
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Clinical Research
Urinary tract infection profile among a hospitalized newborn: a single center study in Iran, 2006-2015
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v27i2.2677 Med J Indones. 2018;27:94–100
Received: February 27, 2018
Accepted: June 28, 2018
Author affiliation:
Department of Pediatrics, Hamedan University of Medical Sciences, Hamedan, Iran
Corresponding author:
Behnaz Basiri
E-mail: behnazbasiri@yahoo.com
Background
Urinary tract infection in infants is associated with septicemia and genitourinary anomalies. This study was aimed at investigating the frequency, clinical signs, and anomalies in infants hospitalized for urinary tract infection.
Methods
This cross-sectional study was conducted on all infants with urinary infection who were hospitalized in the neonatal ward of Be’sat Hospital from 2006 to 2015.
Results
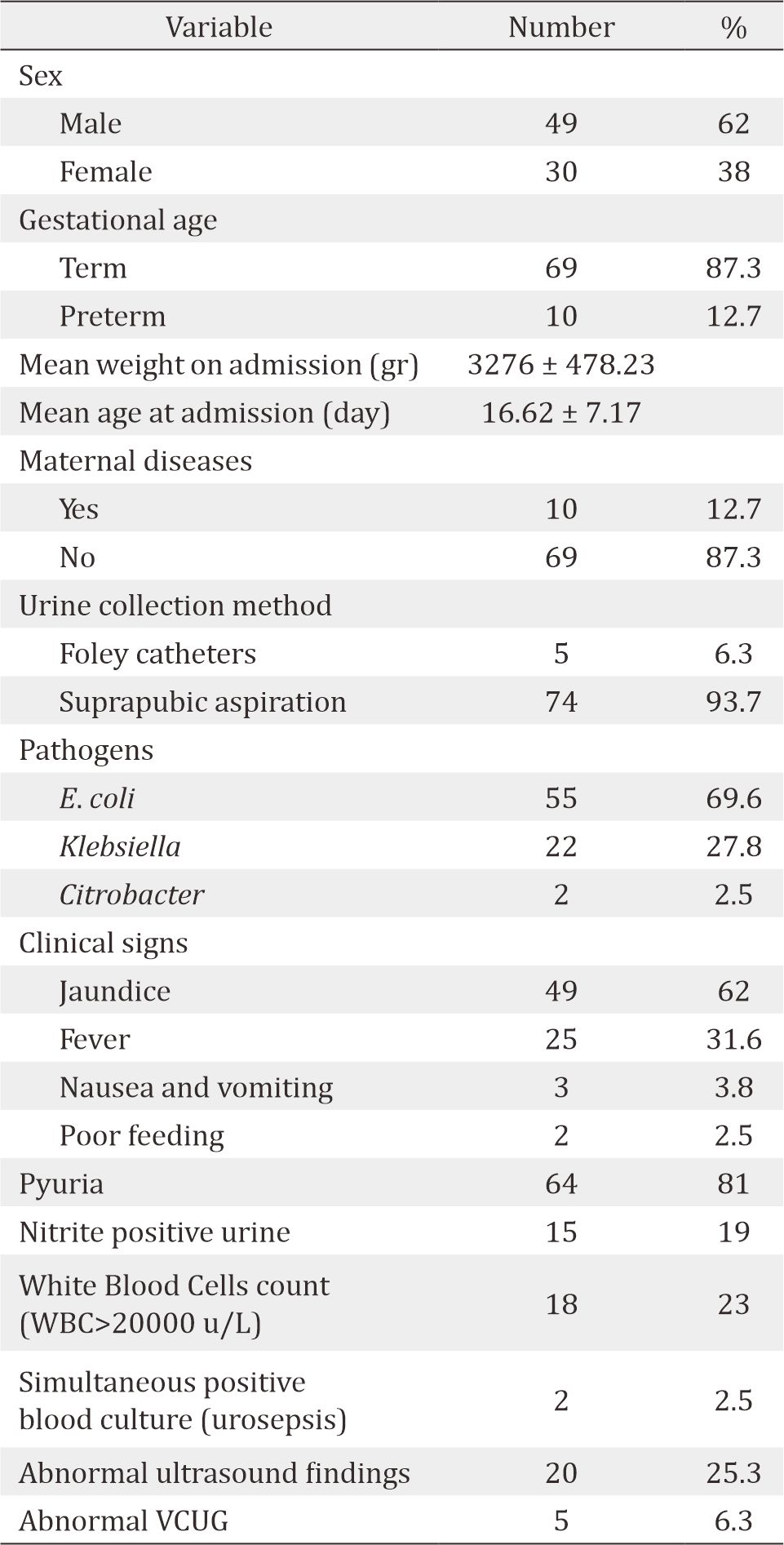
Of 79 infants with urinary infection, 62% were male and 87.3% were term infants. The mean age at admission was 16.62±7.17 days, and the mean weight was 3276±478.23 grams. The most frequent clinical sign and the most common pathogen reported were prolonged jaundice (62%) and Escherichia coli (69.6%), respectively. Of the samples, 93.7% were obtained by suprapubic aspiration, 23% had leukocytosis, and 2.5% had urosepsis. In urinalysis examination, 81% had pyuria and 19% had positive nitrate. Among 25.3% infants who had abnormal ultrasound findings, the most abnormal finding was mild bilateral hydronephrosis and 6.3% of the infants had abnormal voiding cystourethrogram (VCUG) in which vesicoureteral reflux was the most frequent finding.
Conclusion
It showed that a prolonged jaundice in infants should be considered as a strong factor predicting urinary tract infection.
Keywords
clinical signs, neonates, type of organism, urinary tract infection
Urinary tract infection (UTI) is one of the most frequent infections among infants. General prevalence of UTI among infants is 0.1–10% which is 0.1–1% in term infants and up to 10% in preterm infants.1 Urinary infection usually occurs during the second and third week after the birth of term infants. UTI during the initial days after the birth is a few even in infants with bacteremia.2 E. coli is the most frequent pathogen reported among term infants, and it constitutes 80% of the causes of the infection. Other gram-negative bacteria that cause urinary infection such as Klebsiella, Proteus, Enterobacter, and Citrobacter. Gram-positive bacteria include coagulase-negative Staphylococcus, Enterococcus, and Staphylococcus aureus.3
The signs and symptoms of urinary infection in infants are non-specific and include fever in 20–40%, growth failure in 15–42%, jaundice in 3–41%, vomiting in 9–4%, and diarrhea in 3–5%.4 Prematurity, low birth weight, uncircumcised, and urinary tract anomalies are the most important risk factors of urinary tract infection in infants.5-7 Diagnosis of urinary tract infection is based on positive urine cultures obtained from suprapubic samples or bladder catheter, in which suprapubic aspiration of bladder is the most reliable technique of diagnosis.8,9 UTI in infants is very important because it has no specific signs.
Furthermore, there is a possibility of urinary tract abnormalities as a background of the disease. If these abnormalities were untreated, they will lead to a long-term complication such as high blood pressure and kidney failure. Considering the significance of the aforementioned facts, this study was aimed at investigating the prevalence, clinical signs, and anomalies in infants hospitalized for UTI.
METHODS
This study was carried out in a retrospective and descriptive cross-sectional method in all infants who were hospitalized from 2006 to 2015 in the neonatal ward of Be’sat Hospital in Hamedan due to UTI. The variables included the age, sex, weight at admission, gestational age, clinical signs, method of obtaining urine samples, laboratory results, imaging and ultrasound findings, and the mean duration of treatment until negative urine culture. UTI was defined if there was any number of microorganisms in suprapubic samples or more than 1,000 microorganisms in unit samples of urine obtained by catheters. Complete information of all the infants was extracted from the hospitalized profiles, and they were recorded in a separate questionnaire. Results of complete blood count (CBC), blood culture, ultrasound findings, and VCUG of the urinary system were also recorded in a predesigned list.
Ethical consideration
The study has been approved by the Ethics Committee of Hamedan University of Medical Science, No. P/4201/9/35/14.
Statistical analysis
All the collected data were analyzed based on chi-square and two-independent-samples t-test using Statistical Package for the Social Sciences (SPSS) 19. In all the aforesaid tests, the significance level was less than 0.05.
Table 1. Characteristics of infants with urinary tract infection
RESULTS
Out of 3,291 infants admitted to the neonatal ward during the study period, 79 (2.3%) infants had urinary tract infection. The most frequent clinical sign and the most frequent organism causing the infection were prolonged jaundice (62%) and E. coli (69.6%), respectively. Of the samples, 93.7% were provided by suprapubic aspiration, 23% had leukocytosis above 20,000 u/L, and 2.5% had positive blood culture similar to organisms causing urinary infection. Among infants, 25.3% had abnormal ultrasound findings. The most abnormal finding was mild bilateral hydronephrosis, and 6.3% of the infants had abnormal VCUG in which vesicoureteral reflux was the most frequent finding.
DISCUSSION
UTI is one of the most important clinical problems in infancy that early diagnosis and appropriate treatment are very important because if the infection is untreated, it will lead to high blood pressure, recurrent infections, and kidney failure.10,11 This study showed that the most frequent clinical signs in infants with urinary tract infection were prolong jaundice, fever, nausea and vomiting, and poor feeding, respectively. In Nickavar’s study,12 the most frequent signs were jaundice, irritability, poor feeding, vomiting, lethargy, fever, and tachypnea. Hosseini et al13 found that the most frequent signs were jaundice, irritability, poor feeding, lethargy, vomiting, fever, tachypnea, and diarrhea. The results of this study were consistent with the aforementioned studies. Although fever was the most frequent sign of urinary tract infection among infants in the study conducted by Youssef et al11 and Littlewood et al,14 it seems that prolonged jaundice had been a clue to evaluate the infants for urinary tract infection.
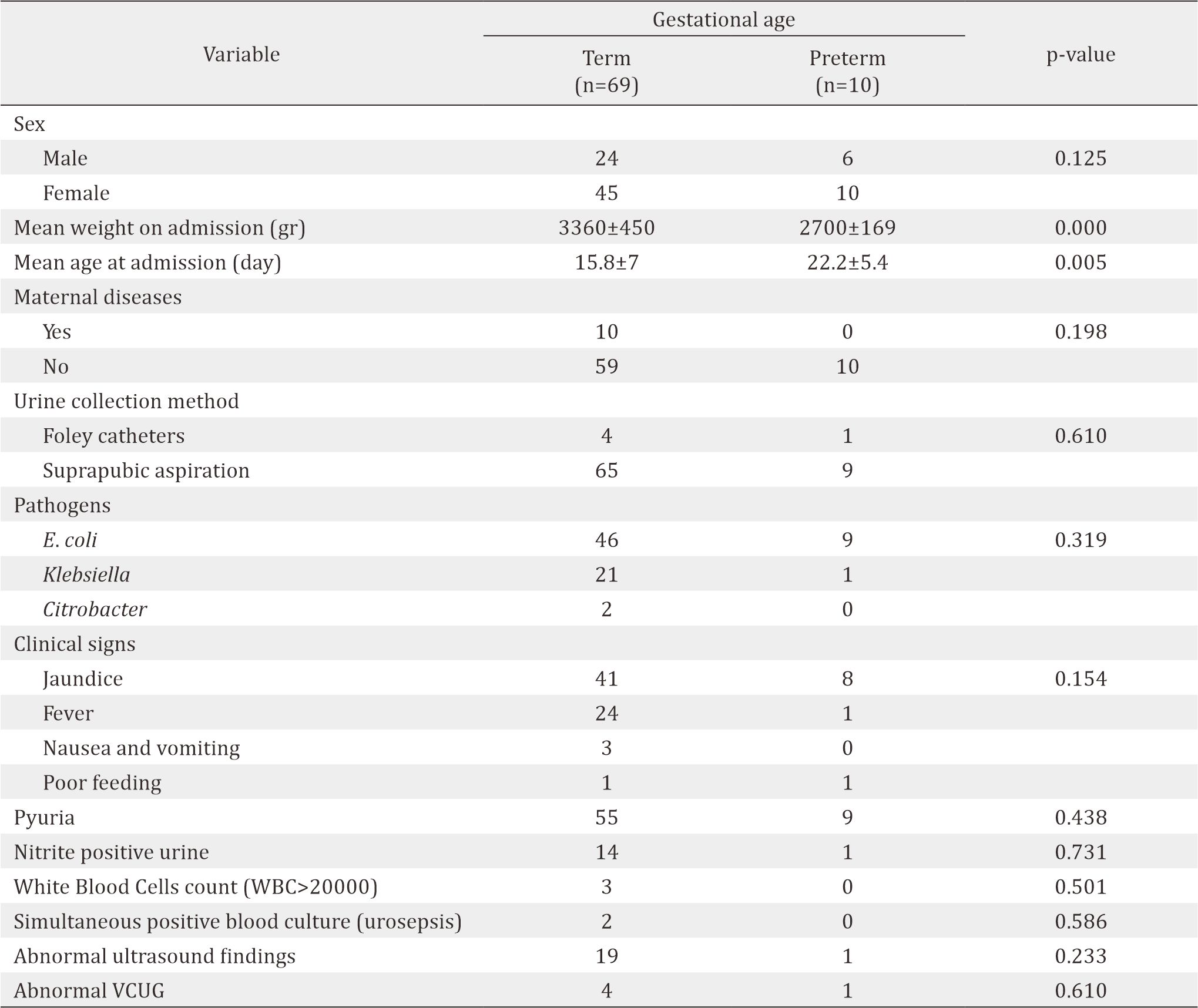
The majority of the infants in this study were male although there was no statistically significant difference between the sexes, which was consistent with the findings of studies conducted by Nickavar et al,12 Bonadio et al,3 Sharif et al,15 Khalesi et al,16 and Hematyar et al,17 as 75%, 73%, 68%, 60%, and 58%, respectively. UTI is more common in male infants, especially uncircumcised male compared to female infants, whereas at higher age, urinary tract infection is more common in females.18 Our study showed that there was no significant relationship between maternal diseases and urinary tract infection in infants, which was consistent with the study of Hemmatyar et al15 and Garcia et al4 However, the study conducted by Youssef et al11 was associated with premature rapture of membrane.
In this study, 97.3% of the urine culture samples had been obtained by suprapubic aspiration which was the standard method for providing urinal cultures, and it was consistent with the findings of other studies.19 The initial laboratory tests in infants with urinary tract infection included a complete blood count and urinalysis. However, these tests were not sensitive enough to detect urinary tract infection.20 In Bonadio’s study,3 40% of infants had peripheral blood leukocytosis, and urine dipstick was positive for leukocyte esterase and/or nitrate in 79% of cases. This study also showed that 23% of the infants had peripheral blood leukocytosis which was similar to the study previously mentioned. Moreover, the differences in amounts were due to the fact that in this study, leukocytosis was considered to be higher than 20.000 u/L and in Bonadio’s study,3 it was higher than 15.000 u/L. In the study conducted by Nickavar et al,12 27.5% of infants had leukocytosis higher than 13.000 u/L.
In the present study, 2.5% of the infants had positive blood cultures with the same pathogen of urinary tract infection (E. coli). Downey et al21 found that the incidence was 13% which was more than the findings of this study and the reason for it lied in investigating preterm infants; however, in the current study, most of the infants were term, and it was clarified that simultaneous prevalence of sepsis in preterm infants was more than that in term infants. In the study conducted by Bonadio et al,3 4% of infants with urinary tract infection had positive simultaneous blood cultures which were consistent with the findings of the present study. None of the infants with urinary infection had positive simultaneous blood cultures in the study carried out by Hosseini et al13 and Nickavar et al.12
Table 2. Comparison of infant's characteristics with ultrasound findings
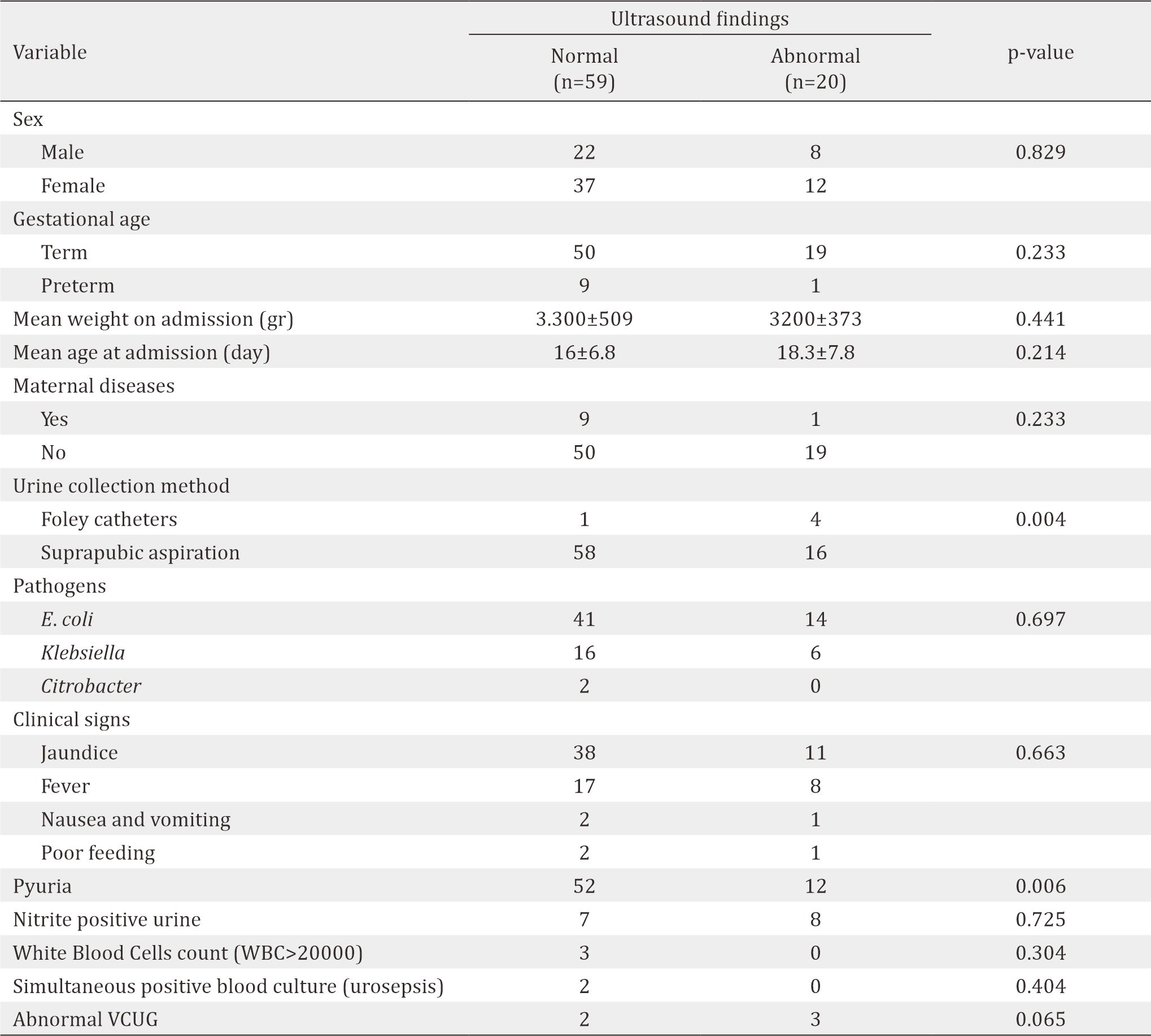
Urinary tract abnormalities were observed in 25%–50% of infants and children with urinary tract infection, and the most frequent abnormalities were mild hydronephrosis and pelvis ectasia.22,23 Major abnormalities like severe hydronephrosis and vesicoureteral reflux were observed in 5%–10% of infants with urinary tract infection.18 In the present study, 25.3% of the infants had abnormal ultrasound findings, in which the most frequent one was mild hydronephrosis. In VCUG, 6.3% had abnormalities, and the most frequent one was mild bilateral vesicoureteral reflux. In the study of Boskabadi et al,24 32% of the infected infants had abnormal ultrasound findings, and 50% of them had vesicoureteral reflux. Hosseini et al13 reported that 40% of the infants had abnormal ultrasound findings, and 20% of them had abnormalities in VCUG. Sastre et al25 showed that 37.1% of the infants had abnormalities in ultrasound, and 20% of the infants had abnormalities in VCUG. Bonadio et al3 also reported 47% had ultrasound abnormalities, with the most frequent one being mild hydronephrosis. Nickavar et al12 found that 37.5% of the infants had abnormal finding, with the most frequent one being mild hydronephrosis which shows the consistency of the present study with the findings and sources in other studies.
In this study, the most frequent organisms causing urinary infection were E. coli, Klebsiella, and Citrobacter, respectively. Moreover, in the study carried out by Hosseini et al13 the most frequent organisms causing urinary infection were E. coli, Klebsiella, Enterobacter, and Citrobacter, respectively. Bonadio et al,3 found that the most frequent organisms causing urinary infection were E. coli, Klebsiella, and Enterococcus. In Nickavar’s study,12 the organisms causing the infection were E. coli, Klebsiella, Enterobacter, and Enterococcus, respectively. In the study conducted by Hematyar et al,17 Khalesi et al,16 Eghbalian et al,26 Huang et al,27 and Crain et al,28 the most frequent cause of infection was E. coli which was consistent with the findings of the present study.
Table 3. Comparison of infant's characteristics with gestational age group
Although urinalysis on adult predicts urinary infection, it is not sensitive and specific enough to diagnose urinary tract infection in infants.29 In the present study, 81% of the infants had pyuria in their urine test, and 19% had positive nitrate. In the study conducted by Rahman et al,30 71.4% of the infants with urinary infection had pyuria in their urine test. Bonadio et al3 found that the amount of leukocyte esterase and positive nitrate in urine dipstick test was 79%. In the study by Bachur et al,31 which studied the sensitivity and specificity of urine analysis test in detecting urinary tract infection, the levels of sensitivity and specificity were 82% and 92%, respectively. Hosseini et al13 reported that 85% of the infants with urinary tract infection had pyuria in their urine test. Boskabadi et al24 showed that leukocyturia and/or bacteriuria were observed in 60% of the infants with urinary infection.
The limitation of our study was the small number of cases. This might be due to the low incidence of the urinary tract infection in infants. However, this study can be a baseline for an epidemiology of UTI in infants in Iran.
In conclusion, the incidence of UTI in infants is low, with E. coli as the most frequent pathogen. A prolonged icterus is the most frequent sign of urinary infection in infants.
Conflicts of Interest
Acknowledgment
This research has been adapted from Mr. Doctor Ali Alahgholi’s thesis. We are very grateful for his efforts and Neonatal Intensive Care Unit respected staff.
REFERENCES
- Bagga A, Tripathi P, Jatana V, Hari P, Kapil A, Srivastava RN, et al. Bacteriuria and urinary tract infections in malnourished children. Pediatr Nephrol. 2003;18(4):366–70.
- Riskin A, Toropine A, Bader D, Hemo M, Srugo I, Kugelman A. Is it justified to include urine cultures in early (<72 hours) neonatal sepsis evaluations of term and late preterm infants? Am J Perinatol. 2013;30(06):499–504.
- Bonadio W, Maida G. Urinary tract infection in outpatient febrile infants younger than 30 days of age: a 10-year evaluation. Pediatr Infect Dis J. 2014;33(4):342–4.
- Garcia FJ, Nager AL. Jaundice as an early diagnostic sign of urinary tract infection in infancy. Pediatrics. 2002;109(5):846–51.
- Wiswell TE, Geschke DW. Risks from circumcision during the first month of life compared with those for uncircumcised boys. Pediatrics. 1989;83(6):1011–5.
- Goldman M, Lahat E, Strauss S, Reisler G, Livne A, Gordin L, et al. Imaging after urinary tract infection in male neonates. Pediatrics. 2000;105(6):1232–5.
- Cataldi L, Zaffanello M, Gnarra M, Fanos V, Neonatal Nephrology Study Group, Italian Society of Neonatology. Urinary tract infection in the newborn and the infant: state of the art. J Matern Fetal Neonatal Med. 2010;23(sup3):90–3.
- Downs SM. Technical report: urinary tract infections in febrile infants and young children. Pediatrics. 1999;103(4).
- Herreros Fernández ML, González Merino N, Taqarro García A, Pérez Seoane B, de la Serna Martínez M, Contreras Abad MT, et al. A new technique for fast and safe collection of urine in newborns. Arch Dis Child. 2013;98(1):27–9.
- Wiswell TE, Hachey WE. Urinary tract infections and the uncircumcised state: an update. Clin Pediatr. 1993;32(3):130–4.
- Youssef DM, Elfateh HA, Sedeek R, Seleem S. Epidemiology of urinary tract infection in neonatal intensive care unit: a single center study in Egypt. J Acad Med Sci. 2012;2(1):25–9.
- Nickavar A, Khosravi N, Doaei M. Early prediction of urinary tract infection in neonates with hyperbilirubinemia. J Renal Inj Prev. 2015;4(3):92–5.
- Milani Hosseini S, Ataei N, Khalafi F, Sheikhvatan M. Incidence of urinary tract infection in neonates with septicemia: a prospective study. Minerva Pediatr. 2011;63(5):369–73.
- Littlewood JM. 66 infants with urinary tract infection in first month of life. Arch Dis Child. 1972;47(252):218–26.
- Sharif M, Madani M, Kheirkhah D. Urinary tract infection in icteric infants younger than one week. KAUMS Journal (FEYZ). 2014;18(4):383–8.
- Khalesi N, Sharaki T, Haghigh M. Prevalence of urinary tract infection in neonates with prolonged jaundice referred to Aliasghar hospital in Zahedan (2005). J Qazvin Univ Med Sci. 2007;11(3):14–8.
- Hematyar M, Emami P. Incidence of urinary tract infection in hospitalized icteric neonates in Javaheri hospital (2003-2006). J Med Counc Islam Repub Iran. 2009;27(3):343–8.
- Désinor OY, Silva JL, Ménos MJ. Neonatal sepsis and meningitis in Haiti. J Trop Pediatr. 2004;50(1):48–50.
- Hajebrahim Tehrani F, Valaie N. Incidence of septicemia and urinary tract infection in newborns with jaundice hospitalized in Mofid hospital. KAUMS Journal (FEYZ). 2004;7(4):58–63.
- Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet. 2005;365(9465):1175–88.
- Downey LC, Benjamin Jr DK, Clark RH, Watt KM, Hornik CP, Laughon MM, et al. Urinary tract infection concordance with positive blood and cerebrospinal fluid cultures in the neonatal intensive care unit. J Perinatol. 2013;33(4):302–6.
- Tamim MM, Alesseh H, Aziz H. Analysis of the efficacy of urine culture as part of sepsis evaluation in the premature infant. Pediatr Infect Dis J. 2003;22(9):805–8.
- Eliakim A, Dolfin T, Korzets Z, Wolach B, Pomeranz A. Urinary tract infection in premature infants: the role of imaging studies and prophylactic therapy. J Perinatol. 1997;17(4):305–8.
- Boskabadi H, Maamouri G, Mafinejad S, Rezagholizadeh F. Clinical course and prognosis of hemolytic jaundice in neonates in North East of Iran. Maced J Med Sci. 2011;4(4):403–7.
- Sastre JB, Aparicio AR, Cotallo GD, Colomer BF, Hernández MC, de Hospitales Castrillo G. Urinary tract infection in the newborn: clinical and radio imaging studies. Pediatr Nephrol. 2007;22(10):1735–41.
- Eghbalian F, Monsef AR. Prolonged jaundice as an early manifestation of asymptomatic urinary tract infection. J Urmia Univ Med Sci. 2009;20(2):98–103.
- Huang YS, Wang SM, Liu CC, Yang YJ. Invasive Escherichia coli infection in infancy: clinical manifestation, outcome, and antimicrobial susceptibility. J Microbiol Immunol Infect . 2002;35(2):103–8.
- Crain EF, Gershel JC. Urinary tract infections in febrile infants younger than 8 weeks of age. Pediatrics. 1990;86(3):363–7.
- Ismaili K, Lolin K, Damry N, Alexander M, Lepage P, Hall M. Febrile urinary tract infections in 0-to 3-monthold infants: a prospective follow-up study. J Pediatr. 2011;158(1):91–4.
- Rahman AJ, Naz F, Ashraf S. Significance of pyuria in the diagnosis of urinary tract infections in neonates. J Pak Med Assoc. 2011;61(1):70–3.
- Bachur R, Harper MB. Reliability of the urinalysis for predicting urinary tract infections in young febrile children. Arch Pediat Adol Med. 2001;155(1):60–5.
Copyright @ 2018 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id