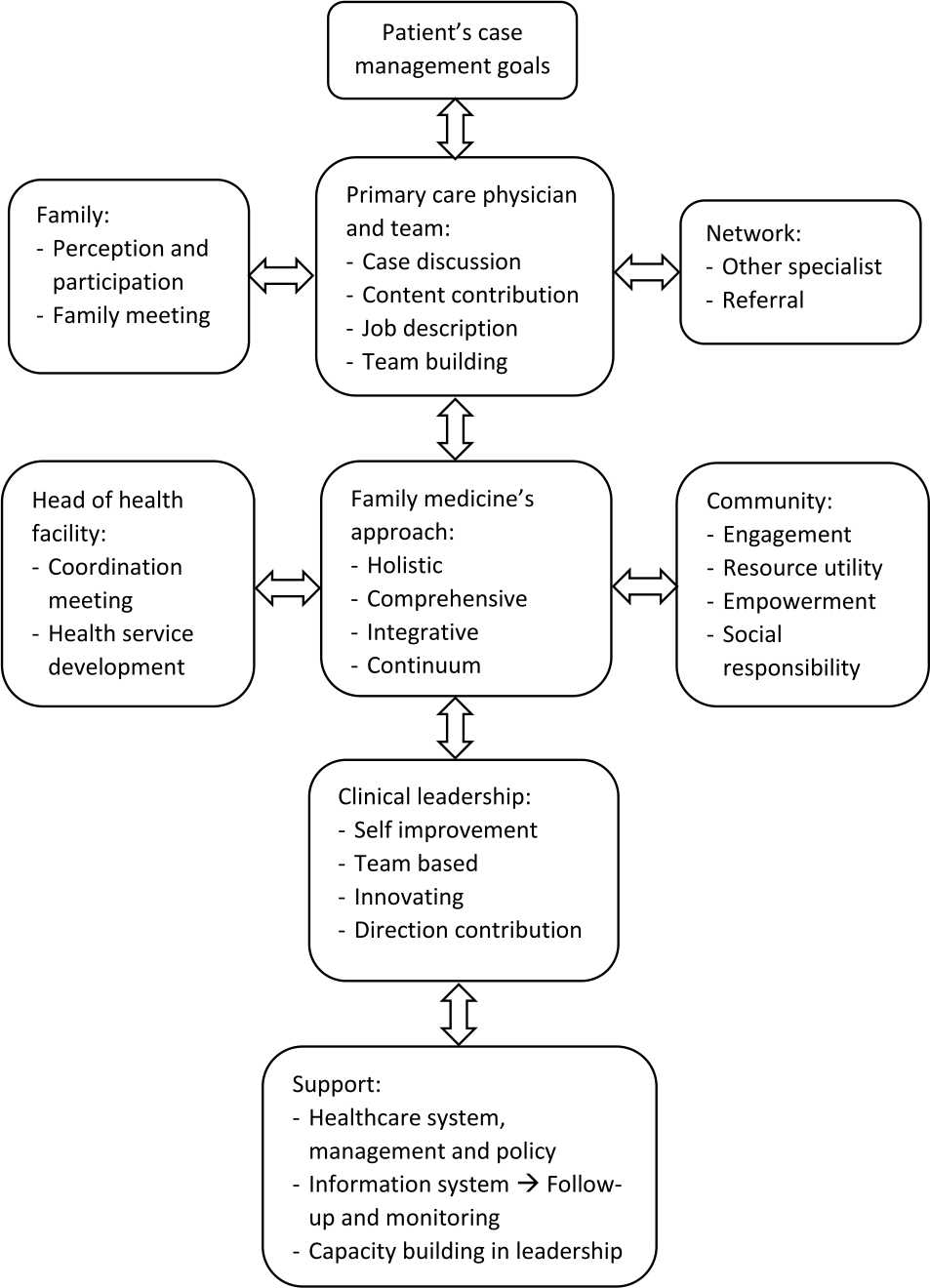
Figure 2. Care coordination model in primary care
Function of primary care doctors as care coordinators can be improved by increasing the implementation of interdisciplinary services, strengthening the capacity of primary care physicians and exposure to manage interdisciplinary team, clarifying the service flow, job desk and responsibilities of each member of the health team, and improving information systems that can be accessed quickly and processed longitudinally to evaluate management goals.
Being a care coordinator is also beneficial as an involvement to determine the direction of service through regular meetings with fellow physicians for case discussions, making clinical guides, new standards or revisions according to current conditions, regular meetings with the head of the health facility to discuss patients’ complaints or to fix service flow and strengthening the role of each health provider involved, as well as regular meetings with management to deliver new/ revised management guidelines and advocate why it needs policy/rule change. Therefore, the doctor will needs diplomacy skills, influence, leadership and effective communication capacities.
Activities such as regular meetings to discuss cases/patient’s complaints, contributions to educational materials creation, guidelines, service flow, or other written guidance, develop recording/integrated data processing in order to avoid overlapping of recording/questions, and team building to develop agreed activities and monitor together, will increase creativity and relationship. This will enhance the relationship among team member that will impact on patient’s outcome.
The doctor plays complex roles as a practitioner, a colleague, and a leader for his or her patient, as well a link to the healthcare services management. Therefore, the ideal doctor needs to have a wide range of exposure to professional experiences, so that he or she would be able to understand the relationship between practical experiences (practical management) and healthcare services management (organizational management). Such exposure to various experiences can be attained by enhancing doctors’ capacity and competency in organizational behaviors, as well as their application to patient case management. This action may help health service reform based on patient needs by applying holistic, comprehensive, integrated, and continuous case management, as well as strengthening relationships by employing various resources for the best interest of the patient. This experiential exposure can be provided within the framework of a structured formal education for doctors who wish to work as practitioners and leaders as the forefront of high quality healthcare services, especially in primary healthcare.15
In conclusion, the doctor is expected to have two kinds of competencies: clinical leadership and transformational leadership, which can support their performance as the patient’s care coordinators and to ensure the continuation of services which cannot be performed by a single individual only. Care coordinators and clinical leadership will meet primary care needs as well as support to WHO primary health care reform. By having formal education/training on leadership competence, having a care coordinator in primary care with leadership spirit and competence, doing periodic evaluation, giving constructive feedback, solid teamwork, cooperation with the patient, family, community and other health workers, as well as networking, hopefully will improve the patient, family, and community’s quality of life.
Conflicts of Interest
There was no conflict of interest for this paper.
Acknowledgment
The writer would like to thank dr. Muchtaruddin Mansyur, MS, SpOk, PhD, Dr. dr. Astrid W. Sulistomo, MPH, SpOk, Dr. dr. Herqutanto, MPH, MARS, Dr. Wirawan, MSL, MM, MSi, Dr. Ekowati Rahajeng, SKM, M.Kes, and Prof. Dr. dr. KRT. Adi Heru Sutomo, MSc.
REFERENCES
- Chan M. WHO The World Health Report 2008 - Primary Health Care (Now More Than Ever). Geneva; 2008. p. 9–19.
- Wattis J, Stephen C. Practical Management and Leadership for Doctors. London: Radcliffe Publishing Ltd; 2011. p. 1–10.
- McWhinney IR, Freeman T. Principles of Family Medicine. Textbook of Family Medicine. 3rd ed. Oxford: Oxford University Press; 2009. p. 13–29.
- McDaniel S, Campbell T, Hepworth J, Lorenz A. Basic Premises of Family Oriented Primary Care. Family Oriented Primary Care. 3rd ed. United States of America: Springer Publishing Company; 2013. p. 1–14.
- Bohmer R. The Instrumental Value of Medical Leadership: Engaging Doctors in Improving Services. London: The King’s Fund; 2012. p. 6–8.
- Pruitt S, Annandale S, Jordan-Epping J, Diaz J, Khan M, A K. Innovative Care for Chronic Conditions. 2002. p. 30–38.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502.
- O’Malley AS, Tynan A, Cohen GR, Kemper N, Davis MM. Coordination of Care by Primary Care Practices: Strategies, Lessons, and Implications. Cent Stud Heal Syst Chang. 2009;12:1–16.
- McDonald KM, Schultz E, Albin L, Noelle P, Lonhart J, Sundaram V, et al. Care Coordination Measures Atlas. 2010. p. 4–10.
- Meyers D, Peikes D, Genevro J, Peterson G, Taylor EF, Lake T, et al. The Roles of Patient-Centered Medical Homes and Accountable Care Organizations in Coordinating Patient. 2010. p. 1–9.
- Undang-Undang Republik Indonesia no 17 tahun 2007. Rencana Pembangunan Jangka Panjang Nasional. 2007. Indonesian.
- Wirawan. Kepemimpinan: Teori, Psikologi, Perilaku Organisasi, Aplikasi dan Penelitian. 1st ed. Jakarta: Rajagrafindo Persada; 2013. p. 103–150.
- Boelen C. The Five-Star Doctor: An asset to health care reform? Geneva; 2000. p. 1–13.
- Azwar A. Pengantar Administrasi Kesehatan. 3rd ed. Jakarta: Binarupa Aksara; 1996. p. 306–07. Indonesian.
- www.careers.bmj.com [Internet]. Doctors as Leaders. BMJ Careers. [updated Oct 2012; cited 2016 Jan] Available from: http://careers.bmj.com/careers/ advice/view-article.html?id=20009282.
- Swanwick T, McKimm J. ABC of Clinical Leadership. West Sussex: Wiley-Blackwell; 2011. p. 1–13.
- Azwar A. Pengantar Administrasi Kesehatan. Jakarta: Binarupa Aksara; 1996. p. 304–05. Indonesian.
- www.mlq.com.au [Internet]. Multifactor Leadership Questionnaire. [updated 1995; cited 2016 Feb] Available from: http://www.mlq.com.au/Products/ MLQ_Products_and_Services.pdf.
- Edmonstone J. Clinical Leadership Development. 1st ed. Edmonstone J, editor. Chicester, West Sussex: Kingsham Press; 2005. p. 232–380.
- National Health System Leadership Academy. Clinical Leadership Competency Framework; 2012. p. 6–7.
- Stewart M, Brown JB, Weston WW, McWhinney IR, William CL, Freeman TR. Patient Centered in Clinical Medicine: Transforming The Clinical Method. Oxford: Radcliffe Publishing Ltd; 2006. p. 60–65.
- Setiawan B, Muhith A. Transformastional Leadership: Ilustrasi di Bidang Organisasi Pendidikan. 1st ed. Jakarta: Rajagrafindo Persada; 2013. p. 50–70. Indonesian.
