
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
Warning sign as a predictor of dengue infection severity in children
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v27i2.2200 Med J Indones. 2018;27:101–7
Received: August 10, 2017
Accepted: June 5, 2018
Author affiliation:
Department of Pediatrics, Faculty of Medicine, Universitas Sumatera Utara, H. Adam Malik General Hospital, Medan, Indonesia
Corresponding author:
Ayodhia P. Pasaribu
E-mail: ayodhia_pitaloka@yahoo.com
Background
Dengue has emerged as a global public health problem, about 500,000 affected patients of 50–100 million cases will develop severe dengue infection. Therefore, early identification of severe dengue infection symptoms can save a patient’s life. The 2009 WHO dengue infection classification proposed seven warning signs to identify the risk of severe dengue. This study was conducted to predict the severity of dengue infection based on the number of warning signs.
Methods
This was a diagnostic study conducted with a retrospective analytic observation of patients admitted to Adam Malik hospital with a diagnosis of dengue infection from January 2014–May 2016. The association between warning signs and severe dengue infection was analyzed using logistic regression. We also analyzed the sensitivity, specificity, positive predictive value and negative predictive value.
Results
Of 140 patients who fulfilled the research criteria were collected from the medical records. The patients were classified as severe dengue (n=28) and nonsevere dengue (n =112). The warning signs that were associated with severe dengue were persistent vomiting (p<0.05, OR 31.9, 95%CI), fluid accumulation (p<0.05, OR 22.4, 95%CI), mucosal bleeding (p<0.05, OR 9.1, 95%CI), lethargy (p<0.05, OR 43.1, 95%CI). After analyzing the diagnostic tests, the combination of three or more warning signs showed that sensitivity of 92.9%, specificity of 78.6%, positive predictive value of 52%, negative predictive value of 97.7% was found to be associated with a severe dengue infection.
Conclusion
The combination of three or more warning signs showed a high sensitivity and specificity for predicting a severe dengue infection.
Keywords
dengue infection, prediction, warning sign
Dengue infection has emerged as a worldwide public health problem. It has been estimated that of 50–100 million patients with dengue infection, and approximately 500,000 patients would develop severe dengue infection requiring hospital treatment. Dengue infection frequently affects children, causing death in 2.5% of them.1 It has been reported that of 65,725 patients with dengue hemorrhagic fever (DHF), and 597 had died in Indonesia in the year 2011.2 In North Sumatera, the number of patients with dengue was 4367, with an incidence rate of 33 per 100,000 population in 2012.3
Several diagnostic examinations are available for diagnosing dengue infection; however, predicting the outcome of the infection remains a challenge for clinicians. Early identification of several symptoms that can predict severe dengue (SD) infection can save patients’ life through early treatment of the disease and more intensive monitoring.4 In 2009, the World Health Organization (WHO) revised the classification of dengue infection and proposed seven warning signs that can be used to identify whether the infection is at risk of SD infection.5,6 The warning signs indicating a potentially SD infection consist of abdominal pain, persistent vomiting, clinical fluid accumulation, mucosal bleeding, lethargy, hepatomegaly, and increased hematocrit with a decreased platelet count.4,7,8 These warning signs were found to have practical value in the next case management of dengue infection.4
Several studies conducted in Indonesia, especially in children, have determined the factors, signs, and predictors responsible for causing SD.9,10 However, those were not diagnostic studies and thus did not assess the seven warning signs that were suggested by the 2009 WHO guidelines as the dependent variable to identify patients at risk of SD. This study was conducted to predict the severity of dengue infection in children according to the number of warning signs.
METHODS
Study design and sample
A diagnostic study was developed by collecting secondary data from the medical records of patients who were diagnosed with dengue infection based on International Classification of Diseases (ICD) 10 from January 2014 to May 2016 at H. Adam Malik General Hospital. The inclusion criteria were as follows: children aged <18 years who were diagnosed with either dengue fever, DHF, or dengue shock syndrome; serological confirmation of IgG and IgM anti-dengue and/ or NS1 antibody; and a complete medical record. Patients with hematologic disease or malignancy and treatment history of consuming drugs that suppress bone marrow were excluded. The minimal sample size sufficient for statistical analysis was 140 children, with an alpha value of 5% (0.05) and a power of 95% (0.95%). This study was approved by Health Research Ethical Committe Faculty of Medicine Universitas Sumatera Utara/H Adam Malik General Hospital with number 254/KOMET/USU/2016.
Data collection procedure
Data were collected from the medical records included age, sex, nutritional status, clinical symptoms, including body temperature (axillary), duration of fever, headache, joint pain, retro-orbital pain, skin redness, petechiae, shortness of breath, abdominal pain, nausea, vomiting, persistent vomiting, edema, ascites, mucosal bleeding, severe bleeding, awareness, liver enlargement, signs of shock, positive tourniquet test, blood pressure, hematocrit, platelet count, leukocyte count, aspartate aminotransferase (AST) or alanine aminotransferase (ALT) > 1000 IU/l level, impaired organs such as heart and kidneys, and results of chest X-ray and abdominal ultrasound. Subjects were grouped into SD and nonsevere dengue (NSD) based on the 2009 WHO classification. Severe dengue infection symptoms were severe plasma leakage (shock, fluid accumulation with respiratory distress), severe bleeding, and severe organ disorders such liver (ALT and AST ≥1000 IU/l), CNS (impaired consciousness), heart, and other organs.
Warning signs
The following definitions were used for each of the warning signs. Abdominal pain was defined as abdominal tenderness and continuous pain (not intermittent), diffuse on some occasions. Persistent vomiting was defined as more than three episodes of vomiting in 12 h. Fluid accumulation was defined based on a pleural effusion and clinically diagnosed ascites, confirmed by an imaging study (ultrasound for ascites, gallbladder wall thickening, and pleural effusion, and/or X-ray for pleural effusion). Mucosal bleeding was defined as bleeding gums or conjunctiva; epistaxis; vaginal bleeding; bleeding from the digestive, respiratory, or urinary system (kidneys). Mucosal bleeding was defined as that from the respiratory, vaginal, digestive, conjunctival, and the urinary tract. Lethargy was evaluated as an alteration of consciousness with a Glasgow score of <15 or a Blantyre score of <5. Hepatomegaly was defined based on the liver edge palpation (done by a clinician) of >2 cm below the costal margin. Increased hematocrit was defined as concurrent with a rapid decrease in platelet count together with a decrease of 10,000 platelets/mm3 in 24 h with respect to previous measurement or concurrent with a platelet count of 100,000 cells/mm3.8
Statistical analysis
The data were entered, processed, and analyzed using SPSS version 17.0. The analysis involved calculation of sensitivity, specificity, positive predictive value, and negative predictive value of warning signs to detect SD and NSD. Logistic regression and receiver operating characteristic (ROC) curve were used to assess sensitivity and specificity. Chi-square test or Fisher’s exact test was used to compare the differences between the two groups, as appropriate.
RESULTS
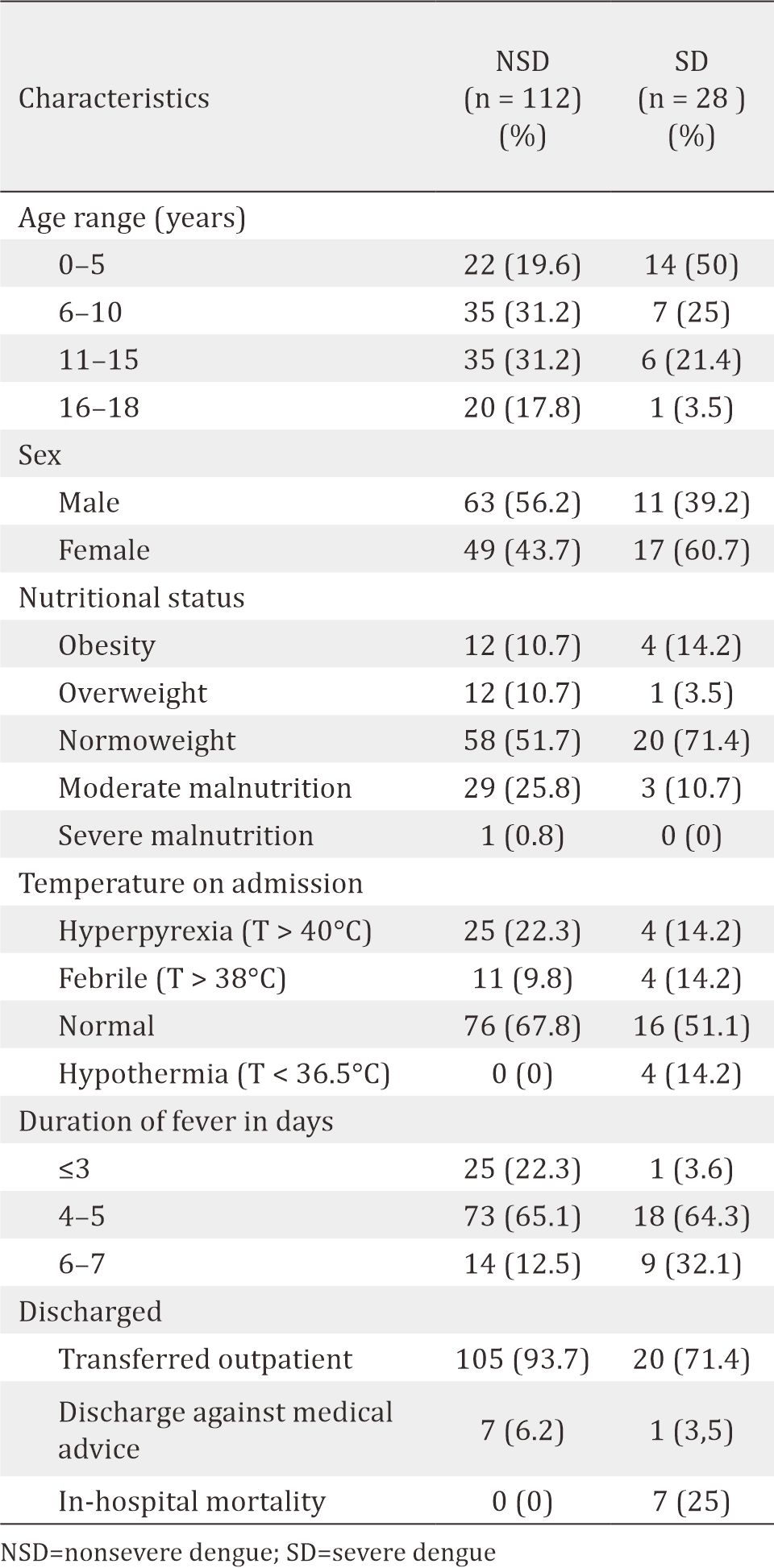
The data of 199 medical records of patients diagnosed with dengue infection from January 2014 to May 2016 met the ICD 10 criteria (A90-dengue fever, A91-DHF A91, A910-dengue with shock). After selection, 140 samples were found to fulfill both the inclusion and exclusion criteria. Of these samples, there were 28 (20%) with SD infection as shown in table 1.
Table 1. Characteristics of subjects
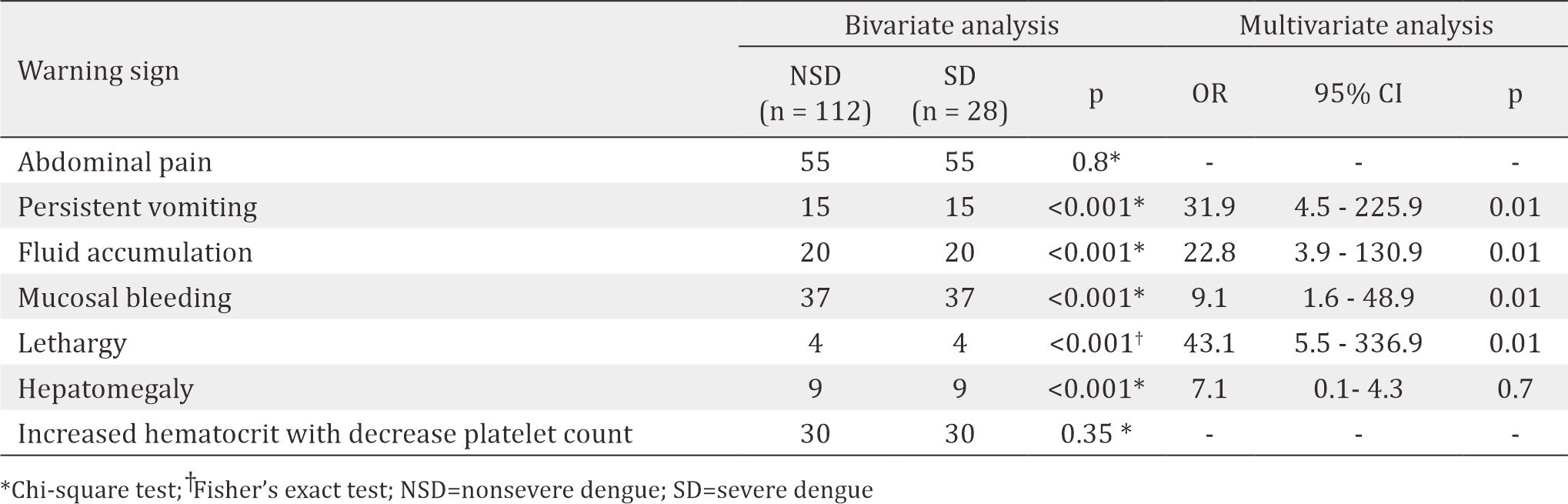
As shown in Table 2, the warning signs, including persistent vomiting, clinical fluid accumulation, mucosal bleeding, lethargy, and hepatomegaly, were significantly associated with SD according to the bivariate analysis. In the multivariate analysis, persistent vomiting, clinical fluid accumulation, mucosal bleeding, and lethargy were found to be significantly associated with SD.
Table 2. Bivariate and multivariate analyses of warning signs with the severity of dengue infection
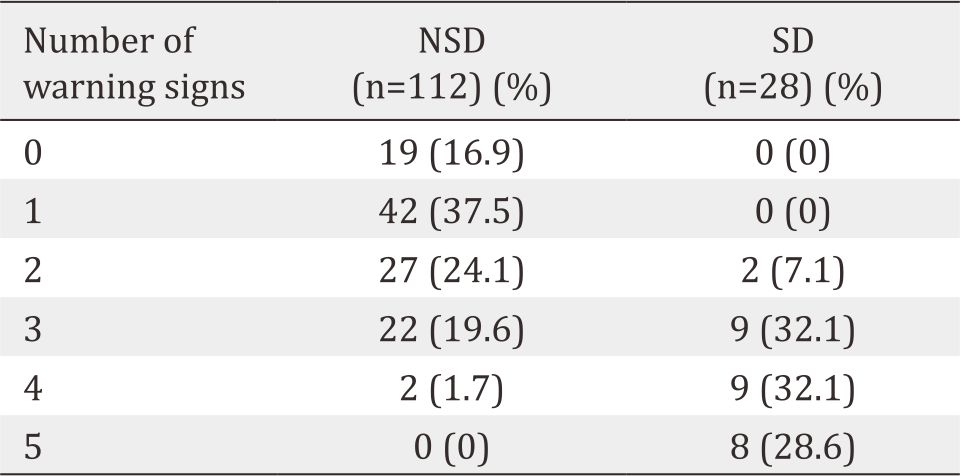
Although only four of five variables showed statistical significance, we included all five in the analysis to assess whether the combination of these variables performed well in diagnosing SD. Table 3 shows that the combination of the three, four, and five warning signs resulted in the diagnostic probabilities of SD infection of 32.1%, 64.3%, and 92.8%, respectively.
Table 3. The number of warning signs for diagnosing the severity of dengue infection
The ROC curve depicted in figure 1 shows the area under the curve (AUC) of three warning signs that performed well in detecting SD infection. The sensitivity of AUC was 92.9%, with a specificity of 78.6%, a positive predictive value of 52%, a negative predictive value of 97.7%, a positive likelihood ratio of 4.31, and a negative likelihood ratio of 0.09 in three or more warning signs.
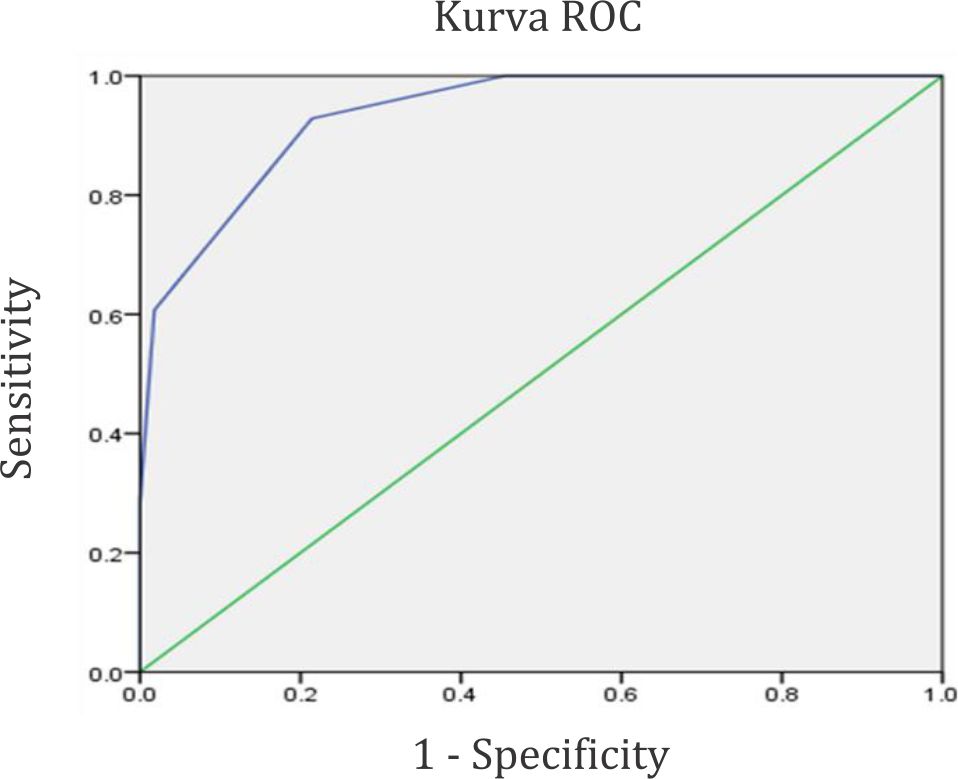
Figure 1. ROC curve for three warning signs for detecting severe dengue infection
DISCUSSION
Warning sign is an early indication for identifying the risk of SD, and starting early intravenous fluid replacement can lead to a better prognosis.10 Abdominal pain is the most frequent symptom of warning sign in dengue infection, and consistent with the present study which showed that 68 patients (59.5%) had complaints of abdominal pain. Vomiting was the most frequent clinical symptom. This is a popular symptom that can be easily recognized and monitored even by the patients. When the vomiting signs were compared between the groups with or without dengue and with or without warning signs (D/DWS) versus those with SD, the severe dengue group had a significantly higher prevalence of vomiting signs and also a higher median number of vomiting episodes.11 Vuong et al11 reported that persistent vomiting is as an early sign for the detection of SD infection. It showed that the frequency of vomiting signs was significantly higher among patients in the SD group (92%, 11/12) than among patients in the D/DWS group (49%, 33/67), and the median number of vomiting episodes per day was also significantly higher in the SD group (2.5, range: 2–3) than in the D/DWS group (0, range: 0–2). Furthermore, the study found that persistent vomiting was associated with the development of SD in 54% of the patients (OR 12.0), and the number of two or more vomiting episodes per day while predicting SD among the D/DWS group of patients showed good sensitivity (92%) and specificity (52%).11
Shock with or without respiratory distress has been reported to be the most frequent complication in patients with SD that was caused by a clinical fluid accumulation.9 In the present study, clinical fluid accumulation was found in 20 patients with NSD infection and 21 patients with SD infection. Similarly, Jayaratne et al5 reported that fluid accumulation was associated with SD (OR 2.94) and was found in 21 cases of NSD and 11 cases of SD infection.
Mucosal bleeding is a manifestation that is found in patients with mild to SD infection and potentially severe infection.12 Leo et al6 showed that mucosal bleeding was commonly found in patients with dengue infection (75.9% of cases), with a sensitivity of 98% for the detection of SD. Meanwhile, in the present study, although it found fewer cases of mucosal bleeding (42.14%, 59/140), there was still a significant association between mucosal bleeding and SD (OR 9.1). Therefore, these results indicated that the presence of mucosal bleeding is a sign for detecting SD infection, which is consistent with the 2009 WHO criteria.
In the present study, hepatomegaly was found to be associated with the incidence of SD infection. Nevertheless, after the logistic regression analysis, this association was diminished. However, Ledika et al9 reported that hepatomegaly was significantly associated with the incidence of SD (OR 21.72, 95% CI 7.73– 61.01). Hepatomegaly occurs in dengue infection due to the direct involvement of the dengue virus in the liver. Pothapregada et al13 also reported a significant association of hepatomegaly with SD infection (OR 4.3) and shock (81%). It showed that hepatomegaly is a risk factor for shock in children, as well as for SD virus infection.13
Rigau-Perez et al14 reported that there is a high incidence (17%) of impaired consciousness during dengue infection. Impaired consciousness is associated with high mortality and impaired organ disorders.15 This study showed that lethargy is a warning sign that primarily contributed to the incidence of SD (OR 43.1). Woon et al16 in Malaysia also reported that lethargy is a warning sign often occurring in children with SD (62.5%, p=0.014). This finding is in accordance to the fact that lethargy is a well-established warning sign that contributes to the risk of SD infection and dengue deaths, as reported in Singapore that shock was the commonest cause of death, followed by organ impairment (71.4% with acute renal impairment, 57.1% with impaired consciousness, and 53.6% with severe hepatitis).14
This study showed that increase in hematocrit concurrent with a rapid decrease in platelet count was not associated with SD infection. Similarly, Carrasco et al17 reported that increase in hematocrit concurrent with a rapid decrease in platelet count was not significantly associated with SD (2%, 2/96 cases, p=0.42). Concurrent increase in hematocrit and a rapid decrease in platelet count are significant in predicting severe hemorrhage and severe plasma leakage. Good predictors of DHF were not necessarily good predictors of SD infection. Carlos et al18 found that increase in hematocrit and low platelet count were significant in the DHF group (p<0.001), but these factors were not significant predictors of SD infection. Jayaratne et al5 reported that a platelet count of <20,000 was significantly associated (p=0.001) with SD infection (OR 1.632 to 455.2). The time the platelet counts dropped to <20,000 cells/mm3 that in those critical phase can be life threatening or even death. However, platelet counts alone did not appear to have a good discriminatory value in predicting the severity of dengue infection.
There were 28/114 (20%) cases of SD infection in this study. This was relatively similar to a previous study in Bandung (24.6%),9 but slightly higher than that reported in Surabaya (15.9%).10 The difference in the severity of dengue infection might be influenced by several factors, including host and viral factors. The interactions among viral, host, and epidemiological risk factors are the determinants of the occurrence of DHF epidemics. Viral factor implies strain virulence, serotype, while host factors include race, age, sex, nutritional status, secondary infection, and host response. Epidemiological risk factors include the number of susceptible individuals, high vector density, broad viral circulation, and hyperendemicity.19
In the present study, the logistic regression analysis showed that the presence of five warning signs was significantly associated with SD infection (p<0.05), including persistent vomiting, clinical fluid accumulation, mucosal bleeding, lethargy, and hepatomegaly. However, after the multivariate analysis, only persistent vomiting, clinical fluid accumulation, mucosal bleeding, and lethargy were significantly associated with SD infection. Andrade et al20 in Brazil reported that mucosal bleeding, persistent vomiting, and severe abdominal pain were associated with SD infection. Alexander et al21 reported that abdominal pain, mucosal bleeding, and decreased platelet count were significantly associated with SD infection.
The 2009 WHO dengue classification showed a sensitivity of 92.1% and a specificity of 78.5% to detect SD infection.8 This study showed that the cutoff point of the number of warning signs for detecting SD infection was three or more warning signs, with a sensitivity of 92.9% and a specificity of 78.6%. Win et al22 also reported that the presence of three or more warning signs is associated with SD infection. Similarly, Thein et al4 reported that the presence of three or four warning signs has a high specificity (95%–98%) in detecting SD infection. Jayaratne et al5 found that the presence of five or more warning signs was significantly associated with SD infection (OR 5.14), whereas the presence of two or less warning signs significantly reduced the risk of SD (OR 0.45). This difference is due to the category increase in the hematocrit concurrent with a rapid decrease in platelet count, wherein two categories were used in the study of Jayaratne et al.5
The limitation of this study is that secondary data collected from the medical records were used as a source of information, which are often incomplete and inaccurate. Several studies have reported different results because several factors affecting SD were not analyzed in this study, such as virulence, assessment of warning signs according to febrile duration at admission to hospital, and others. However, this study had a sufficient sample size for the distribution of patients with SD infection similar to some regions in Indonesia and can be a reference for further research.
This study developed an easily implementable predictive tool based on the presence of three or more warning signs. This tool can be used to identify SD infection at admission, thereby facilitating the initiation of early intervention and frequent monitoring, which could help in saving the patient’s life and reducing complications and the risk of death.
In conclusion, three or more early warning signs in patients with dengue can help in the identification of severe infection at admission with high sensitivity, which may help save patients’ life and avoid complications.
Conflicts of Interest
We declare that we have no conflict of interest.
Acknowledgment
The authors would like to thank the Director of H. Adam Malik General Hospital for permission to publish this paper. This Study is supported by Department of Pediatrics, Faculty of Medicine, Universitas Sumatera Utara.
REFERENCES
- Pongpan S, Wisitwong A, Tawichasri C, Patumanond J, Namwongprom S. Development of dengue infection severity score. ISRN Pediatr. 2013;2013:845876.
- Ministry of health republic Indonesia. Profile of disease control and environmental sanitation in 2011. Jakarta : Directorate general of disease control and environmental sanitation ministry of health republic Indonesia. 2012;135–8.
- Sumatera provincial health office. The Health profile of North Sumatera Province 2012. Medan: Sumatera provincial health office. 2012;38–9.
- Thein TL, Gan VC, Lye DC, Yung CF, Leo YS. Utilities and limitation of the world healt organization 2009 warning sign for adult dengue severity. PLOS Negl Trop Dis. 2013;7:e2023.
- Jayaratne SD, Atukorale V, Gomes L, Thashi C, Wijesinghe T, Fernando S, et al. Evaluation of the WHO revised criteria for classification of clinical disease severity in acute adult dengue infection. BMC Res Notes. 2012;5:645.
- Leo YS, Gan VC, Ng EL, Hao Y, Ng LC, Pok KY, et al. Utility of warning signs in guiding admission and predicting severe disease in adult dengue. BMC Infect Dis. 2013;13:498.
- Pozo-Aguilar JO, Monroy-Martinez V, Diaz D, Barrios- Palacios J, Ramos C, Ulloa-García A, et al. Evaluation of host and viral factor associated with severe dengue based on the 2009 WHO classification. Parasites Vectors. 2014;7:590.
- Narvaez F, Gutierrez G, Perez MA, Elizondo D, Nuriez A, Balmaseda A, et al. Evaluation of the traditional and revised WHO classifications of dengue disease severity. PLoS Negl Trop Dis. 2011;5(11):e1397.
- Ledika MA, Setiabudi D, Dhamayanti M. Association between clinical profiles and severe dengue infection in children in developing country. American Journal of Epidemiology and Infectious Disease. 2015;3(3):45–9.
- Basuki PS, Budiyanto, Puspitasari D, Husada D, Darmowandowo W, Ismoedijanto, et al. Application of revised dengue clasification criteria as a severity marker of dengue viral infection in Indonesia. Southeast Asian J Trop Med Public Health. 2010;41(5):1088–94.
- Vuong NL, Manh DH, Mai NT, Phuc LH, Luong VT, Quan VD, et al. Criteria of persistent vomitting in the WHO 2009 warning sign for dengue case classification. Trop Med Health. 2016;44:14.
- Lee IK, Liu JW, Chen YH, Chen YC, Tsai CY, Huang SY, et al. Development of a simple clinical risk score for early prediction of severe dengue in adult patients. PLoS One. 2016;11(5):e0154772.
- Pothapregada S, Kamalakannan B, Thulasingham M. Risk factors for shock in children with dengue fever. Indian J Crit Care Med. 2015;19(11):661–4.
- Rigau-Pérez JG, Laufer MK. Dengue-related deaths in Puerto Rico, 1992-1996: diagnosis and clinical alarm signals. Clin Infect Dis. 2006;42(9):1241–6.
- Leo YS, Thein TL, Fisher DA, Low JG, Oh HM, Narayanan RL, et al. Confirmed adult dengue deaths in singapore: 5 years multi center retrospective study. BMC Infect Dis. 2011;11:123.
- Woon YL, Hor CP, Hussin N, Zakaria A, Goh PP, Cheah WK. A two year review on epidemiology and clinical characteristic of dengue deaths in Malaysia, 2013-2014. PLoS Negl Trop Dis. 2016;10(5):e0004575.
- Carrasco LR, Leo YS, Cook AR, Lee VJ, Thein TL, Go CJ, et al. Predictive tools for severe dengue conforming to world health organization 2009 criteria. Plos Negl Trop Dis. 2014;8(7):e2972.
- Carlos CC, Oishi K, Cinco MT, Mapua CA, Inoue S, Cruz DJ, et al. Comparison of clinical features and hematologic abnormalities between dengue fever and dengue hemorrhagic fever among children in the Philippines. Am J Trop Med Hyg. 2005;73(2):435–40.
- Hadinegoro SR. The revised WHO dengue case classification: does the system need to be modified? Paediatr Int Child Health. 2012;32(1):33–8.
- de Andrade SM, Herkert CM, de Cunha RV, Rodrigues MD, da Silva BA. A new approach to reducing mortality from dengue. Open Journal of Clinical Diagnostics. 2014;4:12–6.
- Alexander N, Balmaseda A, Coelho IC, Dimaano E, Hien TT, Hung NT, et al. Multicentre prospective study on dengue classification in four South-east Asian and three Latin American countries. Trop Med Int Health. 2011; 16(8):936–48.
- Win MM, Phumratanaprapin W, Phonrat B, Dhitavat J, Sutherat M, Luvira V, et al. Warning signs to predict severe dengue in adult patients at hospital for tropical diseases Thailand. In: Faculty of Tropical Medicine Mahidol University, Editors. Tropical disease post 2015: New threats or towards sustainable success. Bangkok: Faculty of Tropical Medicine Mahidol University, 2015.p.81.
Copyright @ 2018 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id