
Section Abstract Introduction Methods Results Discussion Conflict of Interest Acknowledgment Funding Sources References
Basic Medical Research
Zika, chikungunya, and dengue viral infections in human peripheral blood mononuclear cells: cell susceptibility and gene expression
pISSN: 0853-1773 • eISSN: 2252-8083
https://doi.org/10.13181/mji.oa.193548 Med J Indones. 2020;29:129–35
Received: January 30, 2019
Accepted: April 03, 2019
Authors' affiliation:
¹Department of Chemistry, Faculty of Mathematics and Natural Sciences, Universitas Indonesia, Depok, Indonesia,
²Eijkman Institute for Molecular Biology, Ministry of Research and Technology/National Agency for Research and Innovation, Jakarta, Indonesia
Corresponding author:
R. Tedjo Sasmono
Dengue Research Unit, Eijkman Institute for Molecular Biology,
Jalan Diponegoro 69, Central Jakarta 10430, Indonesia
Telp/Fax: +62-21-3917131
E-mail: sasmono@eijkman.go.id
Background
Infections of Zika (ZIKV), dengue (DENV), and chikungunya viruses (CHIKV) are presented with similar clinical symptoms; these often lead to misdiagnosis. Viremia levels and host immune responses may contribute to disease severity. This study was aimed to characterize the ability of ZIKV, CHIKV, and DENV to infect human peripheral blood mononuclear cells (PBMCs) and assess the expression of tumor necrosis factor (TNF)-α, interleukin (IL)-10, and interferon gamma-induced protein (IP)-10 genes in response to the viral infections.
Methods
PBMCs were isolated from healthy donors using gradient centrifugation. Cells were infected with Indonesian isolates of ZIKV, CHIKV, and DENV for 48 hours. Plaque assays were performed to measure viable virus titers, while viral genomic RNA and the gene expression of TNF-α, IL-10, and IP-10 were determined using real-time quantitative reverse transcription-polymerase chain reaction.
Results
The susceptibility of PBMCs to ZIKV, CHIKV, and DENV infection was observed, and the viable virus titer and viral genome quantity were found to be significantly higher in ZIKV and CHIKV. All viruses induced the expression of immune-related proteins. The TNF-α gene was upregulated by all viruses to relatively similar levels. IL-10 expression was highest in response to ZIKV, followed by CHIKV. In contrast, IP-10 expression was highly upregulated in DENV-infected cells and only moderately expressed in ZIKV- and CHIKV-infected cells.
Conclusions
ZIKV, CHIKV, and DENV clinical isolates infected PBMCs with different levels of virus infectivity. The gene expression of IL-10 was highly upregulated in ZIKV infection and IP-10 in DENV infection.
Keywords
chemokines, chikungunya virus, cytokines, dengue virus, mononuclear leukocytes, Zika virus
Indonesia is among the most vulnerable regions in Asia that suffering from arthropod-borne virus (arbovirus) outbreaks due to its climate and environment suitable for Aedes mosquitoes, which are the principal vector of the virus.¹ Zika (ZIKV), dengue (DENV), and chikungunya viruses (CHIKV) are three arboviruses which are considered major public health concerns because of their expanding geographical range and the high number of cases that may lead to severe clinical and epidemiological implications.² ZIKV, DENV, and CHIKV infections share similar clinical symptoms. Since DENV and CHIKV infections are more common in Asia and Africa, sometimes only a small number of clinicians are aware of ZIKV infections in humans. Moreover, only a few laboratories have ZIKV clinical testing capabilities.³ This situation may lead to clinical misdiagnosis in the areas where these viruses are present. Hence, enhancing our knowledge on the phenotypic differences between these viruses and identifying how they infect cells and induce host immune responses are useful to better understand the pathomechanisms of arboviruses infections.
During the recent outbreak in Bali and Jambi, DENV, CHIKV, and ZIKV were isolated from patients with mild clinical manifestations.⁴⁻⁶ During the 2015 dengue outbreak in Bali, notable clinical symptoms of malaise, nausea, loss of appetite, headache, and myalgia were observed in the majority of patients.⁶ Both ZIKV and CHIKV, which were identified in Jambi during the dengue outbreak in early 2015, showed similar symptoms to DENV acute infection, such as fever and headache. However, ZIKV-infected patients had no rash, conjunctivitis, or peripheral edema, and CHIKV-infected patients did not show rash, arthralgia, or fever, which are hallmarks of the respective viruses.4,5 The analysis of distinct clinical symptoms in the acute phase of arbovirus-infected patients in Indonesia compared with the previous study on ZIKV, DENV, and CHIKV might provide useful information to help uncover the peculiar pathomechanisms and immune responses of the Indonesian population against the arboviruses.
This study was aimed to investigate the characteristics of Indonesian ZIKV, DENV, and CHIKV infections using an in vitro infection model. The susceptibility of healthy human peripheral blood mononuclear cells (PBMCs) and the induced immune responses were analyzed by focusing on cytokine/chemokine gene expression. The susceptibility of PBMCs, which have been previously used in the study of arbovirus infections,7,8 was assessed by measuring virus replication using a plaque assay method and viral RNA genome detection. Also, the gene expression profiles of three immune-related proteins, including tumor necrosis factor (TNF)-α, interleukin (IL)-10, and interferon gamma-induced protein (IP)-10, were analyzed using relative quantification.
METHODS
Human PBMCs were collected from the whole blood of healthy donors. The involvement of human subjects in this study was approved by the Eijkman Institute Research Ethics Commission number 125/2018. All donors provided a written informed consent before their enrollment in this study. All donors were healthy after meeting the criteria as follows: body temperature of 36.5–37.5°C, pulse rate of 60–100 times/min, respiration rate 12–20 times/min, blood pressure of 90/60–120/80 mmHg (systolic/diastolic), with no hematological/anemia status, and not taking medication for any sickness. Based on Dengue NS1 and IgM/IgG detection, all donors were negative for dengue infection. The ZIKV strain JMB-185 (Asian genotype), CHIKV strain JMB-192 (Asian genotype), and DENV-2 strain SJN-006 (Cosmopolitan genotype) were isolated from patients with mild clinical manifestations from Indonesia.⁴⁻⁶ Viruses were propagated in Vero cells (Cercopithecus aethiops, monkey kidney, ATCC® CCL-81™) to provide viral stocks for this study.
Approximately 20 ml of venous blood was collected from three donors using an aseptic venipuncture technique, and this was later stored in heparin tubes (Vacuette®, Greiner Bio-One, Austria). The blood was diluted with Dulbecco’s phosphate-buffered saline (D-PBS) (Gibco, Thermo Fisher Scientific, USA) at a ratio of 1:2. The diluted blood was carefully added into 15 ml centrifuge tubes containing Ficoll-Paque PLUS (GE Healthcare, USA) solution to generate layers of blood on the top of Ficoll at a ratio of 6:4. Tubes were centrifuged for 40 min at 400 × g in a centrifuge chamber set to 20°C. The buffy coat ring containing PBMCs was collected, pooled, washed with D-PBS (three times the volume of the PBMC suspension), centrifuged for 10 min at 100 × g at 20°C, and resuspended in 1X Roswell Park Memorial Institute (RPMI) 1640 (Gibco) complete cell culture medium supplemented with 10% fetal bovine serum and 1% antibiotic/antimycotic solution (Gibco). The number of isolated PBMCs was measured using a hemocytometer (Neubauer Improved, Superior Marienfeld, Germany) and seeded in wells of 24-well plates (Corning, USA).
A total of 1 × 10⁶ PBMCs/well was cultured in 1 ml of RPMI complete medium in 24-well plates, and before infection, cells were incubated overnight at 37°C with 5% CO₂ for cell adaptation and resting. Cells were then infected with ZIKV, CHIKV, and DENV at a multiplicity of infection of one plaque-forming unit (PFU)/cell, such that one virus particle theoretically infected each cell. The positive/reactive and negative/uninfected controls were prepared by adding 1 μg/ml of lipopolysaccharide and RPMI complete medium only, respectively. PBMC infections were performed in duplicate for each group. The plates were incubated for 48 hours at 37°C with 5% CO₂ before the cells and supernatants were harvested.
The plaque assay was performed to quantify the titer of the viable virus from PBMC infection experiments. Briefly, BHK-21 cells (Mesocricetus auratus, hamster kidney, ATCC® CCL-81™) in RPMI complete medium were seeded in 24-well plates at a density of 2 × 105 cells/well and incubated in a 37°C incubator with 5% CO2 for a 2-day incubation period. Cell monolayers was infected with 200 μl of the ten-fold serially diluted supernatant from the PBMC infection assay in duplicate and incubated for 60 min at 37°C with 5% CO2 to allow virus adsorption. Inoculated wells were then aspirated and replenished by adding 0.5 ml of 1% carboxymethyl cellulose overlay. Plates were incubated for four (CHIKV) or five (ZIKV and DENV) days at 37°C with 5% CO2 to ensure similar plaque sizes. Cells were then fixed with 3.7% formaldehyde solution for 30 min and visualized by staining using 1% w/v crystal violet (Sigma, USA) in distilled water. Plaques were counted manually and expressed as PFU/ml.
Viral RNA from the supernatant was extracted using PureLink Viral RNA/DNA Mini Kit (Invitrogen, Thermo Fisher Scientific, USA) as per the manufacturers’ procedures. Total RNA was extracted from cells using the RNeasy RNA extraction kit (Qiagen, Germany) as per the manufacturers’ protocol. Extracted RNA from both cell lysates and supernatants underwent quantification of the viral genome using a SuperScriptTM III PlatinumTM Green One-Step qRT-PCR Kit (Invitrogen), 7500 Fast Real-Time PCR System (Applied Biosystems, USA), and target-specific primer sets as listed in Table 1. The relative quantity of viral RNA was measured based on the cycle threshold (Ct) value. The process was performed in duplicates.
Table 1. Primers used in the study
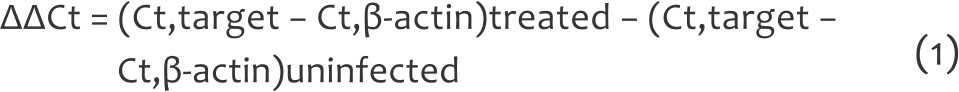
The extracted RNA templates were normalized to 50 ng/reaction, and they were used for cDNA preparation using a SuperScriptTM III Reverse Transcriptase System (Invitrogen) and oligo(dT) primer (Promega, USA) in a SimpliAmpTM Thermal Cycler (Applied Biosystems) at 42°C for 1 hour. The synthesized cDNA was stored at -20°C until use. Cytokine and housekeeping gene expression levels were determined by quantitative polymerase chain reaction (qPCR) using GoTaq® qPCR Master Mix (Promega) in a 7500 Fast Real-Time PCR System. The relative quantification analysis was performed to measure the expression of TNF-α, IL-10, and IP-10 genes normalized to human β-actin housekeeping gene and relative to the uninfected control using primers listed in Table 1. Relative gene expression was calculated based on Ct values using the 2-ΔΔCt method (Equation-1), where
SPSS version 25 (IBM Corp., USA) was used for all statistical analyses. The differences in viable virus quantification, viral RNA detection, and cytokine/chemokine gene expression were evaluated by oneway analysis of variance for mean comparisons of multiple groups with the Tukey–Kramer post-hoc test. A p-value of <0.05 was considered statistically significant. The results were presented as the mean (standard deviation [SD]).
RESULTS
The number of viable ZIKV, DENV, and CHIKV was measured as the number of viable viruses propagated and secreted into the supernatant by infected PBMCs 48 hours after infection. As shown in Figure 1, the number of viable ZIKV, DENV, and CHIKV were 4.92 × 10⁴ (1.23 × 10⁴), 8.04 × 10² (2.75 × 10²), and 5.00 × 10⁴ (1.08 × 10⁴), respectively. Compared with DENV, the measured viable ZIKV and CHIKV were significantly higher (p<0.01).
Figure 1.
Viable virus counts (PFU/ml) following infection of
PBMCs for 48 hours determined by plaque assay method.
Data were obtained from three unrelated individual donors,
and experiments were performed in duplicate. PFU=plaque-forming
unit; ZIKV=Zika virus; DENV=dengue virus;
CHIKV=chikungunya virus
*Tukey–Kramer test, p<0.01
To assess the ability of the viruses to infect and replicate within PBMCs, we quantified viral genomes using real-time quantitative reverse transcription-polymerase chain reaction (qRT-PCR). The intracellular virus genomes were quantified using RNA extracted from PBMC lysates. The relative RNA quantity of ZIKV was significantly higher compared with that of DENV and CHIKV (p<0.01) with Ct values of 15.84 (1.76), 23.16 (1.85), and 23.75 (1.49), respectively (Figure 2a). In addition, DENV and CHIKV have shown a similar amount of viral RNA (Figure 2a). The relative quantity of the viral genomes in the culture supernatant was also measured using the same method. Similarly, the RNA quantity of ZIKV was also higher compared with that of CHIKV and DENV (p<0.01) with Ct values of 13.75 (1.03), 24.51 (1.19), and 19.65 (0.97), respectively (Figure 2b).
Figure 2.
Viral RNA detection in PBMC lysates (a) and culture supernatants (b) determined by qRT-PCR. Higher Ct value represents
lower viral load. PBMC=peripheral blood mononuclear cell; qRT-PCR=quantitative reverse transcription-polymerase chain reaction;
Ct=cycle threshold; ZIKV=Zika virus; DENV=dengue virus; CHIKV=chikungunya virus
*Tukey–Kramer test, p<0.01
The ability of ZIKV, CHIKV, and DENV to infect PBMCs was used as the basis to investigate the response of PBMCs against viral infections by assessing the expression of immune mediators. The gene expressions of TNF-α, IL-10, and IP-10 were measured using real-time qRT-PCR. Figure 3 shows the gene expression of these factors in ZIKV-, DENV-, and CHIKV-infected PBMCs. The expression of TNF-α was upregulated by 2.37 (2.01)-, 2.69 (1.46)-, and 3.65 (2.46)-fold, measured as mean fold change (SD), in PBMCs infected with ZIKV, DENV, and CHIKV, respectively, relative to the uninfected controls. However, no significant change in the expression of TNF-α gene was observed following infection by these viruses (p>0.05). In ZIKV- and CHIKV-infected PBMCs, the expression of IL-10 was upregulated by 3.53 (1.59)- and 1.56 (1.09)-fold, respectively (Figure 3). Interestingly, IL-10 gene expression was significantly downregulated by 0.52 (0.29)-fold in DENV-infected PBMCs. The expression of the chemokine IP-10 varied among arbovirus-infected PBMCs. Specifically, IP-10 gene expression was highly upregulated in DENV-infected PBMCs by 107.80 (54.88)-fold, followed by ZIKV- (32.83 [20.51]-fold) and CHIKV-infected PBMCs (6.91 [2.37]-fold). Overall, the infection of three arboviruses in PBMCs induced the expression of TNF-α, IL-10, and IP-10 to different degrees.
Figure 3. Gene expression of TNF-α, IL-10, and IP-10 in PBMCs in response to ZIKV, CHIKV, and DENV infections determined by qRT-PCR. Data were shown as the mean (SD) from three individual donors in three independent experiments performed in duplicate. Statistical analysis using Tukey–Kramer test: *p<0.05; †p<0.01. PBMCs=peripheral blood mononuclear cells; ZIKV=Zika virus; DENV=dengue virus; CHIKV=chikungunya virus; LPS=lipopolysaccharide; qRT-PCR=quantitative reverse transcription-polymerase chain reaction; SD=standard deviation
DISCUSSION
Studying arboviruses found to be endemic in a country, as well as examining their genetic characteristics, may contribute to better understanding of disease dynamics. PBMCs were used as a model of arbovirus infections as this cell population, particularly monocytes and dendritic cells, is susceptible to ZIKV, DENV, and CHIKV infections.⁸⁻¹⁰ This study showed that ZIKV has an increased viral load compared with DENV in the amount of viable virus and relative viral quantity, both intra- and extra-cellular. These results indicated that ZIKV replicates more robustly in PBMCs than DENV during the 48 hours post-infection. Studies of ZIKV and DENV infections in humans have also shown that PBMCs, especially monocytes, are highly susceptible to ZIKV compared with DENV.¹¹ Similar to ZIKV, CHIKV exhibits a significantly higher viral titer compared with DENV, although they have a comparable viral load in terms of relative extracellular viral quantity. This result was consistent with a previous study that compared the growth kinetics of DENV and CHIKV.¹²
PBMCs were found to be more susceptible to ZIKV and CHIKV than DENV in the acute infection phase even though all arbovirus specimens that were used in this study exhibit similar mild clinical manifestations.4–6 Hence, the difference in viral load after incubation with PBMCs may indicate their efficiency in viral attachment and replication rates against immune cells. However, the detailed mechanisms contributing to the distinct viral kinetics cannot be elucidated without considering the response of the host immune cells.
PBMCs have been widely used in infectious disease research as they display a vigorous cytokine/chemokine responses upon viral infection.7,8,13 Studies have reported that the concentrations of several cytokines/chemokines are elevated during the acute phase of infection by ZIKV.¹⁴ The variable profiles in cytokine/chemokine gene expression were also observed for DENV¹⁵ and CHIKV¹³ acute infections. This study simulated the arbovirus acute infection in which the incubation time for arbovirus-infected PBMCs lasted for 48 hours post-infection. Here, the relative gene expressions of cytokines/chemokines TNF-α, IL-10, and IP-10 were used as representatives of inflammatory cytokines, anti-inflammatory cytokines, and inflammatory chemokines, respectively.
In this study, the upregulation of TNF-α cytokine gene expression was found to be similar following the infection of all three arboviruses. This result was similar to another study that showed ZIKV-infected PBMCs exhibited similar gene expression of TNF-α compared with DENV in HTR8 cells.⁸ The transient expression of TNF-α was also observed in PBMCs infected with ZIKV at 48 hours.⁹ Similarly, elevated TNF-α levels have also been observed in the sera of dengue hemorrhagic fever/dengue shock syndrome patients in the acute phase in Malaysia.¹⁶ Furthermore, TNF-α levels were marginally higher in patients in the acute phase of CHIKV infections compared with healthy controls.¹⁰ Overall, the obtained data suggest a similar inflammatory responses in PBMCs against arbovirus infections.
Unlike TNF-α, different IL-10 gene expression profiles were observed during the arbovirus infection experiments in PBMCs. The anti-inflammatory mediator IL-10 was highly upregulated in ZIKV-infected cells but was downregulated in DENV-infected and moderately upregulated in CHIKV-infected cells. The upregulated expression of IL-10 in ZIKV-infected PBMCs supports previous study that observed the significant upregulation of IL-10 in an acute patient with a mild disease outcome.¹⁷ Regarding IL-10 downregulation in DENV-infected PBMCs, low expression of IL-10 has been found in dengue patients without warning signs but remained high in a patient with warning signs throughout the disease.¹⁸ Whether the low expression of IL-10 observed in this study is related to the nature of the DENV-2 strain used in this experiment, which only caused mild clinical manifestations,⁶ requires further examination. Meanwhile, the IL-10 expression level in CHIKV-infected PBMCs was found to be higher compared to uninfected cells. A similar result was observed in a previous study that analyzed IL-10 levels in a patient suffering from acute CHIKV infection.¹⁰ The acute phase of CHIKV infection can be described in three stages, depending on the presence of IL-10 expression. Specifically, IL-10 is highly expressed during the viral stage (positive for CHIKV), gradually declines in the antibody initiation stage (IgM positive, IgG negative), and reaches the lowest level during the seroconversion stage (IgM positive, IgG positive).¹³
IP-10 is a ligand of the chemokine receptor CXCR3 and a chemoattractant of macrophages, monocytes, natural killer cells, T cells, and dendritic cells; it also promotes the adhesion of T cells to the endothelium. The elevated levels of IP-10, along with MIG, are found to be correlated with the Th1-type reaction.¹⁹ Various degrees of IP-10 gene upregulation have been observed in arbovirus-infected PBMCs.¹⁴ In this study, IP-10 was highly upregulated in DENV-infected PBMCs. This result was in agreement with a previous study that measured IP-10 protein levels in the blood of a patient with acute DENV infection.¹⁶ Together with the downregulation of IL-10, highly expressed IP-10 was observed in a DENV-infected patient with warning signs during the acute infection phase. Even so, the patient from which DENV was isolated only showed mild clinical manifestation similar to the patients in Malaysia.¹⁶ IP-10 was upregulated in CHIKV-infected PBMCs but lower than in DENV-infected cells. A similar profile was also reported in a study that measured the levels of IP-10 in the sera of CHIKV-infected patients.¹³ Interestingly, IP-10 is widely expressed in rheumatoid arthritis (RA) and other arthritis-related disease patients.²⁰ The use of IP-10 as a biomarker for RA symptoms may imply an analogous mechanism for joint deterioration in CHIK disease.²¹ In ZIKV-infected PBMCs, we observed a relatively lower induction compared to DENV and CHIKV. This observation is consistent with the low expression of IP-10 in ZIKV acute patients who were not from an endemic area, in which the level increased during patient recovery.¹⁴ However, the findings from this study are in contrast with a report from patients in an endemic area, where IP-10 was found to be highly upregulated.²² The enhanced upregulation of IP-10 in ZIKV patients was associated with exanthema, which was previously observed from patients in an endemic area²² but not in this study.
An early inflammatory response may occur when the arbovirus is actively replicating, but then it decreases due to a counter anti-inflammatory response when the virus has been eliminated from the system. In this study, the upregulation of inflammatory markers IL-10 and IP-10 in both ZIKV and CHIKV infections was observed. However, the same did not occur in DENV-infected PBMCs, wherein IL-10 expression was found to be low and IP-10 was high. This condition may reflect the acute phase of the infection as it has been previously reported that the level of IL-10 only peaked during the late stage of the disease, whereas IP-10 remained continuously high during disease progression.²³
Limitations to this study include the examination of an incomplete set of cytokines/chemokines and the limited number of donors. Therefore, further investigations are needed to obtain the complete profiles of cytokine/chemokine responses. However, this study is the first to directly compare the cytokine/chemokine gene expression profiles in PBMCs in response to infection by Indonesian strains of ZIKV, DENV, and CHIKV.
In conclusion, this study shows that ZIKV was the most infective due to its high viral load and relative intra- and extra-cellular viral quantity compared with the other two viruses, DENV and CHIKV. Cytokine/chemokine gene expression levels were differently induced upon virus infection. Specifically, IL-10 and IP-10 were found to be highly upregulated in ZIKV and DENV infections, respectively. DENV-infected PBMCs exhibited the most rigorous inflammatory response compared to ZIKV and CHIKV, which possibly explains the low level of DENV viral load 48 hours post-infection. The differences in the induced immune responses may be used as a basis to propose biomarkers for diagnostic tests that will help in differentiating between ZIKV, DENV, and CHIKV infections.
Conflict of Interest
The authors affirm no conflict of interest in this study.
Acknowledgment
The authors thank the donors who volunteered in this study and the Eijkman Institute’s clinicians and nurses for their help in sample collection.
Funding Sources
This study was funded by the Ministry of Research and Technology through DIPA-APBN grant to Dengue Research Unit of the Eijkman Institute.
REFERENCES
- Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, et al. Global trends in emerging infectious diseases. Nature. 2008;451(7181):990–3.
- Paixão ES, Teixeira MG, Rodrigues LC. Zika, chikungunya and dengue: the causes and threats of new and re-emerging arboviral diseases. BMJ Glob Health. 2018;3(Suppl 1):e000530.
- Haddow AD, Schuh AJ, Yasuda CY, Kasper MR, Heang V, Huy R, et al. Genetic characterization of Zika virus strains: geographic expansion of the Asian lineage. PLoS Negl Trop Dis. 2012;6(2):e1477.
- Perkasa A, Yudhaputri F, Haryanto S, Hayati RF, Ma’roef CN, Antonjaya U, et al. Isolation of Zika virus from febrile patient, Indonesia. Emerging Infect Dis. 2016;22(5):924–5.
- Sasmono RT, Perkasa A, Yohan B, Haryanto S, Yudhaputri FA, Hayati RF, et al. Chikungunya detection during dengue outbreak in Sumatra, Indonesia: clinical manifestations and virological profile. Am J Trop Med Hyg. 2017;97(5):1393–8.
- Megawati D, Masyeni S, Yohan B, Lestarini A, Hayati RF, Meutiawati F, et al. Dengue in Bali: clinical characteristics and genetic diversity of circulating dengue viruses. PLoS Negl Trop Dis. 2017;11(5):e0005483.
- Banerjee A, Shukla S, Pandey AD, Goswami S, Bandyopadhyay B, Ramachandran V, et al. RNA-Seq analysis of peripheral blood mononuclear cells reveals unique transcriptional signatures associated with disease progression in dengue patients. Transl Res. 2017;186:62–78.e9.
- Luo H, Winkelmann ER, Fernandez-Salas I, Li L, Mayer SV, Danis-Lozano R, et al. Zika, dengue and yellow fever viruses induce differential anti-viral immune responses in human monocytic and first trimester trophoblast cells. Antiviral Res. 2018;151:55–62.
- Colavita F, Bordoni V, Caglioti C, Biava M, Castilletti C, Bordi L, et al. ZIKV infection induces an inflammatory response but fails to activate types I, II, and III IFN response in human PBMC. Mediators Inflamm. 2018;2018:2450540.
- Chaaitanya IK, Muruganandam N, Sundaram SG, Kawalekar O, Sugunan AP, Manimunda SP, et al. Role of proinflammatory cytokines and chemokines in chronic arthropathy in CHIKV infection. Viral Immunol. 2011;24(4):265–71.
- Michlmayr D, Andrade P, Gonzalez K, Balmaseda A, Harris E. CD14+CD16+ monocytes are the main target of Zika virus infection in peripheral blood mononuclear cells in a paediatric study in Nicaragua. Nat Microbiol. 2017;2(11):1462–70.
- Ruiz Silva M, Aguilar Briseño JA, Upasani V, van der Ende-Metselaar H, Smit JM, Rodenhuis-Zybert IA. Suppression of chikungunya virus replication and differential innate responses of human peripheral blood mononuclear cells during co-infection with dengue virus. PLoS Negl Trop Dis. 2017;11(6):e0005712.
- Kelvin AA, Banner D, Silvi G, Moro ML, Spataro N, Gaibani P, et al. Inflammatory cytokine expression is associated with chikungunya virus resolution and symptom severity. PLoS Negl Trop Dis. 2011;5(8):e1279.
- Tappe D, Pérez-Girón JV, Zammarchi L, Rissland J, Ferreira DF, Jaenisch T, et al. Cytokine kinetics of Zika virus-infected patients from acute to reconvalescent phase. Med Microbiol Immunol. 2016;205(3):269–73.
- Rathakrishnan A, Wang SM, Hu Y, Khan AM, Ponnampalavanar S, Lum LC, et al. Cytokine expression profile of dengue patients at different phases of illness. PLoS One. 2012;7(12):e52215.
- Rathakrishnan A, Klekamp B, Wang SM, Komarasamy TV, Natkunam SK, Sathar J, et al. Clinical and immunological markers of dengue progression in a study cohort from a hyperendemic area in Malaysia. PLoS One. 2014;9(3):e92021.
- Kam YW, Leite JA, Lum FM, Tan JJL, Lee B, Judice CC, et al. Specific biomarkers associated with neurological complications and congenital central nervous system abnormalities from Zika virus-infected patients in Brazil. J Infect Dis. 2017;216(2):172–81.
- Green S, Vaughn DW, Kalayanarooj S, Nimmannitya S, Suntayakorn S, Nisalak A, et al. Elevated plasma interleukin-10 levels in acute dengue correlate with disease severity. J Med Virol. 1999;59(3):329–34.
- Qin S, Rottman JB, Myers P, Kassam N, Weinblatt M, Loetscher M, et al. The chemokine receptors CXCR3 and CCR5 mark subsets of T cells associated with certain inflammatory reactions. J Clin Invest. 1998;101(4):746–54.
- Hanaoka R, Kasama T, Muramatsu M, Yajima N, Shiozawa F, Miwa Y, et al. A novel mechanism for the regulation of IFN-γ inducible protein-10 expression in rheumatoid arthritis. Arthritis Res Ther. 2003;5(2):R74–81.
- Kuan WP, Tam LS, Wong CK, Ko FW, Li T, Zhu T, et al. CXCL 9 and CXCL 10 as sensitive markers of disease activity in patients with rheumatoid arthritis. J Rheumatol. 2010;37(2):257–64.
- Barros JBS, da Silva PAN, Koga CR, Gonzalez-Dias P, Carmo Filho JR, Nagib PRA, et al. Acute Zika virus infection in an endemic area shows modest proinflammatory systemic immunoactivation and cytokine-symptom associations. Front Immunol. 2018;9:821.
- Zhao L, Huang X, Hong W, Qiu S, Wang J, Yu L, et al. Slow resolution of inflammation in severe adult dengue patients. BMC Infect Dis. 2016;16:291.
Copyright @ 2020 Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are properly cited. For commercial use of this work, please see our terms at http://mji.ui.ac.id/journal/index.php/mji/copyright.
mji.ui.ac.id