
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Community Research
Perception of the Zika virus infection and its influence on Zika prevention practices by pregnant women at the Region 5 Health Promotion Center in Thailand
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v27i3.2424 Med J Indones. 2018;27:201–8
Received: November 22, 2017
Accepted: August 23, 2018
Author affiliation:
Department of Social Science, Faculty of Liberal Arts, Rajamangala University of Technology Thanyaburi, Thailand
Corresponding author:
Issara Siramaneerat
E-mail: issara_s@rmutt.ac.th
Background
The Zika virus (ZIKA) infection in pregnant women causes microcephaly, a brain disorder resulting in severe birth defects. The objective of this study was to identify the factors that influence Zika prevention practices by pregnant women at the Region 5 Health Promotion Center in Thailand.
Methods
A cross-sectional study applied a survey method to collect data from pregnant women between 18 and 45 years of age. The sampling method used multistage random sampling. The data were analyzed using descriptive statistics and multiple linear regression analysis.
Results
The findings indicated that 5 of 12 factors could significantly predict Zika prevention practices of pregnant women at the Health Promotion Center Region 5 in Thailand: education, smoking behavior, check-up status during pregnancy, perception of susceptibility, and perception of benefit.
Conclusion
The results show a direct correlation between the perception of susceptibility and benefit and Zika prevention practices. Policies for promoting Zika knowledge and preventive behavior by providing information about Zika should focus on changing the thoughts, attitudes, and beliefs of pregnant women and their families.
Keywords
perception, pregnant, Thailand, Zika
World Health Organization (WHO) has proclaimed a Zika infection as public health emergency, with many countries affected.1 The Zika virus infection was first reported in humans in Nigeria in 19541 , and there have been many outbreaks of the disease in Oceania countries between 2007 and 2017.2,3 The transmission route of Zika in humans is through a mosquito bite. Acute infections from ZIKA are usually mild. Common symptoms include rash, arthralgia, muscle pain, headache, conjunctivitis, fever, rash, and joint pain.4 Most people do not need to worry about the Zika virus because it is not fatal and the symptoms are usually mild, with a duration of about one week.4 However, the Zika virus is extremely dangerous to pregnant women.1–3 Normally, the risk of infection in pregnant women increases 18-fold during pregnancy due to reduced immunity in the cells.5 Although Zika’s symptoms are mild and can disappear within one week for a mother, 6 the effect on a child in utero is completely different and much more dangerous. Therefore, Centers for Disease Control and Prevention (CDC) recommend that pregnant women and those attempting to become pregnant take special precautions to prevent Zika.6 Zika infection in pregnant women has been proven to cause microcephaly, a brain disorder resulting in severe birth defects.6,7 Children with microcephaly are at a high risk of delays in cognitive development, hearing and visual impairment, and other abnormalities.6,7 According to a study in Brazil, incidences of microcephaly increased during an outbreak of Zika, with over 3,800 cases or 20 cases per 10,000 live births.8 Because of this threat, countries around the world need to be cautious about the Zika virus spreading to other areas, including Southeast Asia,6 where Aedes albopictus and Aedes aegypti mosquitoes are present.7
In Thailand, an organized observation and a collection of information about patients infected with the Zika virus began in May 2012 and was systematically expanded in 2017.6 There were 392 Zika cases reported in Thailand in 2017; this number includes 86 pregnant women and two cases of babies being born with abnormal head circumferences.9 Until now there is no vaccine or treatment against Zika. Nearly 80% of people infected by this virus show almost no specific symptoms, making it difficult to diagnose, especially in pregnant women.6,7
Located in the center of Southeast Asian countries, the Kingdom of Thailand spans 514 kilometers and is divided into four areas: Central (including Bangkok), North, Northeast, and South. These four regions are divided into 76 provinces.10 This entire area is covered by 12 Health Promotion Center Regions.9 The Region 5 Health Promotion Center (HPCR5) includes eight provinces: Ratchaburi, Nakhon Pathom, Suphanburi, Karnchanaburi, Samut Sakhon, Samut Prakarn, Phetchaburi, and Prachuap Khiri Khan.9 HPCR5 has large and medium-sized industrial areas, including the fishing industry, many factories, and many unregistered migrant workers, all of which are factors that increase the risk of spreading the disease.8 More importantly, the Ministry of Public Health of Thailand has confirmed Zika virus infections in HPCR5 since 2012.11 In the period from January 2016 to June 2017, HPCR5 reported that the morbidity per population of 100,000 was 0.31. Cumulatively, this morbidity was found in 99 cases in the age group above 15 years; seven of these were infected pregnant women. Fortunately, no newborn babies from these cases are suffering from microcephaly or Guillain-Barré syndrome (GBS).11
Accurate knowledge and increased awareness of the disease are critical to the effective prevention and treatment of ZIKA. An increased role of knowledge has been widely proposed in the areas of health behavior and health behavior change, including in the health belief model (HBM).12–14 The HBM model states that one’s practice of health beliefs is influenced by one’s perception of a disease; increased perception and therefore knowledge about the disease will later improve the patient’s compliance during treatment. In turn, this condition affects the decrease in prevalence as well as the occurrence of further complications.12 Moreover, the degree of perception about the seriousness of a disease directly impacts how a person behaves with regard to get help for health issues, such as the recommended use of health care and medication adherence.12 A nationwide study has proven that an increased perception about the severity of dengue fever has been a major factor in the increase of better prevention practices.15 Likewise, it is hypothesized that the perceived severity of Zika is associated with enhanced mosquito control practices. Little is known about what effect the perception of Zika prevention and control practices has on pregnant women in Thailand.
Thus, this paper aims to identify the factors that influence Zika prevention practices by pregnant women in the Region 5 Health Promotion Center of Thailand. The Ministry of Public Health could take advantage of the resulting database in order to influence how people involved in all sectors make decisions about Zika prevention practices. Both operational and management levels could develop an effective plan to prevent and control the spread of Zika virus infections in accordance with the conditions mentioned in this study.
METHODS
This was a cross-sectional study that used the survey method. The researchers conducted surveys in the eight provinces of the Region 5 Health Promotion Center: Ratchaburi, Nakhon Pathom, Suphanburi, Karnchanaburi, Samut Sakhon, Samut Prakarn, Phetchaburi, and Prachuap Khiri Khan.9 The Ministry of Public Health reformed its management system in 2014, with the management structure formatted across 12 health zones.9 The main purpose was to adjust the operational roles and mechanisms to provide people with quality health care services regardless of where they live. The reason for selecting the Region 5 Health Promotion Center for this research was because this region has both large and mediumsized industrial areas that increase the risk of spreading the disease.9 Most importantly, the Region 5 Health Promotion Center reported the largest number of pregnant women registered.16 This study was officially approved by the Institutional Review Board (IRB) in the Kanchanabhishek Institute of Medical and Public Health Technology, Ministry of Public Health, as KMPHT No. 2016/60020061.
There were approximately 47,889 pregnant women registered.16 According to population study norms, approximately 380 samples are necessary to make accurate projections for a given population over 40,000.17 In order to make allowances for incomplete data or invalid surveys, 395 samples were assigned in this research. The sample size was calculated by using an error margin of 5% and confidence interval levels of 95% to appropriately represent the pregnant women in the Region 5 Health Promotion Center. Inclusion criteria were as follows: (1) pregnant women aged ≥18 years old; (2) able to speak Thai; and (3) willing to participate in this study. Respondents who fulfilled these criteria were then given information about the purpose, benefit, and procedure of this research. Respondents were interviewed after agreeing using verbal consent. The interview was done by a trained enumerator in order to ensure the quality of the data collection. The next step was to complete an interview with each respondent as guided by a questionnaire. An interview was considered complete when a respondent had either answered all the questions or withdrew his/her participation from the study. Incomplete questionnaires were excluded from the study. Data was collected from May–June 2017 and entered into a database.
This study employed multistage random sampling, which is a sample selection technique done in stages, and is usually based on the division of administrative territories. In stage one, we selected four provinces randomly out of the eight provinces: Ratchaburi, Nakhon Pathom, Suphanburi, and Karnchanaburi. In the second stage, we randomly selected pregnant women from the list provided by the District Health Promotion Center, which also provided addresses and contact information. The interviews took place in the respondents’ homes, except in cases where the respondent was not home, in which case the interview was conducted at a later time by phone.
The data was collected using structured questionnaires divided into seven sections as follows: (1) five questions about respondent demographics (age, marital status, education, occupation, and household monthly income); (2) four questions about respondent healthrelated behavior (pregnancy check-up status, smoking, drinking, and drug use); (3) 10 questions about the respondent’s knowledge of the causes, symptoms, and effects of Zika; (5) nine questions about the individual’s exposure to media as related to Zika information within the past six months; (6) 20 questions about the individual’s perception of Zika, including perception of susceptibility, vulnerability, benefits, and barriers; and (7) 18 questions about Zika prevention practices used within the past six months.
The respondents were classified into six age categories: 18–20 years, 21–25 years, 26–30 years, 31–35 years, 36–40 years, and >40 years old. The education levels were categorized as Primary, Junior High, High School/Vocational, Diploma, Bachelor, and Post-Graduate. The occupation categories included farmers, civil servants, contractors, employees, students, business operators, and other. The pregnancy check-up status was divided according to “never been checked” (coded as 1), “incomplete pregnancy check-up” (coded as 2), and “complete pregnancy check-up” (coded as 3).
Respondents’ knowledge about Zika was assessed based on 10 questions in the third section of the questionnaire, all of which had to be answered as “yes,” “no,” or “do not know.” Each correct answer was assigned 1 point, while each wrong or “do not know” answer was assigned zero points. The questions asked to assess individuals’ ZIKA-related knowledge included the method of Zika virus transmission, the most important precaution to take against Zika, Zika’s symptoms, and high risk people. Hence, the maximum possible score was 10. Respondents’ levels of knowledge were classified into three categories: low (score 0–3), moderate (score 4–6), and high (score 7–10).
The questions about the perception of Zika asked about the perception of susceptibility, vulnerability, benefits, and barriers in the six sections of the questionnaire.18 The perceived susceptibility question asked about Zika’s risk factors and transmission; the perceived severity question asked about the severity of Zika’s medication and ZIKA’s risk; the perception of benefit questions asked about Zika-benefit prevention; and the perception of barriers questions asked about the time spent in visiting medical doctors and creating barriers through prevention behavior. Each of the perceptions was measured using five questions. General perceptions about Zika were elicited by asking respondents to rank their agreement with five statements using a Likert scale numbered from 1 (strongly disagree) to 5 (strongly agree). Next, the answers were added together for a total final score. The final score number was then categorized as very low (1–5), low (6–10), moderate (11–15), and high (16–20).
The dependent variable was the preventive practice against Zika, which refers to mosquito bite prevention. The dependent variable was derived from 20 questions. These 20 questions represented mosquito bite prevention practices, including eliminating mosquito breeding places, practicing good nutrition and personal hygiene, using a facemask during influenza outbreaks, and accessing health resources when sick. Each item was scored as 3 (regular), 2 (often), 1 (once in a while), and 0 (never). In total, the score would fall between 0 and 60. The total score was categorized as low (0-19), moderate (20–39), and high (more then 40).
Before being used for the survey, the questionnaire was pretested with 30 individuals whose characteristics were similar to the study population in order to verify the clarity of the language used and the questionnaire’s structure.19 Wording revision then took place accordingly. A Cronbach’s alpha of 0.766 meant that the reliability of the questionnaire was acceptable.19 The content validity of the questionnaire was also validated by five experts, including nurses, public health practitioners, and social workers who work with pregnant women. The test contained 71 items and had an acceptable measure of content validity; the index of conjugate (IOC) was 0.95.
Descriptive statistics were used to describe the variables by presenting the mean and standard deviations for age, education, occupation, pregnancy check-up status, knowledge about Zika, perception of Zika, and preventive practices against Zika. This paper investigates the effect of socioeconomic factors, and knowledge and perception of Zika toward the preventive practice against Zika infection. The HBM model is used to describe the health behavior background that is based on the attitudes and beliefs described about a particular disease/ event. The HBM model illustrated that knowledge and perception of a disease affects a person’s behavior in the treatment and other behaviors associated with the disease experience.12,13 For the dependent variable measurement as an interval scale, the multiple linear regression was applied accordingly. Moreover, this method is suitable for predicting independent variable effects on interval scale dependent variables. The classical multiple linear regressions, such as normal distribution, multicollinearity, heteroscedasticity, autocorrelation, were satisfied at the minimum point.19 Multiple linear regression was performed using a statistical program application. Furthermore, the result is considered statistically significant if the p-value <0.05.
RESULTS
Table 1 presents the demographic characteristics of the 395 participants. Most respondents (37.22%) were 31–35 years old, and 36.2% of them had completed a Bachelor’s degree. The majority of the occupation statuses (28.35%) were businesswomen. Regarding household economic status, the median household monthly income of the participants was 35,837.97 baht, which fell within a large range, from 4,000 to 500,000 baht. The majority (76.96%) had completed a pregnancy check-up. The average of knowledge about Zika was 2.85 out of 10. Regarding perception, the perceived benefit was the highest average (x̅ =19.61) while the perceived barrier was the lowest average (x̅ =12.56). In addition, the preventive practice of Zika was revealed as moderate practice (x̅ =34.08).
Table 1. Social determinant, perception, knowledge and preventive practice of Zika
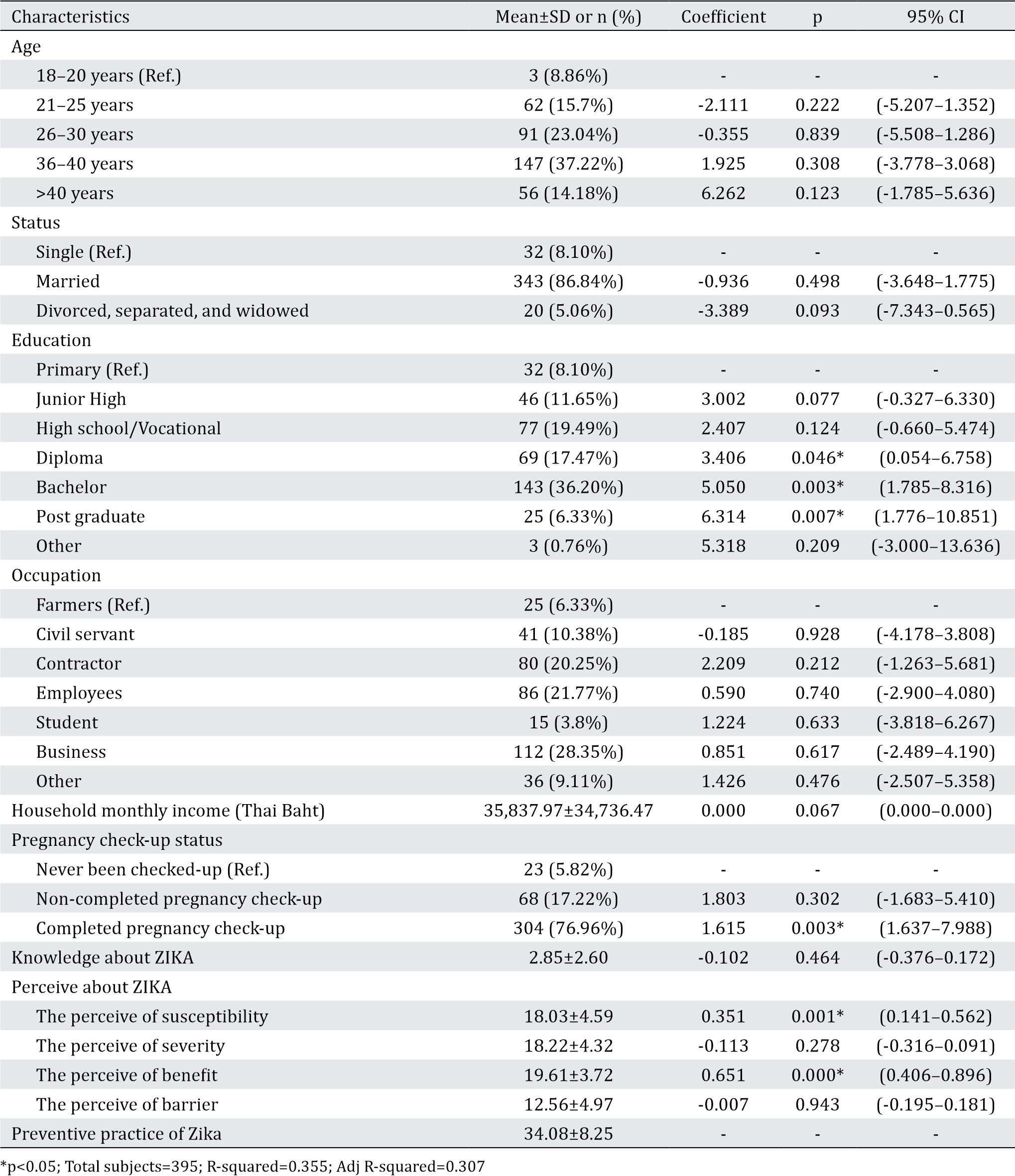
For multiple linear regression analyses, all variables, such as age, education, occupation, household monthly income, pregnancy checkup status, and knowledge and perception of Zika were included in the model. The results revealed that education significantly influenced Zika prevention practices during pregnancy. This is true particularly for those who graduated with a diploma or degree (Coefficient=3.406, 95% CI: 0.054–6.758), bachelor’s degree (Coefficient=5.050, 95% CI: 1.785–8.316), and post graduate degrees (Coefficient=6.314, 95% CI: 1.776–10.851).
In addition, women who completed a pregnancy check-up used more Zika prevention practices than others did (Coefficient=1.615, 95% CI: 1.637–7.988). Moreover, the perception of susceptibility and benefit positively influenced Zika prevention practices. The coefficients were 0.351 and 0.651, respectively. The regression model could explain the 35.50% variance of Zika prevention practices by pregnant women (R2=0.355).
DISCUSSION
This study found that the level of perception of Zika among pregnant women is low. This implies that the overall perception of Zika is not high among the study population. The target of promotion and prevention strategy in combating the Zika virus includes women who are planning to have a baby and their partners. The HBM was developed by several scholars according to the role of perception in changing health behaviors and sustained behavioral changes.12,13
Moreover, this study revealed that most of participants (pregnant women) in the survey had low levels of knowledge about Zika. This fact emphasizes the need for a government to promote informational campaigns directed at the target population. Correct knowledge about Zika is an important issue in preventing the transmission of the disease in pregnant women. In addition, husbands of pregnant women who often travel abroad need to be educated on all aspects of the Zika virus. Transferring knowledge using mass media would help reach a broader audience, but the media must distribute accurate information. More importantly, neonatal care providers such as nurses, health staff, and medical personnel play an important role in disseminating information.20,21
This research found that the perception of susceptibility and benefit are directly correlated with Zika prevention practices, which is consistent with the results of several other studies.20,21 Similar to a study in Malaysia, which found community involvement in combating Zika to be the main focus in Malaysia. Its main goal is to increase public perception of the severity of Zika.22
A person will take action or behave to prevent or control illnesses only when he or she believes it will decrease their susceptibility to the illness or that he or she will benefit from the recommended action.23 Therefore, the government should provide information on the health risks of Zika infection and the benefits of avoiding the virus through community education and media campaigns.23,24 Policies for promoting knowledge about Zika and associated preventive behavior should focus on changing the thoughts, attitudes, and beliefs of pregnant women and their families.23 Media campaigns throughout the community can influence perceived benefits of avoiding the Zika virus using billboards, newspapers, radio, and posters.23,24 Accordingly, the health belief model and social cognitive theories also support the idea that media campaigns are an important component of influencing and changing human perception.16
Furthermore, in the Zika endemic area, one effective way to prevent transmission of the Zika virus is by preventing mosquito bites. For this reason, pregnant women and their partners should always be careful to try to prevent mosquito bites.23,24 They must follow prevention guidelines as regulated for general population.24 Efforts that can be made include: (1) using brightly colored clothes that cover as much as possible of all parts of the body; (2) using mosquito nets during sleep, whether day or night; (3) keeping potential places for mosquito breeding clean by draining and/or closing water reservoirs such as pots.
Most importantly, in areas where the Zika virus is present, pregnant women must have regular antenatal examinations and follow the advice given by health-care providers.21,24,25 Pregnant women who show symptoms or signs of Zika should have an early antenatal screening and perform continued proper screening and treatment. Moreover, national plans can target the polluted water and sewage with a water treatment and sanitation.24
This study has revealed some important factors related to Zika prevention practices by pregnant women in Thailand. However, one limitation of this study is that it only covered pregnant women who registered at the District Health Promotion Center; it did not cover those who received their pregnancy check-ups at the hospital, clinic, or private medical doctor’s office.
In conclusion, our findings confirmed that pregnant women have a low level of knowledge about Zika, and more importantly, that they have a moderate perception of Zika’s severity. This study also confirms that the perception of susceptibility to Zika is an important predictor of improving prevention practices around Zika transmission. These results provide evidence that the increased public perception about the severity of Zika can also improve mosquito control practices by the community. This finding is important for planning future prevention and health education interventions.
Conflicts of Interest
This study was funded by Kanchanabhishek Institute of Medical and Public Health Technology and the Ministry of Public Health. The sponsor gave a full authority to the researcher to collect, use, and publish the data. I can fully access and am responsible for the data and its analysis.
Acknowledgment
This research was supported by the Kanchanabhishek Institute of Medical and Public Health Technology and the Ministry of Public Health. The author would like to thank Dr. Sawanya Siriphakhamongkhon, Ms. Wannisa Raksamart, Mr. Chanawee Surachatri, and Mrs. Sarinthorn Mungkhamanee for assisting with collecting data.
REFERENCES
- Schuler-Faccini L, Ribeiro EM, Feitosa IM, Horovitz DD, Cavalcanti DP, Pessoa A, et al. Possible association between Zika virus infection and microcephaly — Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(3):59–62.
- Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects — reviewing the evidence for causality. N Engl J Med. 2016;374:1981–7.
- Frieden TR, Schuchat A, Petersen LR. Zika virus 6 months later. JAMA. 2016;316:1443–4.
- Binsaeed AA, Al-Hajri M, Noureldin EM, Farag E, Malik SM, Al-Zedjali MS, et al. Zika virus strategic response framework for the Gulf states 2016: an urgent need for collaboration. J Egypt Soc Parasitol. 2016;46(3):571–80.
- Polwiang S. The estimation of imported dengue virus from Thailand. J Travel Med. 2015;22(3):194–9.
- Wikan N, Suputtamongkol Y, Yoksan S, Smith DR, Auewarakul P. Immunological evidence of Zika virus transmission in Thailand. Asian Pac J Trop Med. 2016;9(2):141–4.
- Oliveira Melo AS, Malinger G, Ximenes R, Szejnfeld PO, Alves Sampaio S, Bispo de Filippis AM. Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the iceberg?. Ultrasound Obstet Gynecol. 2016;47(1):6–7.
- Pearson E, Punpuing S, Jampaklay A, Kittisuksathit S, Prohmmo A. The Mekong Challenge: Underpaid, Overworked and Overlooked: The realities of young migrant workers in Thailand: Volume One. International Labour Organization (ILO) & the Institute for Social and Population Research (IPSR), Mahidol University. 2006.
- World Health Organization. The Kingdom of Thailand Health System Review, Health Systems in Transition, World Health Organization Asia Pacific Observatory on Health Systems and Policies. Manila. 2015.
- World Desk Reference [Internet]. Thailand introduction. Bangkok: 2017 [cited 2017 June 28]. Available from: http://dev.prenhall.com/divisions/hss/ worldreference/TH/introduction.html/
- Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health [Internet]. Report on major diseases and health hazards Health zone 5. Bangkok: 2017 [cited 2017 June 28]. Available from: https:// odpc.ddc.moph.go.th/documents/1214115155.8282. pdf.
- Stretcher V, Rosenstock IM. The health belief model. Heal Behav Heal Educ Theory, Res Pract. 1997;31–6.
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–83.
- Busari OA, Olanrewaju TO, Desalu OO, Opadijo OG, Jimoh AK, Agboola SM, et al. Impact of patients‘ knowledge, attitude and practices on hypertension on compliance with antihypertensive drugs in a resource-poor setting. TAF Prev Med Bull. 2010;9(2):87–92.
- Petrie KJ, Weinman J. Patients’ perceptions of their illness: the dynamo of volition in health care. Curr Dir Psychol Sci. 2012;21(1):60–5.
- National Statistical Office Thailand [Internet]. Key Findings: The 2009 Reproductive Health Survey. Retrieved from: http://web.nso.go.th/en/survey/ reprod/data/rhs09_100810.pdf
- Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–10.
- Wong LP, Shakir SM, Atefi N, AbuBakar S. Factors affecting dengue prevention practices: nationwide survey of the Malaysian public. PLoS One. 2015;10(4):e0122890.
- Saunders M, Lewis P, Thornhill A. Research methods for business students. Selecting samples. Pearson Education, England. 2009:210–56.
- Petersen EE, Staples JE, Meaney-Delman D, Fischer M, Ellington SR, Callaghan WM, et al. Interim guidelines for pregnant women during a Zika virus outbreak — United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65(2):30–3.
- Whittemore K, Tate A, Illescas A, Saffa A, Collins A, Varma JK, et al. Zika virus knowledge among pregnant women who were in areas with active transmission. Emerg Infect Dis. 2017;23(1):164–6.
- Besnard M, Lastère S, Teissier A, Cao-Lormeau VM, Musso D. Evidence of perinatal transmission of Zika virus, Frensh Polynesia, December 2013 and February 2014. Euro Surveill. 2014;19(13):pii=20751.
- World Health Organization (WHO) [Internet]. Zika strategic response plan revised for July 2016–December 2017. [cited 2018 Jan 7]. Available from: http://apps. who.int/iris/bitstream/10665/246091/1/WHO-ZIKVSRF- 16.3-eng.pdf.
- New Mexico Department of Health. Zika Preparedness and Response Plan December 1, 2016 [Internet]. New Mexico Department of Health All-Hazard Emergency Operations Plan Functional / Hazard-Specific Annex. [cited 2018 Jan 7]. Available from: https://nmhealth. org/publication/view/plan/2230/.
- Buathong R, Hermann L, Thaisomboonsuk B, Rutvisuttinunt W, Klungthong C, Chinnawirotpisan P, et al. Zika strategic response plan, 2012-2014. Am J Trop Med Hyg. 2015;93:380–83.
Copyright @ 2018 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id