
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Community Research
Association of stature and mental problems among adolescents in Jatinangor District, West Java
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v27i3.2467 Med J Indones. 2018;27:209–12
Received: December 4, 2017
Accepted: July 18, 2018
Author affiliation:
1 Department of Child Health, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
2 Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
Corresponding author:
Meita Dhamayanti
E-mail: meita.dh@gmail.com
Background
The prevalence of short stature during adolescence in Indonesia remains high. Adolescents are very concerned about their stature. Most adolescent health problems are related to psychosocial issues. The prevalence of mental disorders among adolescents in Indonesia is 6.0%, and West Java is 9.3%. The aim of this study was to analyze the association between stature and mental problems during middle adolescence.
Methods
This analytical cross-sectional study was performed at three high schools in Jatinangor, West Java, Indonesia. The subjects were students, age of 16–17 years old without physical abnormalities other than short stature and weight problems. Mental problems were screened using a self-report Strength and Difficulties Questionnaire (SDQ). Data were analyzed using the chi-square test with prevalence risk.
Results
Of the 150 respondents, 116 subjects met the inclusion and exclusion criteria. The prevalence of short stature was 55 cases (47.4%) and more predominant in females. Among the behavioral and emotional problems assessed, the emotional symptom was associated significantly with short stature; prevalence ratio 1.87 (95% CI=1.14; 3.08). There was no significant association of short stature with other attributes such as conduct, hyperactivity, peer problems, and total difficulties (p>0.05).
Conclusion
Stature in adolescence is associated with emotional problems.
Keywords
adolescent, emotional, short stature
Adolescents are individuals with ages that range between 10–19 years old. Adolescence is one of the most important transitions in a person’s life, from childhood to young adulthood marked by tremendous growth and changes that occur quickly.1 The gaps between biophysical developments may affect psychological and emotional development. Adolescence is often divided into three sub-stages: early (10–14 years), middle (15–17 years), and late (>17 years) adolescence. Many health problems in young people have a psychosocial rather than a biological basis. Although mental health problems account for about 50% of the burden of illness in adolescence, some are mild and transitory. The World Health Organization (WHO) stated that 1 of 5 children aged <16 years, and 104 out of 1000 children aged 4–15 years had behavioral and emotional problems, and the incidence rate is even higher in the age group >15 years.2 In 2013, the Indonesian National Health Research reported that the prevalence of behavioral and emotional disorders in the population ≥15 years old is 6.0%, and in West Java, one of the provinces with the highest prevalence, was 9.3%.3
Stature is one factor affecting psychological problems in adolescents. Growth in stature is an essential determinant of wellbeing, which signifies increasing independence.4,5 Furthermore, short stature may have a negative effect on both an adolescent’s development and psychological functions.6 Short stature is defined as having a height below the third percentile, or as a height, that is 2 standard deviations (SDs) below the normal stature for both age and sex according to the population reference.7 WHO reported that the trend of short stature in the world is decreasing.8 In contrast, short stature is an important concern of public health in many developing countries. By 2020, it is predicted that 68 million children in Asia and 64 million children in Africa will be of short stature, respectively.8,9 In Indonesia, the prevalence of short stature in 590,570 families was 33.2%.10 Since short stature is assumed to impact young patients’ functioning and well-being, many studies have focused on middle adolescence. However, there are few researches on the effects of stature on mental problems in developing countries. This issue is critical as behavioral and emotional problems often persist into adulthood and may influence future cognitive and academic outcomes.
METHODS
This comparative cross-sectional study was conducted from September 2016 to June 2017 in the Jatinangor sub-district. Subjects were adolescents between the ages of 16 and 17 years in SMA Plus Al-Falah, SMA Swasta Darul Fatwa, and SMA Swasta Al- Ma’some. The convenient sampling method was used. Exclusion criteria were the presence of significant comorbidities (e.g., asthma), an inability to fill out questionnaires, as well as failure to obtain children assent, in addition, parental consent when required. A sample size of 150 students was needed based on calculation using two unpaired, independent proportions with the a value of 0.05, and the b value of 0.2. Convenient sampling was used in sample selection. A total of 116 students were eligible to participate.
The variables assessed in this study included stature, behavioral, and emotional problems. Stature is defined as height-for-age Z-score (HAZ) according to the WHO Growth Standard Chart, categorized into normal (Z-score≥2 SD) and abnormal (Z-score<2 SD). Height was determined by measuring standing height using a stadiometer with a fixed vertical backboard, and an adjustable headpiece. Data were calculated using WHO Anthro version 3.2.2 software to determine the HAZ. Behavioral and emotional problems were measured using the self-report Strength and Difficulties Questionnaire (SDQ). The SDQ is a behavioral and emotional screening questionnaire, which consists of 25 attributes divided into questions assessing total difficulties (emotional symptoms, hyperactivity/inattention, conduct problems, peer relationship problems), and questions assessing prosocial behavior. Results of the SDQ are categorized into normal, borderline, and abnormal.
The chi-square test was used to analyze categorical variables. Associations between behavioral problems, emotional problems, and height stature were tested by prevalence ratios (PRs). All analyses were performed using Statistical Package for Social Science (SPSS) version 22 software. Informed consent was obtained in accordance with the Declaration of Helsinki standards, and the ethical review committee of the Faculty of Medicine, Universitas Padjadjaran number 407/UN6.C.10/PN/2017 approved this study.
RESULTS
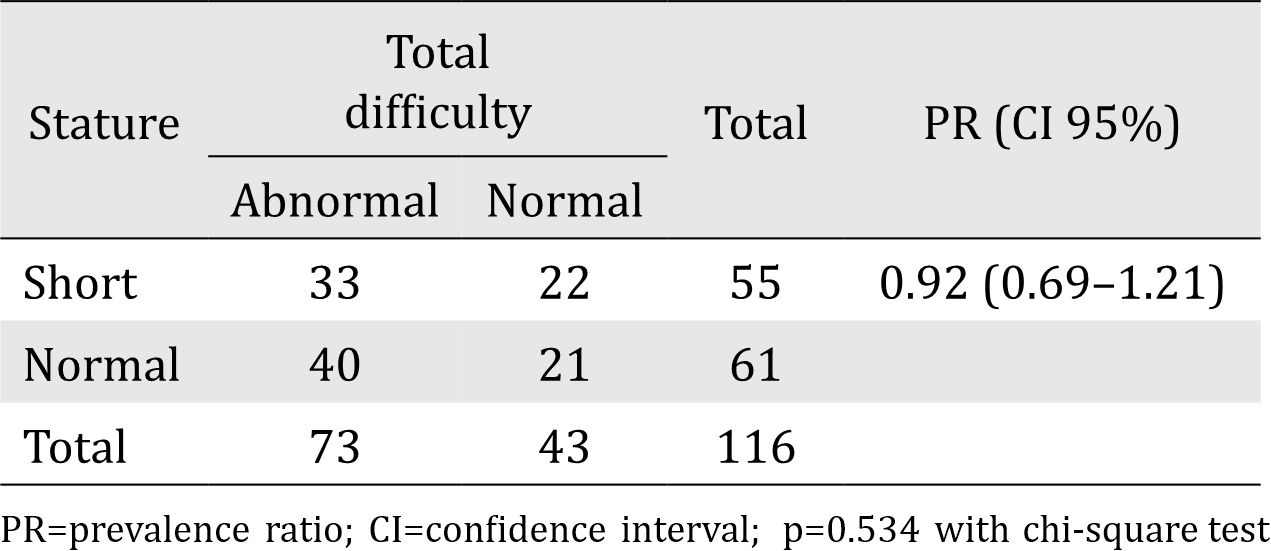
Of 116 participants, short stature was found in 55 (47%) students, 18 (33%) males, and 37 (67%) females (Table 1). There were no significant differences in characteristics such as gender, age, parental income, and the number of siblings by stature group. When compared with SDQ tests, problems related to conduct, hyperactivity/inattention, and peer relationships were not statistically associated, with PR and 95% confidence interval (CI) of 1.11 (0.54–2.26); 1.01 (0.71–1.42); 1.01 (0.83–1.23), respectively. However, emotional problems were significantly associated with a PR of 1.87 in short stature students, as shown in Table 2. This study also found that short stature had a significant association with total difficulties particularly regarding behavioral and emotional problems, as shown in Table 3.
Table 1. Distribution of subject characteristics based on stature
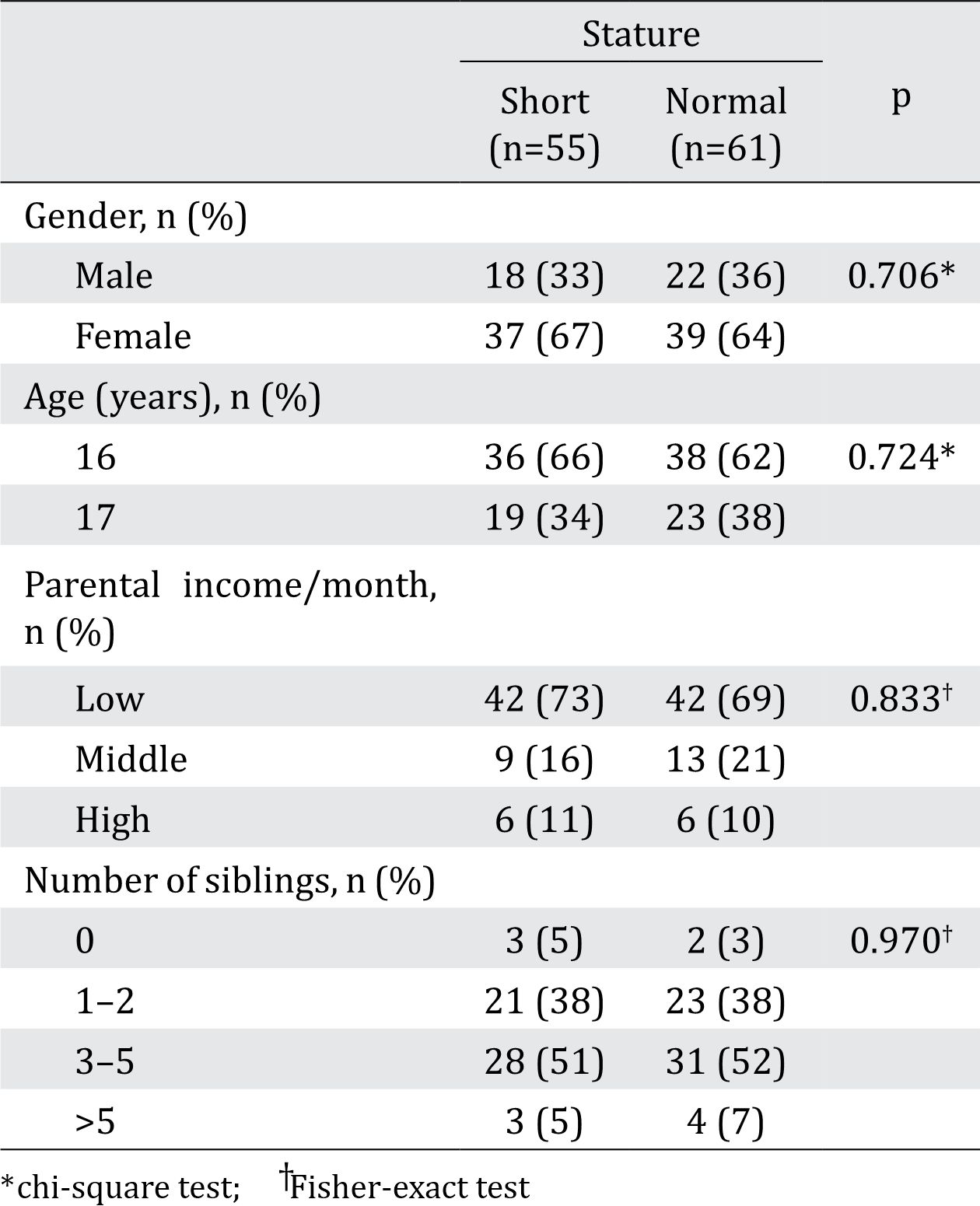
Table 2. Association of stature and emotional symptoms on the SDQ
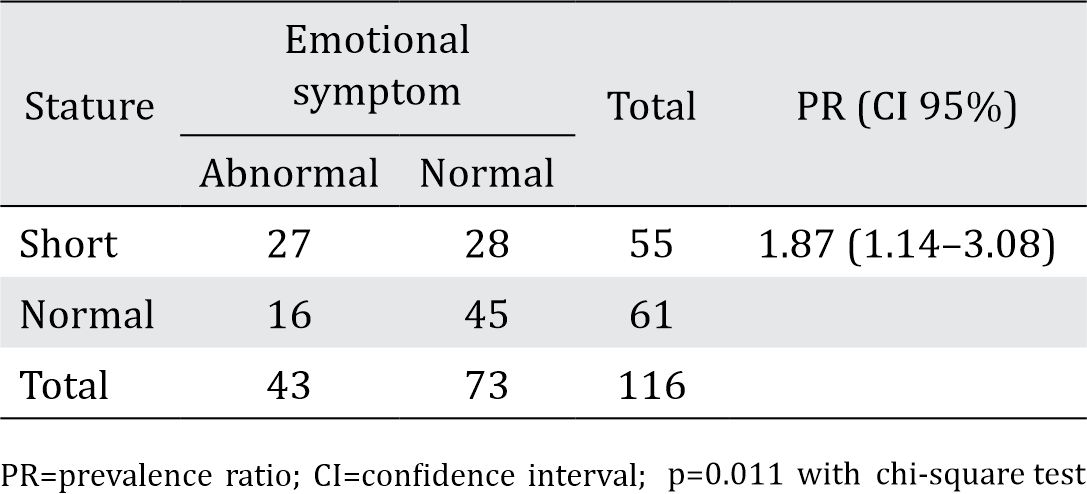
Table 3. Association of stature and total difficulty on the SDQ
DISCUSSION
This study found a significant association between short stature and emotional symptoms during middle adolescence. This finding is consistent with other studies, in which short stature has a negative influence on psychosocial functioning.11 Furthermore, adolescents with short stature are at a higher risk of mentally internalizing problems, which manifested as symptoms resembling physical illness, anxiety, unhappiness, and lack of self-confidence.5,12 Different studies have reported controversial findings regarding the association of height with social behaviors. One community-based study showed no differences in behaviors between short stature and normal children.13 However, the behavioral problem is dependent on the degree of short stature, and the ability of the individual to cope with their short stature.14
In this study, conduct, hyperactivity, and peer problems were not associated significantly with stature. Similar to the Chang et al no differences were found between short stature and non-stunted groups regarding the presence of hyperactivity and other emotional difficulties.15
The current study found that short stature was more prevalent among females when compared with male adolescents. However, this difference was not statistically significant. Jafari-Adli et al reported that the prevalence of short stature among Tehran students is both statistically and significantly higher in females (4.4%) when compared with males (2.8%), p<0.05.6 It is well established that the existence of early emotional problems in children may predict later mental issues, such as depression, when these individuals become adults. Stunted children, therefore, may be at risk for more serious social problems in adulthood.13
A limitation of this study is that the etiology of short stature was not examined further. Therefore, it is suggested that further research is conducted to classify short stature variables contained in the study based on etiology. In addition, the nature of the study design itself was a limitation since it had a cross-sectional study design and used self-reported data. Thus, it is advisable for subsequent research to use a qualitative approach to obtain in-depth details regarding the behavioral and emotional problems that adolescents face.
There is an association between stature and emotional symptoms during the middle of adolescence. The prevalence of emotional symptoms in mid-adolescents with short stature is higher than that in mid-adolescents with normal stature. However, there was no difference in the behavioral and emotional status between mid-adolescents with both short and normal stature based on conduct, hyperactivity, peer problems, and total difficulties.
Conflicts of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
This study was funded by Academic Leadership Grant of Universitas Padjadjaran.
REFERENCES
- Holland-Hall C, Burstein GR. Adolescent Development. In: Kliegman RM, Stanton BF, Schor NF, editors. Nelson Textbook of Pediatrics. 20th ed. Philadelphia: Elsevier; 2016. p. 926–36.
- WHO. Maternal, newborn, child and adolescent health. [Internet]. [cited 2016 Nov 11]. Available from: http:// www.who.int/maternal_child_adolescent/topics/ adolescence/dev/en/
- Balitbangkes Kemenkes RI. Riset Kesehatan Dasar: RISKESDAS 2013. [Internet]. Available from: http:// www.depkes.go.id/resources/download/general/ Hasil%20Riskesdas%202013.pdf.
- Deaton A. Height, health, and development. Proc Natl Acad Sci USA. 2007;104(33):13232–7.
- Quitmann J, Rohenkohl A, Specht A, Petersen-Ewert C, Schillmöller Z, Bullinger M. Coping strategies of children and adolescents with clinically diagnosed short stature. J Child Fam Stud. 2015;24(3):703–14.
- Jafari-Adli S, Qorbani M, Heshmat R, Ranjbar SH, Taheri E, Motlagh ME, et al. Association of short stature with life satisfaction and self-rated health in children and adolescents: the CASPIAN-IV study. J Pediatr Endocrinol Metab. 2016;29(11):1299–306.
- Ghai OP, Paul VK, A. B. Essential pediatrics. 7th ed ed. India: CBS Publishers and distributors Pvt. Limited. 2010.
- Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–60.
- de Onis M, Blössner M, Borghi E. Prevalence and trends of stunting among pre-school children, 1990-2020. Public Health Nutr. 2012;15(1):142–8.
- Semba RD, de Pee S, Sun K, Sari M, Akhter N, Bloem MW. Effect of parental formal education on risk of child stunting in Indonesia and Bangladesh: a cross-sectional study. Lancet. 2008;371(9609):322–8.
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177(6):534–9.
- Sommer R, Daubmann A, Quitmann J, Ravens-Sieberer U, Bullinger M. Understanding the impact of statural height on health-related quality of life in German adolescents: a population-based analysis. Eur J Pediatr. 2015;174(7):875–82.
- Kim B, Park MJ. The influence of weight and height status on psychological problems of elementary school children through child behavior checklist analysis. Yonsei Med J. 2009;50(3):340–4.
- Lee JM, Appugliese D, Coleman SM, Kaciroti N, Corwyn RF, Bradley RH, et al. Short stature in a population-based cohort: social, emotional, and behavioral functioning. Pediatrics. 2009;124(3):903–10.
- Chang SM, Walker SP, Grantham–McGregor S, Powell CA. Early childhood stunting and later behaviour and school achievement. J Child Psychol Psychiatry. 2002;43(6):775–83.
Copyright @ 2018 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id