
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
Progressive sperm motility is associated with spontaneous pregnancy after varicocelectomy
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v27i4.2636 Med J Indones. 2018;27:256–61
Received: February 6, 2018
Accepted: October 12, 2018
Author affiliation:
1 Department of Surgery, Faculty of Medicine, Universitas Udayana, Sanglah Hospital, Denpasar, Indonesia
2 Postgraduate Programme, Faculty of Medicine, Universitas Udayana, Denpasar, Indonesia
Corresponding author:
Pande M.W. Tirtayasa
E-mail: wisnu.tirtayasa@gmail.com
Background
Varicocelectomy is performed on patients with clinical varicocele associated with abnormal sperm parameters. The goal of this procedure is to improve men’s sperm parameters and pregnancy rates of their partners. The objective of our study was to assess the factors that were associated with spontaneous pregnancy in female partners after varicocelectomy
Methods
A retrospective case-control study was conducted to review several factors that are associated with spontaneous pregnancy after varicocelectomy. The data were taken from medical records at Sanglah General Hospital and three private hospitals in Denpasar from January 2015 to June 2016. Case subjects (n=38) include varicocele patients with abnormal sperm parameters whose partner had a spontaneous pregnancy following varicocelectomy and a control group (n=38) whose partner did not have a spontaneous pregnancy following varicocelectomy.
Results
Progressive sperm motility (≥37.5%) before varicocelectomy was 2.7 times more likely to result in a spontaneous pregnancy (odds ratio: 2.7; 95% confidence interval: 1.04–6.96; p=0.04). No statistical significance was found between age at varicocelectomy, grade of varicocele, body mass index, infertility duration, smoking habit, sperm concentration, normal sperm morphology before varicocelectomy, and spontaneous pregnancy.
Conclusion
Progressive sperm motility before varicocelectomy is a significant factor for the occurrence of spontaneous pregnancy after varicocelectomy.
Keywords
sperm motility, spontaneous pregnancy, varicocelectomy
Varicocele is an abnormal dilation of the pampiniform plexus and a potential cause of infertility in men.1 The incidence of varicocele is 4.4%–22.6% in the general population, which is composed of 15%–20% of men with primary infertility and 75%–81% with secondary infertility.2 Despite tremendous studies, the exact mechanism by which varicocele might induce male infertility has not been established, although some potential factors have been proposed. Moreover, previous studies showed that morphological abnormalities of sperm could result from blood stasis and accumulation of reactive oxygen species (ROS), nitric oxide, and other toxins.3
Varicocelectomy is a surgical approach performed on patients with clinical varicocele associated with abnormal sperm parameters. The main objective of this surgery is to improve sperm parameters in men and pregnancy rates of their partners.1,4 A meta-analysis study suggested that varicocelectomy showed an increase in sperm parameters ranging from 60% to 80%1 and in spontaneous pregnancy from 11.8% to 60%.5 Several different surgical techniques have been introduced to treat varicocele, and a number of studies have attempted to compare the outcomes of these techniques. Previous studies showed that varicocelectomy has a significant effect on improving total and progressive sperm motility as well as concentration after treatment regardless of techniques used,1,6 although one meta-analysis showed the superiority of microsurgical repair technique over open technique in terms of sperm motility.7 Microsurgical technique has been considered as a gold standard therapy for varicocele because it has fewer complications and lower recurrence rates compared with other techniques.1,6 On the other hand, different studies have reported controversial results regarding this issue. Therefore, various other techniques are still considered a reasonable option.1,6,8
Several studies have been conducted to study suspected factors affecting the incidence of spontaneous pregnancy after varicocelectomy. Those studies considered age at varicocelectomy, grade of varicocele, body mass index (BMI), duration of infertility, smoking habits, and sperm parameters before varicocelectomy as related to spontaneous pregnancy following varicocelectomy. However, all of them are still debatable until now. To date, there is no study that can determine a predictor for a successful spontaneous pregnancy after varicocelectomy in Indonesia. Thus, the aim of this study is to identify the predictor for a spontaneous pregnancy following varicocelectomy.
METHODS
A retrospective case-control study was conducted to review factors associated with spontaneous pregnancy after varicocelectomy. The data were taken from medical records at Sanglah Hospital and three private hospitals in Denpasar from January 2015 to June 2016. A simple random sampling method was used, and the minimum sample size calculated was 76. We divided the 76 cases evenly into two groups; case and control groups. Case samples (n=38) include patients with abnormal sperm parameters-associated varicocele whose partner had a spontaneous pregnancy after varicocelectomy, while the control group (n=38) includes patients whose partner did not have a spontaneous pregnancy after varicocelectomy. The samples of this study were infertile patients because of varicocele with abnormal sperm parameters, and where the varicocele was seen and palpable through clinical examination (clinical varicocele). All patients with varicocele were treated with bilateral varicocelectomy using a retroperitoneal approach or vasoligation varicocelectomy (Palomo technique). The study excluded infertile female partners examined by obstetricians, women using contraceptives before and during the study period, male and female couples suffering from a chronic systemic disease (diabetes mellitus and hypertension), and women who had a smoking habit.
BMI was determined using the World Health Organization (WHO) 2010 criteria. Meanwhile, the criteria for smoking are people who have smoked more than 100 cigarettes at least in the last 5 years. The sperm parameters before varicocelectomy included sperm concentration, progressive sperm motility (A+B), and normal sperm morphology based on the WHO 1999 criteria. The study also considered female factors as confounding variables including age, BMI, and occupation, which were included in the statistical analysis. Some of the variables were categorical, while some were numerical. However, all of the variables were categorized and divided into two groups based on previous studies.9–11 The cutoff point for sperm parameters (concentration, motility, and morphology) was the median of all samples to obtain a similar number between the two groups. Statistical analysis used bivariate and multivariate tests of logistic regression to determine the factors that significantly affect the occurrence of spontaneous pregnancy after varicocelectomy, using p-value <0.05 with 95% confidence interval (CI). All the analyses in this study used Statistical Product and Service Solutions (SPSS) version 19. This study has been approved by the Ethical Committee of Faculty of Medicine, Universitas Udayana/Sanglah General Hospital No: 1401/UN.14.2/KEP/2017.
RESULTS
The characteristics of the sample based on the case and control groups are shown in Table 1. Bivariate analysis identified four variables with a p-value <0.25, that is, infertile duration, progressive sperm motility before varicocelectomy, female age, and female in employment. These variables were assessed further using multivariate analysis (Table 1).
Table 1. The characteristics of the samples and analysis between independent and confounding variables with the occurrence of spontaneous pregnancy after varicocelectomy
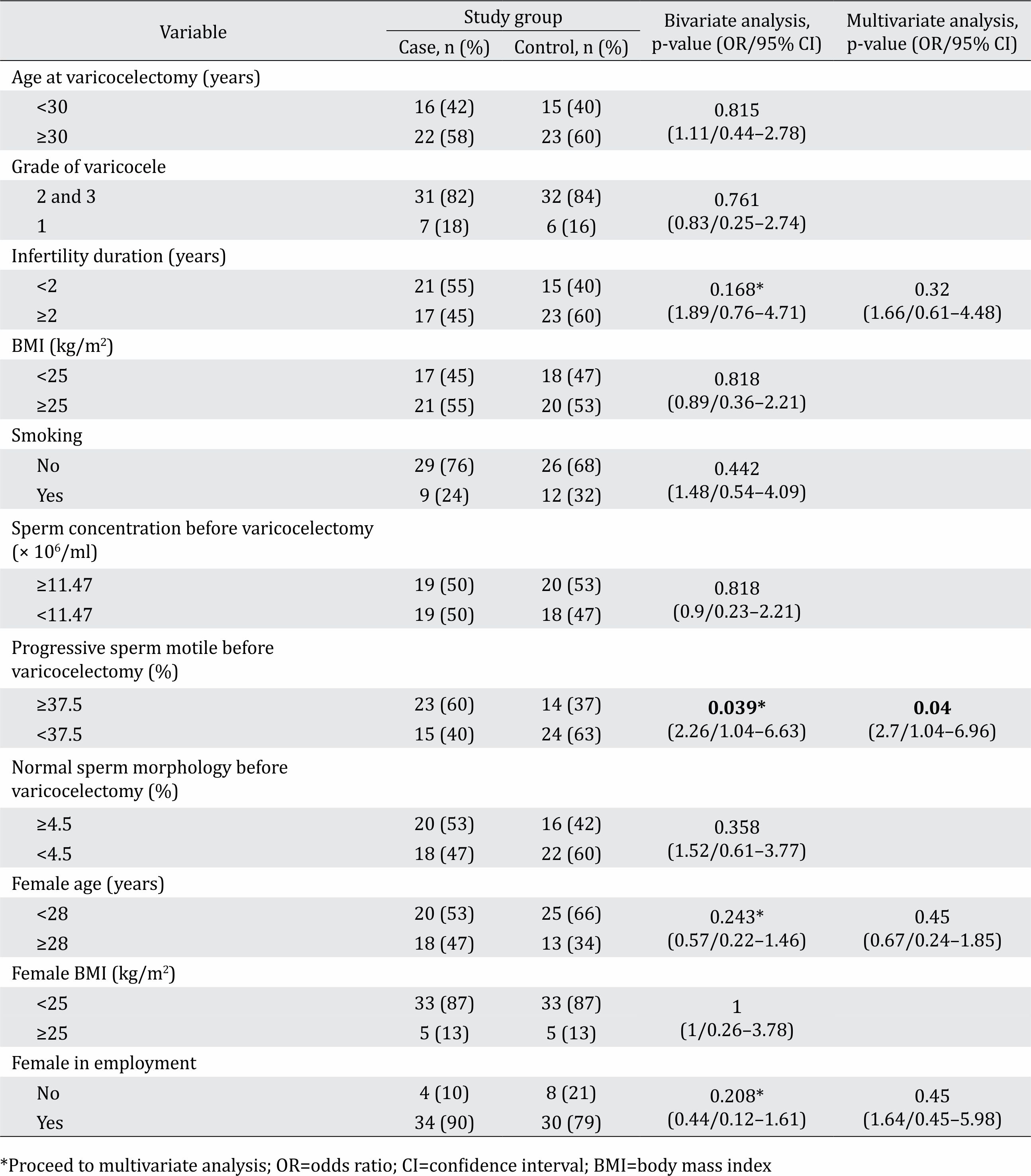
Multivariate analysis showed that only progressive sperm motility before varicocelectomy had a significant association with spontaneous pregnancy after varicocelectomy. Progressive sperm motility before varicocelectomy (≥37.5 %) was 2.7 times more likely to result in a spontaneous pregnancy after varicocelectomy.
DISCUSSION
Several factors can affect the occurrence of spontaneous pregnancy after varicocelectomy, such as the age at varicocelectomy, grade of varicocele, BMI, the duration of infertility, smoking habits, and sperm parameters before varicocelectomy. Nevertheless, previous studies showed different results, and none of those factors were proven to have a significant effect on spontaneous pregnancy.9–13 This study was conducted to determine the predictor for a successful spontaneous pregnancy after varicocelectomy.
The association of age at varicocelectomy with spontaneous pregnancy resulted in OR: 1.11; 95% CI 0.44–2.78; p=0.815. This suggested that the age at varicocelectomy was not associated with spontaneous pregnancy. Similar results were obtained in previous studies suggesting that there was no significant difference in the occurrence of spontaneous pregnancy after varicocelectomy between age groups.14,15 However, the elimination of age as a confounder was found in this study since all men were between 23 and 39 years old and women younger than 35 years old. Abdel-Meguid et al14 in a previous study also limited their study to couples with men between 20 and 39 years old and women below 35 years old to eliminate age as a confounder and abolish the controversies regarding outcomes of varicocelectomy in younger and older age groups.
The grade of varicocele seemed to play a role in sperm ROS levels. The greater the grade, the higher ROS levels reported, which can also decrease sperm concentration. According to The Guidelines on Male Infertility, Ikatan Ahli Urologi Indonesia 2015, varicocele grades 2 and 3 were two of the factors that might influence the success of varicocelectomy.11 High-grade varicocele tends to have poor sperm parameters. However, this group would acquire more improvement in sperm parameters compared with low-grade varicocele groups following varicocelectomy. Based on this consideration, we put varicocele grades 2 and 3 as one group to represent high-grade varicocele. In bivariate analysis related to the grading of varicocele, this study showed a p-value=0.761. This suggested that the grade of varicocele did not significantly affect spontaneous pregnancy after varicocelectomy. Our finding was in line with previous studies conducted by Abdalla et al12 and Abdel-Meguid et al.14
BMI studies have been associated with the occurrence of varicocele.15,16 Nonetheless, there were limited data in the literature on the association of BMI with the occurrence of spontaneous pregnancy after varicocelectomy. The increase of BMI would affect the occurrence of systemic oxidative stress and also contribute to an endocrine imbalance in the hypothalamic-pituitary-gonadal axis that decreases testosterone levels. In this study, bivariate analysis showed that a BMI of <25 kg/ m2 was not significantly related to spontaneous pregnancy after varicocelectomy (p=0.818). Pham and Sandlow reported that varicocelectomy in overweight and obese patients produced the same result compared with normal weight patients.17
Multivariate analysis based on infertility duration of <2 years was also performed (OR 1.66; 95% CI 0.61–4.48; p=0.32). The results suggested that the duration of infertility of <2 years was not associated with the occurrence of spontaneous pregnancy after varicocelectomy. The same result was also presented by Zorba et al18 who examined the effect of infertility duration on spontaneous pregnancy after varicocelectomy. They found that spontaneous pregnancy correlated negatively with the duration of infertility and this could support the perspective that varicocele has detrimental effects on the testicular biology over time.
Smoking habits in patients with varicocele will cause high levels of cadmium (Cd) in sperm. Cd has a negative effect on spermatogenesis and increases the production of ROS.19–21 Bivariate analysis regarding smoking habits showed p=0.442. This implied that a smoking habit was not significantly related to spontaneous pregnancy after varicocelectomy. Bivariate and multivariate analyses revealed that progressive sperm motility before varicocelectomy (≥37.5%) was the only factor associated with spontaneous pregnancy after varicocelectomy (OR 2.7; 95% CI 1.04–6.96; p=0.04). This result was consistent with the previous studies. According to Peng et al22 and Shabana et al,23 sperm motility prior to varicocelectomy was associated with spontaneous pregnancy. After varicocelectomy, the drop of testicular venous hydrostatic pressure, reflux of toxic metabolites, and testicle temperature will improve the function of Leydig and Sertoli cells and eventually sperm motility. A study, which tested the ability of sperm motility to penetrate the cervical mucus in vitro using a cervical mucus penetration test to obtain sperm motility, reported a very important role for the occurrence of pregnancy, especially in its ability to penetrate in the cervical mucus.24 This study found that sperm concentration (p=0.818) and normal sperm morphology before varicocelectomy (p=0.358) did not induce spontaneous pregnancy after varicocelectomy. Statistical analysis of a female partner including age, BMI, and female in employment showed that none of these factors were related to spontaneous pregnancy after varicocelectomy.
Several different techniques have been introduced to treat varicocele, including high ligation of the testicular vein through a retroperitoneal approach above the internal inguinal ring (Palomo technique); ligation of the cremasteric and internal spermatic veins as they travel through inguinal canal (Ivanissevich technique); use of a microscope to spare lymphatics and arteries while ligating spermatic veins within the inguinal canal or below the external inguinal ring (inguinal or sub-inguinal microsurgical techniques, respectively); and retrograde embolization or sclerotherapy under radiographic guidance.1 The comparison of these different techniques has been attempted in many studies regarding their effect on sperm quality and pregnancy rates.6,7,13,25 Previous studies showed that varicocelectomy has a significant effect on improving total and progressive sperm motility as well as concentration after treatment regardless of techniques used.1,6 In addition, the microsurgical technique has proven its superiority among all techniques particularly in complications and recurrence rates and is considered as a gold standard in treating varicocele.1 However, this technique might require microsurgical training, and many centers do not have microscopes, like most of our centers in Bali. Therefore, the various other techniques are still considered as an option. Taken altogether, there would be no significant difference among all techniques in terms of sperm quality and pregnancy rates after the therapy. We used the Palomo technique in this study because we were familiar with it.
We utilized the Palomo technique because most of our centers did not provide a microscope that is required to perform microsurgical technique at the time this study was conducted, and this issue was the limitation of this study. Therefore, it is more sensible to arrange a multicenter study in the future, which use a gold standard technique such as microsurgical to obtain more reliable results.
In conclusion, the progressive sperm motility before varicocelectomy was positively associated with the occurrence of spontaneous pregnancy after varicocelectomy. None of the other factors such as the age at varicocelectomy, grade of varicocele, BMI, infertile duration, smoking habit, sperm concentration, and normal sperm morphology before varicocelectomy were correlated with spontaneous pregnancy after varicocelectomy.
Conflicts of Interest
The authors confirm no conflict of interest in this study.
Acknowledgment
None.
REFERENCES
- Baazeem A, Belzile E, Ciampi A, Dohle G, Jarvi K, Salonia A, et al. Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol. 2011;60(4):796–808.
- Reddy SV, Shaik AB, Sailaja S, Venkataramanaiah M. Outcome of varicocelectomy with different degrees of clinical varicocele in infertile male. Adv Androl. 2015;2015:432950.
- Miyaoka R, Esteves SC. A critical appraisal on the role of varicocele in male infertility. Adv Urol. 2012;2012:597495.
- Shridharani A, Owen R, Elkelany OO, Kim ED. The significance of clinical practice guidelines on adult varicocele detection and management. Asian J Androl. 2016;18(2):269–75.
- Kumar R, Sekar H, Krishnamoorthy S, Kumaresan N, Ramanan V. Analysis of outcomes of surgical treatment for varicocele in primary infertility based on seminal parameters and pregnancy rate. IJSS. 2016;4(4):205–10.
- Hosseini K, Nejatifar M, Kabir A. Comparison of the efficacy and safety of Palomo, Ivanissevich and laparoscopic varicocelectomy in Iranian infertile men with palpable varicocele. Int J Fertil Steril. 2018;12(1):81–7.
- Yuan R, Zhuo H, Cao D, Wei Q. Efficacy and safety of varicocelectomies: a meta-analysis. Syst Biol Reprod Med. 2017;63(2):120–9.
- Ding H, Tian J, Du W, Zhang L, Wang H, Wang Z. Open non-microsurgical, laparoscopic or open microsurgical varicocelectomy for male infertility: a meta-analysis of randomized controlled trials. BJU Int. 2012;110(10):1536–42.
- Reşorlu B, Kara C, Sahin E, Unsal A. The significance of age on success of surgery for patients with varicocele. Int Urol Nephrol. 2010;42(2):351–6.
- Liguori G, Ollandini G, Pomara G, Amodeo A, Bertolotto M, Mazzon G, et al. Role of renospermatic basal reflow and age on semen quality improvement after sclerotization of varicocele. Urology. 2010;75(5):1074–8.
- Duarsa GWK. Varikokel. In: Duarsa, GWK. Guidelines of Male Infertility. Jakarta: Ikatan Ahli Urologi Indonesia; 2015. p. 33–5. Indonesian.
- Abdalla A, Amin A, Hamdy A, Nady M. Spontaneous pregnancy outcome after surgical repair of clinically palpable varicocele in young men with abnormal semen analysis. Afr J Urol. 2011;17(4):115–21.
- Simforoosh N, Ziaee SA, Behjati S, Beygi FM, Arianpoor A, Abdi H. Laparoscopic management of varicocele using bipolar cautery versus open high ligation technique: a randomized, clinical trial. J Laparoendosc Adv Surg Tech A. 2007;17(6):743–7.
- Abdel-Meguid T, Al-Sayyad A, Tayib A, Farsi HM. Does varicocele repair improve male infertility? an evidencebased perspective from a randomized, controlled trial. Eur Urol. 2011;59(3):455–61.
- Gokce A, Demirtas A, Ozturk A, Sahin N, Ekmekcioglu O. Association of left varicocoele with height, body mass index and sperm counts in infertile men. Andrology. 2013;1(1):116–9.
- Rais A, Zarka S, Derazne E, Tzur D, Calderon-Margalit R, Davidovitch N, et al. Varicocoele among 1 300 000 Israeli adolescent males: time trends and association with body mass index. Andrology. 2013;1(5):663–9.
- Pham KN, Sandlow JI. The effect of body mass index on the outcomes of varicocelectomy. J Urol. 2012;187(1):219–21.
- Zorba UO, Sanli OM, Tezer M, Erdemir F, Shavakhabov S, Kadioglu A. Effect of infertility duration on postvaricocelectomy sperm counts and pregnancy rates. Urology. 2009;73:767–71.
- Collodel G, Capitani S, Iacoponi F, Federico MG, Pascarelli NA, Moretti E. Retrospective assessment of potential negative synergistic effects of varicocele and tobacco use on ultrastructural sperm morphology. Urology. 2009;74(4):794–9.
- Fariello RM, Pariz JR, Spaine DM, Gozzo FC, Pilau EJ, Fraietta R, et al. Effect of smoking on the functional aspects of sperm and seminal plasma protein profiles in patients with varicocele. Hum Reprod. 2012;27(11):3140–9.
- Taha EA, Ezz-Aldin AM, Sayed SK, Ghandour NM, Mostafa T. Smoking influence on sperm vitality, DNA fragmentation, reactive oxygen species and zinc in oligoasthenoteratozoospermic men with varicocele. Andrologia. 2014;46(6):687–91.
- Peng J, Zhang Z, Cui W, Yuan Y, Song W, Gao B, et al. Spontaneous pregnancy rates in Chinese men undergoing microsurgical subinguinal varicocelectomy and possible preoperative factors affecting the outcomes. Fertil Steril. 2015;103(3):635–9.
- Shabana W, Teleb M, Dawod T, Elsayed E, Desoky E, Shahin A, et al. Predictors of improvement in semen parameters after varicocelectomy for male subfertility: a prospective study. Can Urol Assoc J. 2015;9(9– 10):E579–82.
- Björndahl L. The usefulness and significance of assessing rapidly progressive spermatozoa. Asian J Androl. 2010;12(1):33–5.
- Al-Said S, Al-Naimi A, Al-Ansari A, Younis N, Shamsodini A, A-sadiq K, et al. Varicocelectomy for male infertility: a comparative study of open, laparoscopic and microsurgical approaches. J Urol. 2008;180(1):266–70.
Copyright @ 2018 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id