
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Brief Communication
The knowledge retention after continuing health education among midwives in Indonesia
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v27i2.2413 Med J Indones. 2018;27:128–33
Received: November 14, 2017
Accepted: Macrh 19, 2018
Author affiliation:
1 Department of Nutrition, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo General Hospital, Jakarta, Indonesia
2 Faculty of Psychology, Universitas Indonesia, Depok, Indonesia
3 Nestle Nutrition Institute – PT Nestle Indonesia, Indonesia
Corresponding author:
Saptawati Bardosono
E-mail: tati.bardo@yahoo.com
Background
Amongst the Health Care Professionals, midwife has a strategic role in taking care of both mother and child in contributing to their survival, health, and wellbeing. The retaining midwife’s knowledge and quality of care through training on specific skills is strongly needed. This study aimed to evaluate the knowledge retention among midwives after the provision of digestive health, nutrition, and parenting education sessions at immediate and three months after the education.
Methods
A serial pre-post intervention experimental study was conducted from January to July 2016 to evaluate the knowledge before (pre-test), immediate after (post-test), and three months after the provision of three sessions of digestion health, nutrition, and parenting (character building) topics by the experts which covered from several areas in Indonesia. The improvement of the sufficient knowledge proportion time by time was analyzed by using McNemar test.
Results
The low immediate response rate (77.2%) and very low response after the 3-month follow-up (26.4%) were revealed during the study. At baseline, less than 50% of the subjects had sufficient knowledge on digestive health, nutrition, and parenting. At immediate after and after three months, there were significant improvements in the proportion of sufficient knowledge in nutrition and parenting topics. However, there was a declining of sufficient knowledge at after 3 months group compared to immediate group.
Conclusion
The knowledge retention from the continuing health education among widwives in Indonesia decreased after 3 months.
Keywords
digestive health, knowledge, midwives, nutrition, parenting
Amongst the Health Care Professionals, midwife has a strategic role in taking care of both mother and child in contributing to their survival, health, and wellbeing.1 Therefore, improving midwife’s knowledge and quality of care through training on specific skills is strongly needed. The training program should be designed to evaluate and demonstrate changes in midwife’s knowledge, and hopefully also improving their skills that could be evaluated at immediately after the training, and its retention above baseline overtime.2
In-service training or so-called continuing health education will improve the quality of midwife by rendering more knowledge and competence.3 Besides emphasizing antenatal care and birth preparedness practices through training, issues to optimal child growth and development in relation to healthy digestion, nutrition, and parenting are also substantial for midwife to manage child nutrition related conditions.4,5 Furthermore child nutritional status is not merely affected by food intake. It also needs healthy digestion to be able to absorb all nutrients from the food consumed. Moreover, to complete the child growth and development, good parenting skill is needed to support building child character.6
Until now, there is no study to evaluate the knowledge retention among midwives in Indonesia. This study aimed to evaluate the knowledge retention among midwives after the provision of digestive health, nutrition, and parenting education sessions at immediate and three months after the education.
METHODS
Study design
A serial pre-post intervention experimental design was conducted to evaluate knowledge of midwives before, immediate after the continuing health education, and at three months later. A serial measure on knowledge were done each of the time, i.e. before, immediate after, and three months after the education sessions.
Place and time
Data collection was covering several big cities in Indonesia, i.e. Medan, Tangerang, Bandung, Yogyakarta, and Balikpapan, from January to July 2016. These were done after receiving the Ethical Approval from the Ethical Committee of Faculty of Medicine Universitas Indonesia, No. 276/UN2.F1/ETIK/2016.
Population and subjects
All midwives who participated the continuing health education from January to May 2016 were recruited after signing the informed consent for their participation willingness. There was in average about 400 midwives following the education program in each city. By using 95% confidence interval and 90% of power to detect 10% of score improvement and assumed standard deviation of 50%, a minimal sample size of 263 midwives was needed.
Data collection
Characteristics of the subjects, age, education, employment status, years having midwifery practice, and ownership of maternity clinic were gathered through self-administered questionnaire. Knowledge on digestive health, nutrition, and parenting in character building were collected also by using self-administered questionnaire before, immediate after, and three months after the education sessions, in which the right or wrong answer was scored as five or zero, respectively. The questionnaires to evaluate the knowledge were constructed as a formative research questionnaire by each of the resource person who was professional in the topic and responsible as the lecturer to deliver the topic. It was consisted of six questions used to evaluate digestive health knowledge, 11 questions for nutrition topic, and 11 questions for parenting topic. Sufficient knowledge was determined if the subjects could reach 80% of the total score.
Data was managed by using a statistical program for social sciences (SPSS) version 20, and presented descriptively. Statistical analysis was performed by using McNemar test to evaluate the improvement of sufficient knowledge proportion between baseline, immediate after, and three months after the intervention. The p-value of less than 0.05 was used to interpret statistical significance of the test.
RESULTS
During the screening period, the study recruited 1,783 subjects from five study areas (Figure 1). However, during the immediate after of the training, there was a subject reduction number in which only 1,376 (77.2%) of the subjects took the post-test. Three months after the education program, we mailed the questionnaire to all subjects, but only 471 subjects (26.4%) responded.
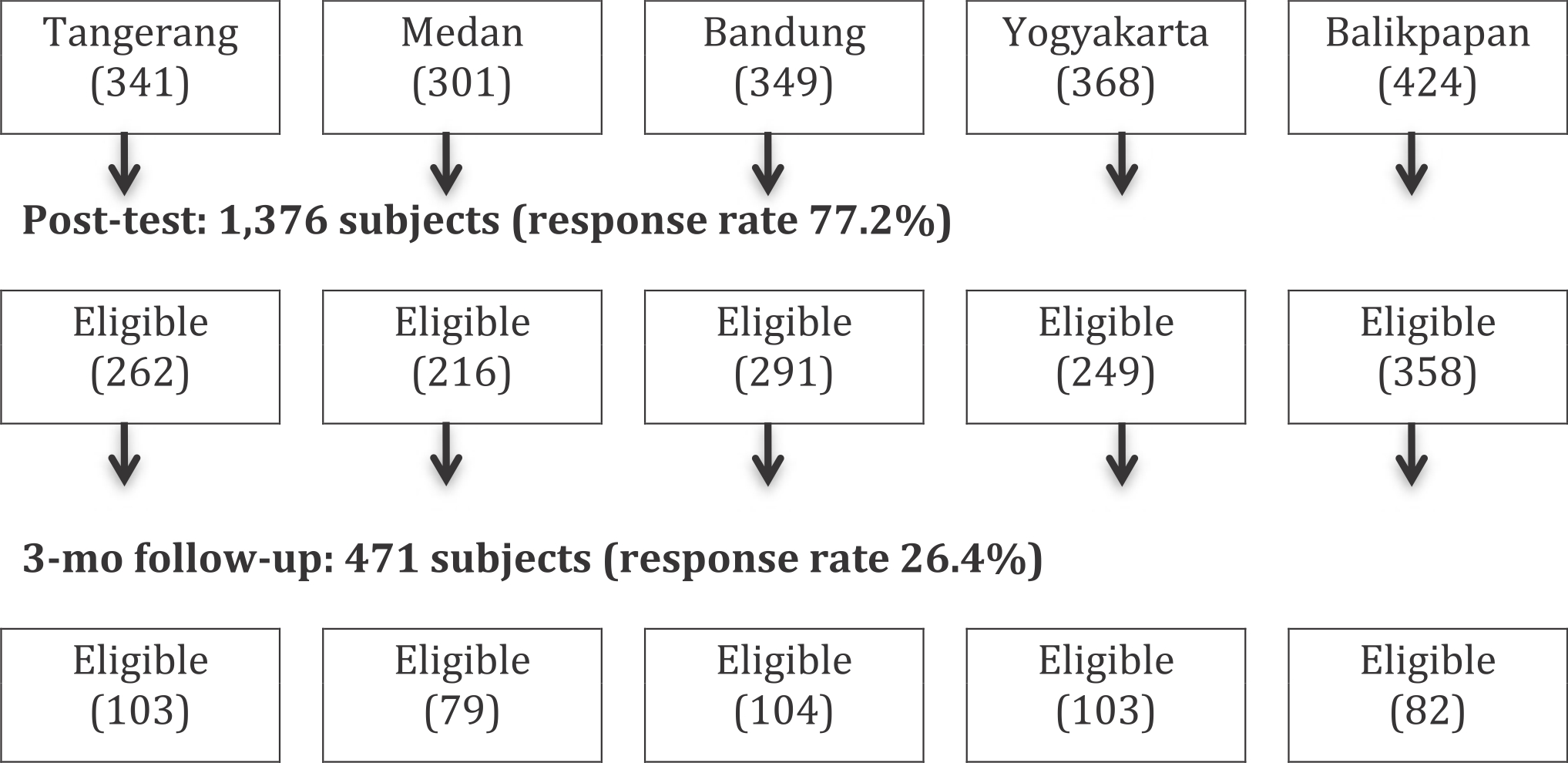
Figure 1. Figure 1.
Basic characteristic of the subjects are described in Table 1. The age was widely varied and mostly the subjects had middle-low level of midwifery training (69.9%). Less than 50% had their private and/or self-managed practice twice a week and/or every day, and mostly (58.2%) had their own maternity clinic.
Table 1. Characteristics of the subjects (n=471)
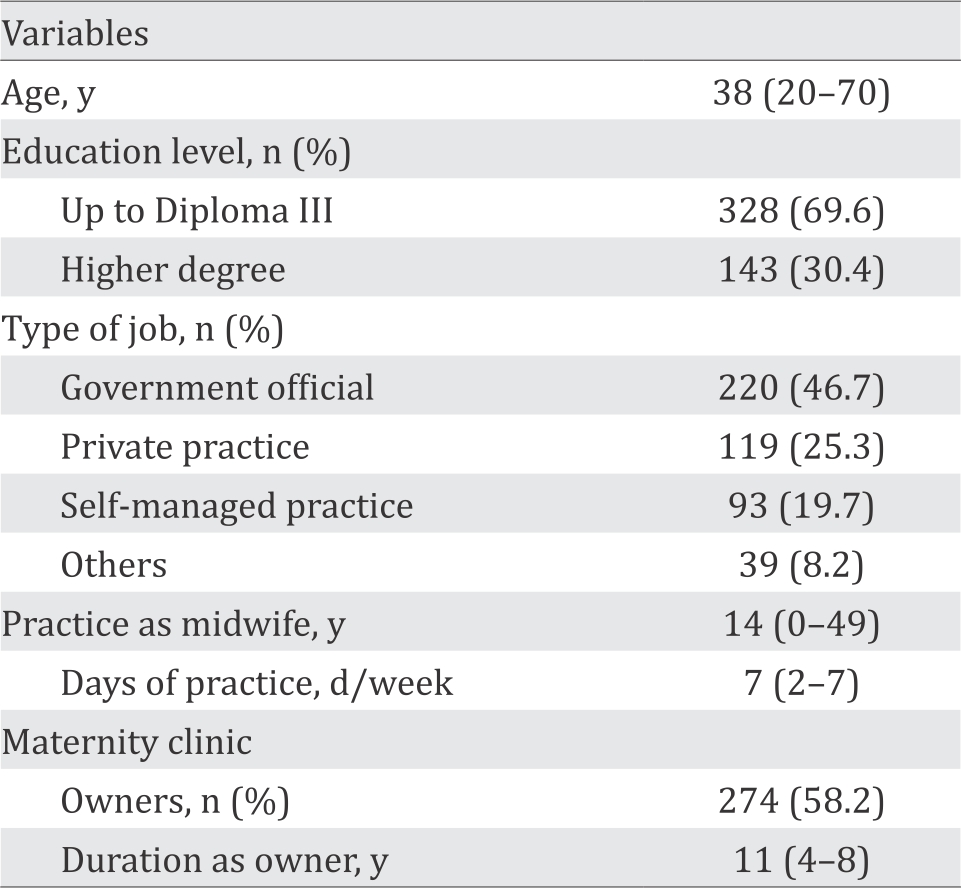
Table 2 shows that less than 50% of the subjects had sufficient knowledge in digestive health (38.6%), nutrition (42%), and parenting for character building (44.8%). At the immediate after or post-test results, there was slightly reduction of sufficient knowledge proportion in digestive health. There were significant improvements in the proportion of sufficient knowledge of more than 20% in nutrition and parenting for character building.
Table 2. Improvements in the proportion of sufficient knowledge (n=471)
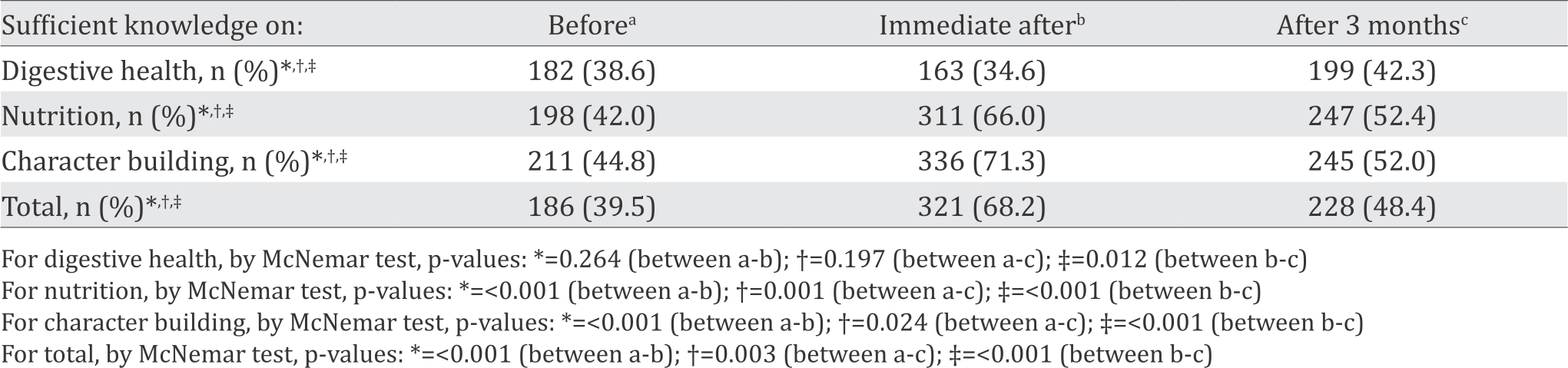
After three months, again there was no significant improvement in the proportion of sufficient knowledge in digestion health (p=0.197) as compared to the baseline, but there was a significant improvement as compared to the immediate after (p=0.012). For sufficient nutrition knowledge, there was a significant reduction as compared to the immediate after (p<0.001). Similarly, there was a significant reduction as compared to immediate after (p<0.001). Thus, in total, there was a significant reduction in the proportion of knowledge at three months after the education as compared to the immediate after (p<0.001), as shown in Table 2.
DISCUSSION
This study was considered as the first study that presented the evaluation of knowledge of midwives on digestive health, nutrition, and parenting among midwives in Indonesia within the continuing health education format in 3 months. During a followup study, it is challenged to maintaining the subjects’ compliance after three months which the response rate was 26.4% (Figure 1). This finding was still in range of the systematic review by Sykes et al7 on response rate of health surveys from articles published from January 1990 to June 2009, which found the response rates between 22.0–68.8%. However, our result was lower than another systematic review of response rates between 1996 and 2005 by Cook et al8 which found an average response rate in doctors was 57.5% (95% CI: 55.2% to 59.8%). It was higher than response rate of midwives for an e-learning program (15%).9 However, although the response rate was low in this study, we still could reach the calculated minimal sample size of 263 subjects until the end of the study.
Several factors affected response rate, including survey mode, length of questionnaire, survey language, and cultural sensitivity to content.7 Cook et al8 found that response rates were higher when reminders were sent (adjusted OR 1.3; 95%CI 1.1-1.6), and in studies with less than 1,000 participants. Edwards et al10 in a systematic review found some strategies were efficient to improve the response rate of a study, such as by providing monetary incentive (and almost doubled when incentives were not conditional on response), using short and personalized questionnaires and letters, using colored ink, and designing interesting questionnaires, sending the questionnaire by recorded delivery, by first class post, as well as by adding stamped return envelopes. Contacting participants before sending questionnaires and following up contacts also increased response.
Cunningham et al11 that specifically purposed to explore response rates among physician (904) also found similar result of a very low response rate (35.0%) of physician toward the survey. This study used an internet-based questionnaire. However, multiple methods were also used to encourage survey response such as individual personalized email invitation, multiple reminder, and a draw for three gift certificate prizes were used to increase response rate. Nonrespondents listed lack of time/survey burden as the main reason for not responding. In this study, the questionnaires were sent by postal method. A personalized letter, stamped return envelope, and souvenir were attached in the envelopes. We also contacted the participants by phone before sending the questionnaire and made followup calls. The wide variation of the subject’s characteristics may affect the response rate.
Although the response rate is low after 3 months, however, the number of sample more than 400 can be a representative for this kind of study. Further study should consider multiple methods or sending follow up reminders using an electronic survey or internet-based survey is needed. Important attention needs to be given to improve midwife capacity to support the health and nutrition of children.
In terms of knowledge enhancement as the effect of the training, at baseline it was found less than 50% of the subjects had sufficient knowledge in digestive health, nutrition, and parenting for character building (Table 2). This shows how those three topics were important to be delivered to the midwives at any opportunity as their on-going continuing education. It is understood that gut health is an important issue in which there is a role of nutrition to gut health and brain axis.6 While for parenting knowledge, there is also a need for midwives to support the promotion of parenting self-efficacy for the new mothers.12 While for nutrition, a literature review in from Arrish13 that included eight studies in the final review reported that midwives lacked a basic knowledge of nutrition requirement during pregnancy. This might be attributed to inadequate nutrition education provided in both undergraduate and postgraduate midwifery programs. Nevertheless, nutrition education components of midwifery courses were not identified within the study reviewed.
In this study, knowledge increased was found at the immediate after the training (i.e. 39.5% at baseline and 68.2% at immediate after), but it was not retained after three months evaluation (48.4%). Thus, the knowledge retention was not maintained. Naeem et al14 suggested that although short training led to increase knowledge, however, to be able to retain the knowledge, there was a need to do regular and periodic refreshers, especially to topics that are not applied regularly. A cohort study done in Mozambique15 showed that in the range of six moths after the assimilation of knowledge, there was a deficit in knowledge retention and resulting in loss of information in all the topics provided during the courses. There are several reasons, i.e. decreased in the performance interfering in perceptual mechanisms and levels of attention, the willingness of the subjects to learn, the logic and meaningful of the presented content, and the role of the resource persons to make the content interesting to learn in having new ideas with transformation and refinement of what was already known. Especially for midwives, knowledge and understanding of child health related sciences are essential to their daily practice, particularly when faced with the continual advancement of promotion and prevention modalities. Another suggestion to assist in its retention is by perceived relevance demonstrated through applicability to practical situations.16
In conclusion, the knowledge retention from the continuing health education among midwives in Indonesia decreased after 3 months. Thus there is a need to do regular and periodic refreshers, especially to topics that are not applied regularly, to retain the knowledge.
Conflicts of Interest
Ray Wagiu Basrowi and Yulianti Wibowo as employees of Nestle Nutrition Institute are supporting this study in the scientific site.
Acknowledgment
This study was done during the scientific meeting “Kartini Update” conducted by PT. Nestle Indonesia. We would like to thank all the midwives participating in the study since the beginning until the end. High appreciation is given to the Indonesian Midwives Association in facilitating and supporting the study.
REFERENCES
- Biro MA. What has public health got to do with midwifery? Midwives’ role in securing better health outcomes for mothers and babies. Women Birth. 2011;24(1):17–23.
- Hennessy D, Hicks C, and Koesno H. The training and development needs of midwives in Indonesia: paper 2 of 3. Hum Resour Health. 2006;4:9.
- Agrawal N, Kumar S, Balasubramaniam SM, Bhargava S, Sinha P, Bakshi B, et al. Effectiveness of virtual classroom training in improving the knowledge and key maternal neonatal health skills of general nurse midwifery students in Bihar, India: a pre- and post-intervention study. Nurse Educ Today. 2016;36:293–7.
- Mueler NT, Bakacs E, Combellick J, Grigoryan Z, Dominguez-Bello MG. The infant microbiome development: mom matters. Trends Mol Med. 2015;21(2):109–17.
- Sodjinou R, Bosu WK, Fanou N, Déart L, Kupka R, Tchibindat F, et al. Nutrition training in medical and other health professional schools in West Africa: the need to improve current approaches and enhance training effectiveness. Glob Health Action. 2014;7:24827.
- Oriach CS, Robertson RC, Stanton C, Cryan JF, Dinan TG. Food for thought: the role of nutrition in the microbiotagut– brain axis. Clin Nutr Exp. 2016;6:25–38.
- Sykes LL, Walker RL, Ngwakongnwi E, Quan H. A systematic literature review on response rates across racial and ethnic populations. Can J Public Health. 2010;101(3):213–9.
- Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: an observational study. BMC Health Serv Res. 2009;9:160.
- Hunter AT. Perceived effectiveness of clinical e-learning for Georgia midwives. Dissertation. University of South Carolina; 2014.
- Edwards PJ, Roberts I, Clarke MJ, DiGuiseppi C, Wents R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009;8(3):MR000008.
- Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol. 2015;15:32.
- Gao LL, Sun K, Chan SW. Social support and parenting self-efficacy among Chinese women in the perinatal period. Midwifery. 2014;30(5)532–8.
- Arrish J, Yeatman H, Williamson M. Midwives and nutrition education during pregnancy: a literature review. Women Birth. 2014;27(1):2–8.
- Naeem N. Which knowledge and skills do participants retain after attending medical education training workshops? Creat Educ. 2016;7:870–7.
- Ferreira JJ, Maguta L, Chissaca AB, Jussa IF, Abudo SS. Cohort study to evaluate the assimilation and retention of knowledge after theoretical test in undergraduate health science. Porto Biomed J. 2016;1(5):181–5.
- Malau-Aduli BS, Lee AY, Cooling N, Catchpole M, Jose M, Turner R. Retention of knowledge and perceived relevance of basic sciences in an integrated casebased learning (CBL) curriculum. BMC Med Educ. 2013;13:139.
Copyright @ 2018 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id