
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment References
Community Research
The effect of albendazole toward anemia in children with soil-transmitted helminths infection in a remote and endemic area
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.v27i4.2857 Med J Indones. 2018;27:293–8
Received: May 22, 2018
Accepted: November 28, 2018
Author affiliation:
Department of Parasitology, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
Corresponding author:
Sri Wahdini
E-mail: sri.wahdini01@ui.ac.id
Background
Soil-transmitted helminths (STH) infections lead to nutritional disorder and anemia among children. Albendazole 400 mg is used to control STH, although it has a low cure rate for Trichuris trichiura. The effectiveness of albendazole could be increased by giving a dose of 400 mg for 3 consecutive days. The aim of the study was to investigate the effectiveness of the tripledose albendazole 400 mg course in decreasing STH and anemia prevalence.
Methods
This study used an experimental comparative design conducted in July 2016 and January 2017 in Perobatang Village, Southwest Sumba, Indonesia. Children aged 1–15 years were asked to collect fecal samples to be examined using a Kato-Katz method. Hemoglobin level (Hb) was tested using a rapid test diagnostic strip. STH positive subjects were given 400 mg of albendazole for 3 days witnessed by the researchers. Six months after, the stool samples and Hb levels were re-examined (posttest).
Results
From the 156 subjects examined (pretest), the prevalence of Ascaris lumbricoides, Trichuris trichiura, and hookworm were 65.4%, 55.8%, and 15.4%, respectively, and the prevalence of anemia was 71.2%. On post-test, the prevalence of A. lumbricoides, T. trichiura, and hookworm decreased to 8.3%, 12.8%, and 0%, respectively, and the prevalence of anemia decreased to 25%. There was a significant difference in the prevalence of STH infection and anemia before and after the administration of triple-dose albendazole (p=0.001).
Conclusion
The triple-dose albendazole is effective in reducing the prevalence of STH and anemia in children with STH infection.
Keywords
albendazole, anemia, soil-transmitted helminths, triple dose
Soil-transmitted helminths (STH) infections can lead to nutritional disorder and anemia in children. The most frequent types of STH are Ascaris lumbricoides, Trichuris trichiura, and hookworm (Necator americanus and Ancylostoma duodenale). A. lumbricoides absorbs nutrients from the host, while T. trichiura and hookworms feed on the host’s blood that could lead to anemia, especially in severe infection. Mild anemia could lead to weakness and activity disruption, whereas moderate and severe anemia could interfere with the growth and development of children and result in premature births for pregnant women and low birth weight of neonates.1,2
The World Health Organization (WHO)3 recommendation to control STH infections is a single-dose albendazole 400 mg. The drug has a broad-spectrum effect; therefore, it could control any type of STH infections. Nevertheless, the treatment of albendazole 400 mg single dose has a low cure rate for T. trichiura (34%).2 But the cure rate of albendazole could be increased by giving a dose of 400 mg for 3 consecutive days; however, its effectiveness is influenced by various factors such as infection level and food consumption. A high infection level may reduce the bioavailability of an anthelmintic, and a high number of immature stages may be less sensitive to anthelmintics.1,2 Foods that contain fat will increase the absorption of albendazole, which will affect the concentration of the drug in the blood.
Perobatang Village, Southwest Sumba District (SSD), East Nusa Tenggara, Indonesia, is a remote area with a tropical climate. It suffers from difficulties including a lack of clean water, poverty, and low and poor education. The area has clay soil and a loose ground structure that are suitable for the development of infective larvae. Because of these factors, the infection rate of STH in this area is high. People mainly work as farmers and the children play on the ground, which increase the risk of STH infection.3,4 The daily consumption of Sumba people is mainly carbohydrates, and they very rarely consume fat; low-fat consumption can affect albendazole absorption. Hence, it is necessary to investigate the effectiveness of the triple-dose albendazole 400 mg treatment regime in decreasing STH and anemia prevalence in children in Perobatang Village, SSD.
METHODS
This study used an experimental design with a comparative categorical analysis in pairs of two proportions. The intervention given was a triple-dose 400 mg albendazole. The data were collected at Perobatang Village, SSD, in July 2016 and January 2017. The subjects included were children aged 1–15 years (total sampling) who followed the whole series of the study. Exclusion criteria were severe STH infection and fever. The subjects were dropped out from the study if they had not followed the whole examination process.
Prior to data collection, the subjects and their parents were explained about the purpose and role of the participants in the study. After informed consent has been obtained, an interview to gather biodata and measurement of hemoglobin (Hb) levels using a rapid test diagnostic strip were conducted. Afterward, the subjects were instructed on how to collect the fecal samples. Thumb-sized feces were placed into a 10 ml pot (priorly labeled), which was then returned to the researcher on the next day for examination using the Kato-Katz method and then examined microscopically.
All positive subjects were given albendazole 400 mg (>2 to 15 years old) and 200 mg (1 to <2 years old) for 3 consecutive days, and the administration of the drugs was witnessed by the researchers. Six months following the pretest, a re-examination of the stool and Hb level (posttest) was performed to investigate whether there is a decrease in STH prevalence and an increase of Hb level. The treatment was effective when there was a significant decrease in the prevalence of anemia in children with STH infection (p<0.05).
The data were processed using Statistical Product and Service Solutions (SPSS) version 20. McNemar’s test was used to determine the association of prevalence between STH and anemia in STH-infected children before and after the treatment. The α-value was set at 0.05, and the confidence interval (CI) was 95%. A p-value of less than 0.05 was considered significant. This study has obtained ethical clearance from the Faculty of Medicine, Universitas Indonesia No. 876/UN2.F1/ETIK/2016.
RESULTS
Prevalence of STH before and after intervention
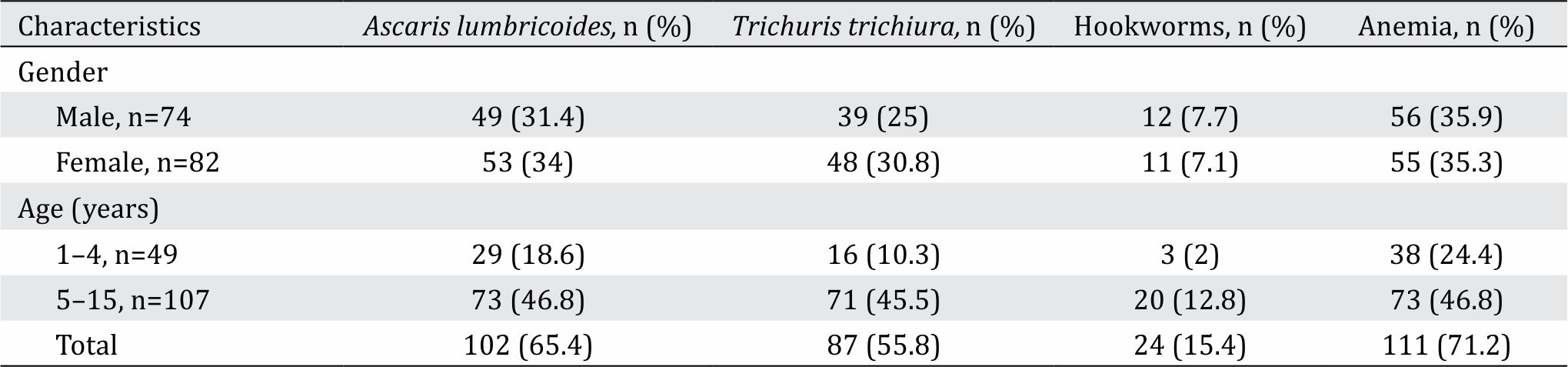
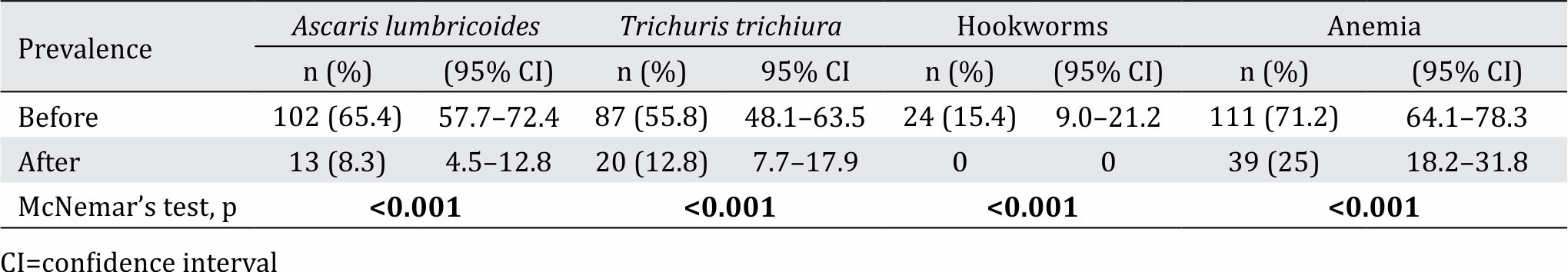
Out of the 250 children, 156 were included in this study. Before the treatment, the prevalence of STH infection was high (84%) and consisted of A. lumbricoides (65.4%), T. trichiura (55.8%), and hookworm (15.4%; Table 1). The infection intensity of the three worms was mostly moderate; however, 3% was regarded as severe infection for A. lumbricoides and T. trichiura. Six months after the treatment, the prevalence of A. lumbricoides, T. trichiura, and hookworms decreased significantly to 8.3%, 12.8%, and 0%, respectively (McNemar’s test, p<0.001; Table 2).
Table 1. The prevalence of soil-transmitted helminths (STH) and anemia based on gender and age of children at Perobatang Village, 2016
Prevalence of anemia before and after intervention
As shown in Table 2, the prevalence of anemia before the treatment was 71.2%, and it significantly decreased to 25% after the treatment (McNemar’s test, p<0.001).
Table 2. The prevalence of soil-transmitted helminths (STH) and anemia before and 6 months after the treatment of triple-dose albendazole
DISCUSSION
Perobatang Village, SSD, is one of the underdeveloped regions in Indonesia. The residents face problems such as lack of clean water sources, poverty, and low education. To obtain water, wells must be more than 50 meters deep. The government made an artesian well for each village, but this is often not enough to fulfill their needs. The residents are also unable to dig their own wells because of the depth and fund limitation. These restrict the residents’ use of water primarily for cooking and drinking and rarely for washing their hands before meals or after contact with soil. These, in addition to their main occupation as rice and corn farmers, are risk factors for STH infections.
The houses at Perobatang Village are usually built from traditional materials. The roofs are made of coconut leaves, walls of bamboos, and floor of soils. Pets such as dogs, pigs, and chickens roam freely inside the house. Houses are usually unequipped with latrines, hence, the poor hygienic practice of free defecation. The residents rarely use footwear because they cannot afford shoes and feel uncomfortable wearing them. These are the risk factors for hookworm infections. Hookworm larvae could penetrate through the exposed skin, which comes in direct contact with larvae-contaminated soil.
Children actively play in the yard and are often in contact with the soil but rarely bath and wash their hands. Their nails were long, black, and dirty, which are a possible transmission site of STH eggs especially as they often do not wash their hands. STH infections in boys and girls were similar because of a comparable outdoor activity and soil contact as well as hygiene and sanitation practices. Based on age groups, children aged 5–15 years had a higher STH infection rate compared with children aged 1–4 years. This is because school-aged children have more outdoor activities and hence are more in contact with soil compared with preschoolers.
STH infection status before and after the intervention
After the administration of triple-dose albendazole, STH infection was decreased significantly. Randomized controlled studies conducted by Edegnika et al5 compared the single dose and repeated doses of albendazole in the treatment of A. lumbricoides, T. trichiura, and hookworm. Single-dose albendazole effectively treated A. lumbricoides with cure and egg reduction rates of 85% and 93%, respectively. Double-dose albendazole effectively treated hookworm with cure and egg reduction rates of 92% and 92%, respectively. Triple-dose albendazole is ineffective in treating T. trichiura but provides an egg reduction rate of 90.6%.
Speich et al6 studied the efficacy and reinfection of STH 18 weeks after the treatment. Albendazole–oxantel pamoate showed good efficacy against T. trichiura (cure rates of 54% and egg reduction rate of 98.6%) than other anthelminthics. STH reinfection occurred 18 weeks after the treatment, i.e. 37.2% against T. trichiura, 34.6% to A. lumbricoides, and 25% to hookworm. Tun et al7 conducted a study in Myanmar and found that 400 mg of albendazole every 6 months for 7 years succeeded in controlling STH without changing the subject environment and behavioral practices.
The WHO recommends periodic drug treatment (deworming) to all children living in endemic areas once a year when the prevalence of STH infections in the community is over 20% and twice a year when over 50%. In this study, the prevalence of STH was more than 50%; hence, another mass drug administration must be carried out every 6 months using triple-dose albendazole. The results of this study endorse the local government to conduct mass treatment every 6 months for at least 5 consecutive years to control STH and provide clean water and latrines for residents in order to stop open defecation practices.
Anemia status before and after intervention
Anemia due to chronic infection could be eliminated by treating the infection. Hence, anemia caused by an STH infection could be treated by eliminating the STH that infects the patients.8,9 Hookworm is one of the common types of STH that most often cause anemia because it uses a hook to attach itself to the proximal duodenum of the intestinal mucosa, including the distal part of the jejunum and proximal ileum. The attachment causes rupture of the arterioles and venules in the luminal surface of the small intestine resulting in bleeding. Hookworm secretes a hyaluronidase enzyme that degrades intestinal mucosa and erodes blood vessels, resulting in blood loss. Hookworm can cause anemia because of the intestinal mucosal bleeding.10,11
Anemia could also be caused by a T. trichiura infection especially in severe cases. Immature worms will migrate to the large intestine and penetrate the epithelial and intracellular cells. They continue to expand creating tunnels in the epithelium. The posterior part of the worm destroys the cell membrane, and the worm partially protrudes into the lumen of the colon, whereas the anterior portion is still attached to the epithelium. This causes the destruction of the normal bowel architecture; thus, the more severe the infection is, the more parasites are attached to the intestinal surface thereby causing more blood loss.12
Severe ascariasis could also cause anemia, but not as severe as a hookworm infection. A. lumbricoides absorb the proteins and components needed to form erythrocytes, and Hb synthesis is disrupted. In ascariasis, anemia is due to iron deficiency from vitamins B6 and B12, folic acid, and other nutrients.13
Smith et al14 conducted a research on indigenous communities in Manu forest, Peru. Researchers found that a double-dose albendazole yields a decrease in STH and increase of Hb to 1.89 g/l, while a double-dose mebendazole did not increase the Hb level. A combination therapy of albendazole–praziquantel showed an increase in Hb at 2.37 g/l (95% CI: 0.13–0.34), but the administration of albendazole with iron supplementation did not provide an additional benefit to anemia. A cohort study by Casey et al15 showed that triple-dose albendazole with iron supplementation and folic acid every week for 54 weeks decreased anemia from 38% to 18%. The therapy also reduced hookworm infection from 76% to 11%.
In this study, prior to the administration of triple-dose albendazole, 71.2% of the subjects had anemia. Six months after the treatment, the subjects affected by anemia decreased to 25%. Anemia is more common in women than in men because women have menstruation. In this study, anemia in boys did not differ significantly with that of in girls because only a few girls have experienced menstruation.
Furthermore, another factor that causes anemia is poor nutritional intake. Various substances, including metals (iron, cobalt, and manganese), vitamins (B12, B6, C, E, folate, riboflavin, pantothenic acid, and thiamine), and amino acids are needed to form erythrocytes. The function of erythrocytes is to circulate oxygen bound by Hb to all body tissues and carry CO2 to the lungs and out from the body.8,9 In performing this function, Hb is an important factor in carrying erythrocytes.8 Hb is a protein consisting of Hb A (Hb dominant in the blood after 3–6 months of age), which is composed of four α2β2 polypeptide chains with its respective heme groups; adult patient’s blood also contains small amounts of fetal hemoglobin (HbF) and adult hemoglobin (HbA).9 Heme synthesis occurs in the mitochondria through a series of biochemical reactions and involves the condensation of glycine and succinyl-coenzyme A regulated by the enzyme δ-aminolaevulinic acid (ALA) synthase. Vitamin B6 is a coenzyme used in the formation of Hb; thus, food intake needs to be varied to obtain the necessary minerals and Hb-forming vitamins.9
People at the village rarely consume nutritious food that contains iron, folic acid, and vitamin B12. Many of the villagers work as farmers and fishermen; thus, fish is the main source of protein. However, almost all of the fish caught are sold, leaving only a small portion to be consumed by the family. The villagers of Perobatang often keep swine, but they are still often for sale. Other sources of protein are chicken and eggs. In addition to raising animals, people need to be taught how to grow crops for consumption.
STH treatment should be done every 6 months. Health education primarily concerning the nutrition aspect and hygiene practice must be conducted. This way, the residents could prioritize the fulfillment of nutritional needs of each family and improve their hygiene practice.
In conclusion, the administration of triple-dose albendazole effectively decreased the prevalence of STH and anemia in STH-infected children. The prevalence of A. lumbricoides, T. trichiura, and hookworms at baseline were 65.4%, 55.8%, and 15.4%, respectively, and decreased to 8.3%, 12.8%, and 0%, respectively. The prevalence of anemia in children with STH infection was 71.2% and decreased to 25% after the treatment.
Conflicts of Interest
Saleha Sungkar is one of the editorial board members, but was not involved in the review or decision process of this article.
Acknowledgment
This study was supported by grants from the Directorate of Research and Public Services Universitas Indonesia (Direktorat Riset dan Pengabdian kepada Masyarakat Universitas Indonesia) 2017. The authors would like to thank the Perobatang Village chief for his continuous support during our study.
REFERENCES
- WHO. Intestinal worm. Geneva: WHO; 2016. Accessed 20 June 2016. Available from: http://www.who.int/ intestinal_worms/epidemiology/en/
- Steinmann P, Utzinger J, Du Z, Jiang J, Chen J, Hattendorf J, et al. Efficacy of single-dose and triple dose albendazole and mebendazole against STH and Taenia sp: a randomized controlled trial. PLoS ONE. 2011;6(9): e25003.
- WHO [Internet]. Preventive chemotherapy in human helminthiasis. Geneva: WHO; 2006 [cited Jun 2016]. Available from: http://apps.who.int/iris/ bitstream/10665/43545/1/ 9241547103_eng.pdf
- Indonesian Central Bureau of Statistics [Internet]. Income per capita by city 2013-2014 [cited 20 June 2016]. Jakarta: Indonesian Central Bureau of Statistics; 2013. Available from: http://ntt.bps.go.id/ linkTableDinamis/view/id/44
- Edegnika AA, Zinsou JF, Issifou S, Ateba-Ngoa U, Kassa RF, Feugap EN, et al. Randomized controlled assessorblind clinical trial to assess the efficacy of single-versus repeated-dose albendazole to treat A. lumbricoides, T. trichiura, and hookworm infection. Antimicrob Agents Chemother. 2014;58(6):2535–40.
- Speich B, Moser W, Ali SM, Ame SM, Albonico M, Hattendorf J, et al. Efficacy and reinfection with soiltransmitted helminths 18-weeks post-treatment with albendazole-ivermectin, albendazole-mebendazole, albendazole-oxantel pamoate and mebendazole. Parasit Vectors. 2016;9:123.
- Tun A, Myat SM, Gabrielli AF, Montresor A. Control of soil-transmitted helminthiasis in Myanmar: results of 7 years of deworming. Trop Med Int Health. 2013;18(8):1017–20.
- Maakaron JE [Internet]. Anemia: practice essentials, pathophysiology, etiology [cited: Nov 2017] Available from: http://emedicine.medscape.com/article/198475
- Hoffbrand AV, Moss PAH. Erithropoiesis and general aspects of anemia. In: Hoffbrand AV, Moss PAH, editors. Hoffbrand’s essential haemology. 7th Ed. London: Wiley; 2016.
- Centers for Disease Control and Prevention [Internet]. Parasites-hookworm. Atlanta: CDC; 2013 [cited June 2016]. Available from: http://www.cdc.gov/parasites/ hookworm/
- Haburchak D. Hookworm. Medscape [Internet]. Updated: Feb 24, 2016 [cited June 2016]. Available from:http://emedicine.medscape.com/article/218805
- Centers for Disease Control and Prevention [Internet]. Trichuriasis. Atlanta: CDC; 2016. [cited June 2016]. Available from: http://www.cdc.gov/parasites/ whipworm/
- Centers for Disease Control and Prevention [Internet]. Ascariasis. Atlanta: CDC; 2013. [cited June 2016]. Available from: http://www.cdc.gov/parasites/ ascariasis/
- Smith JL, Brooker S. Impact of hookworm infection and deworming on anemia in non-pregnant population: a systemic review. Trop Med Int Health. 2010;15(7):776–95.
- Casey GJ, Montresor A, Cavalli-Sforza LT, Thu H, Phu LB, Tinh TT, et al. Elimination of iron deficiency anemia and STH infection: evidence from a 44 month ironfolic acid and deworming program. PLoS Negl Trop Dis. 2013;7(4):e2146.
Copyright @ 2018 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited.
mji.ui.ac.id